AbstractObjectiveMost airway prediction tools only consider anatomical factors. The HEAVEN criteria incorporate both anatomical and physiological elements, but have never been studied in the emergency department. This study aimed to evaluate the association between HEAVEN criteria and intubation difficulty.
MethodsWe conducted a prospective cross-sectional study from April 1, 2020 to January 31, 2021 in the emergency department of a tertiary public hospital. All patients requiring rapid-sequence or delayed-sequence intubation were included. Patients intubated during cardiopulmonary resuscitation were excluded. We enrolled 174 patients. Study endpoints were first pass success and intubation complications.
ResultsThe presence of any HEAVEN criteria was associated with a decrease in the first pass success rate (odds ratio [OR], 0.10; 95% confidence interval [CI], 0.02–0.43; P < 0.01). The anatomical challenge was the only criterion associated with first pass sucess (OR, 0.13; 95% CI, 0.05– 0.29; P < 0.01), whilst other criteria (hypoxemia, extremes of size, vomit/blood/fluid, exsanguination, and neck mobility) were not (P > 0.05). All anatomical factor criteria were associated with difficult airway view (P < 0.05). Intubation complications occurred more in the presence of hypoxemia (OR, 7.44; 95% CI, 2.82–19.63; P < 0.01) and vomit/blood/fluid (OR, 5.55; 95% CI, 2.39–12.92; P < 0.01).
ConclusionAnatomical challenge in HEAVEN criteria can predict first pass success. All anatomical factors in HEAVEN criteria could predict difficult airway view and peri-intubation hypoxemia could be used to anticipate intubation complications. More validation studies are still needed to evaluate the use of HEAVEN criteria as a predictor tool for difficult airway.
INTRODUCTIONEndotracheal intubation is a vital resuscitation skill performed in airway management. Although intubation is common in the emergency department (ED), a difficult airway remains challenging [1]. The current trend places emphasis on first pass successful intubation, as several studies demonstrated more adverse events with repeated intubation attempts [2-4]. Recognizing a difficult airway prepares the providers to improve the chances of first pass successful intubation.
The commonest airway prediction tool is the LEMON score [5]. The modified LEMON score, where “Mallampati” was being excluded as it was not a pragmatic assessment in the ED, was validated subsequently [6-8].
Most airway prediction tools only consider anatomical factors. Physiological factors such as peri-intubation hypotension and hypoxemia were correlated with peri-intubation cardiorespiratory arrest, as evaluated in several studies [9,10]. The risk of a difficult airway in an easy anatomical airway might increase in the presence of shock and hypoxia [11,12]. Four important factors were described; hypoxemia, hypotension, severe metabolic acidosis, and right ventricular failure were noted as elements of the physiologically difficult airway by Mosier et al. [13] The MACOCHA score, a simplified score for identifying patients with difficult intubation in the intensive care unit, has incorporated hypoxemia as one of the factors [14]. However, this score has not been validated in the ED, where intubation is rarely performed by an anesthesiologist, a parameter in MACOCHA.
Davis et al. [15] proposed a difficult airway assessment tool for emergency airway management in 2017, created by a retrospective analysis of rapid-sequence intubation performed by air medical crews requiring more than one attempt. The etiologies with high positive predictive value for airway failure were organized into six categories and the acronym HEAVEN was derived [15]. H for “hypoxemia,” oxygen saturation ≤ 93% at the time of initial laryngoscopy; E for “extremes of size,” meaning a pediatric patient ≤ 8 years of age or clinical obesity; A for “anatomical challenge” which includes trauma, mass, swelling, foreign body, or other structural abnormality limiting laryngoscopic view; V for “vomit/blood/fluid,” clinically significant fluid present in the pharynx/hypopharynx at the time of laryngoscopy; E for “exsanguination,” a suspected anemia that could potentially accelerate desaturation during rapid-sequence intubation associated apnea; and N for “neck mobility,” limited cervical range of motion due to immobilization or arthritis.
A validation study in 2018 retrospectively demonstrated a high negative predictive value of 97% for all HEAVEN criteria, with the exception of “exsanguination.” First attempt successful intubation is inversely related to the total HEAVEN criteria [16]. Another retrospective study in 2019 showed that a more difficult laryngoscopic view and lower intubation success were associated with the presence of HEAVEN criteria [17].
HEAVEN is a concise airway assessment tool incorporating both anatomical and physiological data elements. This study aimed to evaluate the association between HEAVEN criteria and intubation difficulty based on failure at first successful intubation attempt and intubation complications.
METHODSWe conducted a prospective cross-sectional study from April 1, 2020 to January 31, 2021, in the ED of a tertiary public hospital in Malaysia with approximately 300 to 400 attendees daily and 25 to 30 intubations performed weekly. Patients from all age groups requiring rapid-sequence or delayed-sequence intubation were included. Those who required ongoing cardiac resuscitation during intubation were excluded from the research, as were those whose next-of-kin declined to participate. Patients were intubated by clinical staff credentialed for endotracheal intubation following the hospital intubation protocol using either direct or video laryngoscopy. If the first intubation was unsuccessful, the airway providers would either call for help or attempt again depending on the assessment during the intubation process. All patients in this study were successfully intubated within the rapid-sequence or delayed-sequence intubation protocols. None of the patients required rescue or surgical airway. The endotracheal tube was secured after intubation, and patients were monitored for intubation-related complications. Any complications that arose following intubation were managed according to standard practices. A standardized data collection form was used. The form documented the airway provider’s clinical experience, the patient’s demographic profile, and the intubation clinical profile, including the HEAVEN criteria and intubation complications. Details pertaining to the data collection form were explained and clarified by the investigators to all airway providers prior to data collection. The airway providers were credentialed clinical staff from various designations with different backgrounds of training and experience in endotracheal intubation.
Postintubation and stabilization, the study team member (not on clinical duty) assessed the patient for eligibility criteria and approached the next-of-kin for consent if eligible. The next-of-kin was brought to a discussion room and the study was explained to them. Sufficient time up to the entire duration of stay in the ED was allowed for next-of-kin to consider study participation. None of the approached family members refused to consent for the study. Once consented, the airway provider was requested to complete the form before the end of the shift to reduce recall bias. The form was subsequently checked by the study team upon collection. If there was any incomplete data, the airway provider was requested to complete it within the same shift. Completed data were keyed into the software Microsoft Excel (Microsoft Corporation, Redmond, WA, USA) by the investigator and examined by another investigator to minimize data handling bias. The flow chart of data collection is explained in Fig. 1. The study endpoints were first pass success and intubation complications. The sample size was 174, estimated based on the first pass success rate in ED of a tertiary hospital in Malaysia [18], including 10% dropout rate.
Data were statistically analyzed using the SPSS Statistics ver. 17.0 (SPSS Inc., Chicago, IL, USA). Percentages were used for categorical data. The chi-square, Fisher exact test, and odds ratio (OR) were used for variable comparisons. A P-value less than 0.05 was considered to indicate a statistically significant difference.
This study was self-funded. Ethical approval by the Medical Research Ethics Committee was obtained through the National Medical Research Register (NMRR-20-106-52935). Written informed consents were obtained from the patients.
RESULTSMost intubations were performed by medical officers (82.7%). Airway providers with > 3 years of ED experience formed the largest pool (39.7%). Ninety-four airway providers (54%) had 10 to 100 prior experiences of successful intubation. There were more male (74.1%) than female (25.8%) patients. The majority of the intubations were performed using a video laryngoscope (71.3%). Airway providers’ clinical experience, patients’ sex and method of laryngoscopy were not associated with first pass success intubation (P > 0.05). Most intubated patients were categorized under modified Cormack-Lehane (MCL) classification of 1 (39.1%) and 2a (40.8%). A difficult airway view, defined as grades 2b, 3, and 4 in MCL, was documented in 20.1% of patients [19]. Both MCL classification and difficult airway view were found to have a strong association with first pass success (P ≤ 0.01) (Table 1).
First pass success in patients with the presence of any HEAVEN criteria was less likely compared to in those without any HEAVEN criteria (OR, 0.10; 95% CI, 0.02–0.43; P < 0.01) (Table 2). Among the HEAVEN criteria, anatomical challenge was the only criterion strongly associated with first pass success. The odds of first attempt intubation success in the presence of anatomical challenge was 86.8% lower than that in the absence of this criterion (OR, 0.13; 95% CI, 0.05–0.29; P < 0.01). Other HEAVEN criteria (hypoxemia, extremes of size, vomit/blood/fluid, exsanguination, and neck mobility) were not associated with first pass success (P > 0.05) (Table 2).
All anatomical HEAVEN criteria (extremes of size, anatomical challenge, vomit/blood/fluid, and neck mobility) were associated with a difficult airway view. The likelihood of having a difficult airway view was 2.97-fold greater with extremes of size (95% CI, 1.35–6.53; P < 0.01), 4.53-fold with anatomical challenge (95% CI, 1.92–10.75; P < 0.01), 4.65-fold with vomit/blood/fluid (95% CI, 2.13–10.13; P < 0.01) and 3.79-fold with limited neck mobility (95% CI, 1.55–9.25; P < 0.01) (Table 3).
Hypoxemia and vomit/blood/fluid were strongly associated with intubation complications. The OR of intubation complications was 7.44 (95% CI, 2.82–19.63; P < 0.01) with peri-intubation hypoxemia and 5.55 (95% CI, 2.39–12.92; P < 0.01) with vomit/blood/fluid. Although the presence of any HEAVEN criteria was associated with intubation complications (OR, 3.69; 95% CI, 1.33–10.21; P < 0.01), there was no association with parameters such as extremes of size, anatomical challenge, exsanguination, and neck mobility (P > 0.05). The presence of any HEAVEN criteria increased the likelihood of having aspiration 8.56-fold (95% CI, 1.09–67.37; P < 0.05). There was an association between peri-intubation hypoxemia and intubation complications, including dysrhythmia, cardiac arrest, and postintubation hypoxemia. Dysrhythmia occurred 5.84 times (95% CI, 1.21–28.12; P < 0.05) and cardiac arrest 6.53 times (95% CI, 1.61–26.57; P = 0.01) more in the presence of peri-intubation hypoxemia. As expected, peri-intubation hypoxemia increased the risk of postintubation hypoxemia (OR, 42.86; 95% CI, 8.29–221.70; P < 0.01). Similarly, the likelihood of having aspiration in the presence of vomit/blood/fluid was 16.63-fold that without (95% CI, 3.54–78.27; P < 0.01). However, postintubation hypoxemia was not linked with vomit/blood/fluid (P > 0.05), nor was exsanguination (P > 0.05) (Table 4).
DISCUSSIONTo our best knowledge, this is the first prospective study on HEAVEN criteria as a difficult airway assessment tool in the ED. Prior to this, there have been only two retrospective studies on the HEAVEN criteria; both of which were based on data retrieved from the Air Methods Airway Registry in the United States [16,17].
In this study, there was no correlation between the airway providers’ clinical experience, patients’ sex, and method of laryngoscopy with first pass success. The presence of at least one HEAVEN criteria was associated with lower first pass success, consistent with the study by Kuzmack et al. [16] and Nausheen et al. [17]. However, amongst the criteria, only anatomical challenge could significantly predict intubation success. This could also explain the significant association of MCL classification and difficult airway view with first pass success, as these covariates are inter-related with anatomical challenge. Vomit/blood/fluid and neck mobility were not found to be associated with first pass success despite being documented in 29.3% of our patients, contrary to earlier studies [16,17,19,20]. This is probably due to the amount of vomit/blood/fluid found in our study population that was not significant enough to obscure the laryngoscopic view during intubation. However, further studies quantifying and considering the amount of vomit/blood/fluid could further look into the inclusion of this criterion to predict intubation attempts. Similar to Kuzmack et al. [16] but not Nausheen et al. [17], we found that extremes of size had no association with failure of single attempt intubation. This is despite our study having similar weightage to Nausheen et al. [17], wherein it was more represented by the clinically obese rather than patients aged 8 years or less. The clinically obese criteria had some degree of subjectivity to it since it heavily depends on the airway provider’s assessment. A more objective measure incorporating patient’s actual weight could probably facilitate the assessment.
Regarding the physiological factors in HEAVEN criteria, consistent with Kuzmack et al. [16] and Nausheen et al. [17], both hypoxemia and exsanguination were not associated with failure of first attempt intubation. The preceding studies on HEAVEN did not support hypoxemia as a predictor for difficult intubation, contrary to a review article proposing its use [13]. To our knowledge, there has been no prior research establishing the effects of hypoxemia on first attempt intubation success. Perkins et al. [21] highlighted that changes in pulse oximetry did not reliably predict equivalent arterial oxygen saturation levels and tended to overestimate the actual changes. However, peri-intubation hypoxemia increased the risk of experiencing most intubation complications; specifically dysrhythmia, cardiac arrest, and postintubation hypoxemia. This is consistent with the study by Bodily et al. [22], where pre-intubation oxygen saturation of < 93% was found to be associated with oxygen desaturation postintubation. Similar findings by Mort 3 and Heffner et al. [9] were obtained whence peri-intubation hypoxemia was associated with cardiac arrest and dysrhythmia. This significance is nonetheless not seen in considering exsanguination to predict intubation complications in our study. To our knowledge, no previous studies have specifically investigated the association between anemia and first pass success or intubation complications. Furthermore, Perkins et al. [21] documented that anemia does not alter the precision of oxygen saturation measurements in a clinically significant manner. This corresponds to the rationale that suspected anemia would not accelerate desaturation during intubation. The role of anemia as a criterion to assess for a physiologically difficult airway could be further researched.
Our study supports anatomical challenge as an objective factor in the assessment of a difficult airway. Hypoxemia and the presence of vomit/blood/fluid could also be taken into consideration when managing the airway, considering the significant association with intubation complications. Based on our findings, we do not recommend exsanguination as a parameter for predicting difficult airway. Extremes of size and neck mobility as predictive parameters remain inconclusive.
The strengths of this study include the systematic data collection and prior plan to minimize anticipated bias due to its prospective nature. Furthermore, this is the first study on HEAVEN criteria in an ED setting. Due to the robust data collection efforts, there were no missing data in our study. Although all airway providers were credentialed and privileged for airway intubation, there was no additional training provided to standardize the skills. Nonetheless, the background of the airway provider did not affect the outcome of first pass success. This affirms that the data is pragmatic and can be applied to most EDs. However, this study has several limitations. Firstly, it was a single-center study and the sample size was powered to analyze HEAVEN criteria as a whole, but not the breakdown of each component. Since data collection coincided with the COVID-19 pandemic, there were some changes to the intubation norm. Multiple confounders, such as airway provider’s psychological and physical state, use of personal protective equipment, brief usage of an aerosol box during the pandemic, and changes in bag-mask ventilation techniques could have significantly influenced the intubation process, but could not be determined precisely and were not factored in this study [3,9].
In summary, anatomical challenges in the HEAVEN criteria can predict first pass success. All anatomical factors in the HEAVEN criteria could predict difficult airway view and peri-intubation hypoxemia could be used to anticipate intubation complications. More validation studies are still needed to evaluate the use of HEAVEN criteria as a predictor tool for a difficult airway.
ACKNOWLEDGMENTSWe would like to thank Dr. Elaine Chan, Senior Lecturer at the Institute for Research, Development, and Innovation, International Medical University (Malaysia) and Dr. Lim Dwee Wee, Associate Consultant at the Office of Occupational, Environmental, Health, and Safety from Tan Tock Seng Hospital (Singapore) for guidance and statistical support of this study.
REFERENCES1. Dunford JV, Davis DP, Ochs M, Doney M, Hoyt DB. Incidence of transient hypoxia and pulse rate reactivity during paramedic rapid sequence intubation. Ann Emerg Med 2003; 42:721-8.
2. Sakles JC, Chiu S, Mosier J, Walker C, Stolz U. The importance of first pass success when performing orotracheal intubation in the emergency department. Acad Emerg Med 2013; 20:71-8.
3. Mort TC. Emergency tracheal intubation: complications associated with repeated laryngoscopic attempts. Anesth Analg 2004; 99:607-13.
4. Hasegawa K, Shigemitsu K, Hagiwara Y, et al. Association between repeated intubation attempts and adverse events in emergency departments: an analysis of a multicenter prospective observational study. Ann Emerg Med 2012; 60:749-54.
5. Walls RM, Murphy MF. Identification of the difficult and failed airway; Walls RM, Murphy MF. Manual of emergency airway management. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2012. p.8-21.
6. Reed MJ, Dunn MJ, McKeown DW. Can an airway assessment score predict difficulty at intubation in the emergency department? Emerg Med J 2005; 22:99-102.
7. Soyuncu S, Eken C, Cete Y, Bektas F, Akcimen M. Determination of difficult intubation in the ED. Am J Emerg Med 2009; 27:905-10.
8. Hagiwara Y, Watase H, Okamoto H, Goto T, Hasegawa K; Japanese Emergency Medicine Network Investigators. Prospective validation of the modified LEMON criteria to predict difficult intubation in the ED. Am J Emerg Med 2015; 33:1492-6.
9. Heffner AC, Swords DS, Neale MN, Jones AE. Incidence and factors associated with cardiac arrest complicating emergency airway management. Resuscitation 2013; 84:1500-4.
10. Perbet S, De Jong A, Delmas J, et al. Incidence of and risk factors for severe cardiovascular collapse after endotracheal intubation in the ICU: a multicenter observational study. Crit Care 2015; 19:257.
11. Huitink JM, Bouwman RA. The myth of the difficult airway: airway management revisited. Anaesthesia 2015; 70:244-9.
13. Mosier JM, Joshi R, Hypes C, Pacheco G, Valenzuela T, Sakles JC. The physiologically difficult airway. West J Emerg Med 2015; 16:1109-17.
14. De Jong A, Molinari N, Terzi N, et al. Early identification of patients at risk for difficult intubation in the intensive care unit: development and validation of the MACOCHA score in a multicenter cohort study. Am J Respir Crit Care Med 2013; 187:832-9.
15. Davis DP, Olvera DJ. HEAVEN criteria: derivation of a new difficult airway prediction tool. Air Med J 2017; 36:195-7.
16. Kuzmack E, Inglis T, Olvera D, Wolfe A, Seng K, Davis D. A novel difficult-airway prediction tool for emergency airway management: validation of the HEAVEN criteria in a large air medical cohort. J Emerg Med 2018; 54:395-401.
17. Nausheen F, Niknafs NP, MacLean DJ, et al. The HEAVEN criteria predict laryngoscopic view and intubation success for both direct and video laryngoscopy: a cohort analysis. Scand J Trauma Resusc Emerg Med 2019; 27:50.
18. Ahmad R, Rahmat R, Hisamudin N, et al. Demographic and clinical characteristics of red tag patients and their one-week mortality rate from the emergency department of the Hospital Universiti Sains Malaysia. Southeast Asian J Trop Med Public Health 2009; 40:1322-30.
19. Koh LK, Kong CE, Ip-Yam PC. The modified Cormack-Lehane score for the grading of direct laryngoscopy: evaluation in the Asian population. Anaesth Intensive Care 2002; 30:48-51.
20. Joshi R, Hypes CD, Greenberg J, et al. Difficult airway characteristics associated with first-attempt failure at intubation using video laryngoscopy in the intensive care unit. Ann Am Thorac Soc 2017; 14:368-75.
Fig. 1.Flow chart of methodology. RSI, rapid-sequence intubation; DSI, delayed-sequence intubation; ED, emergency department. 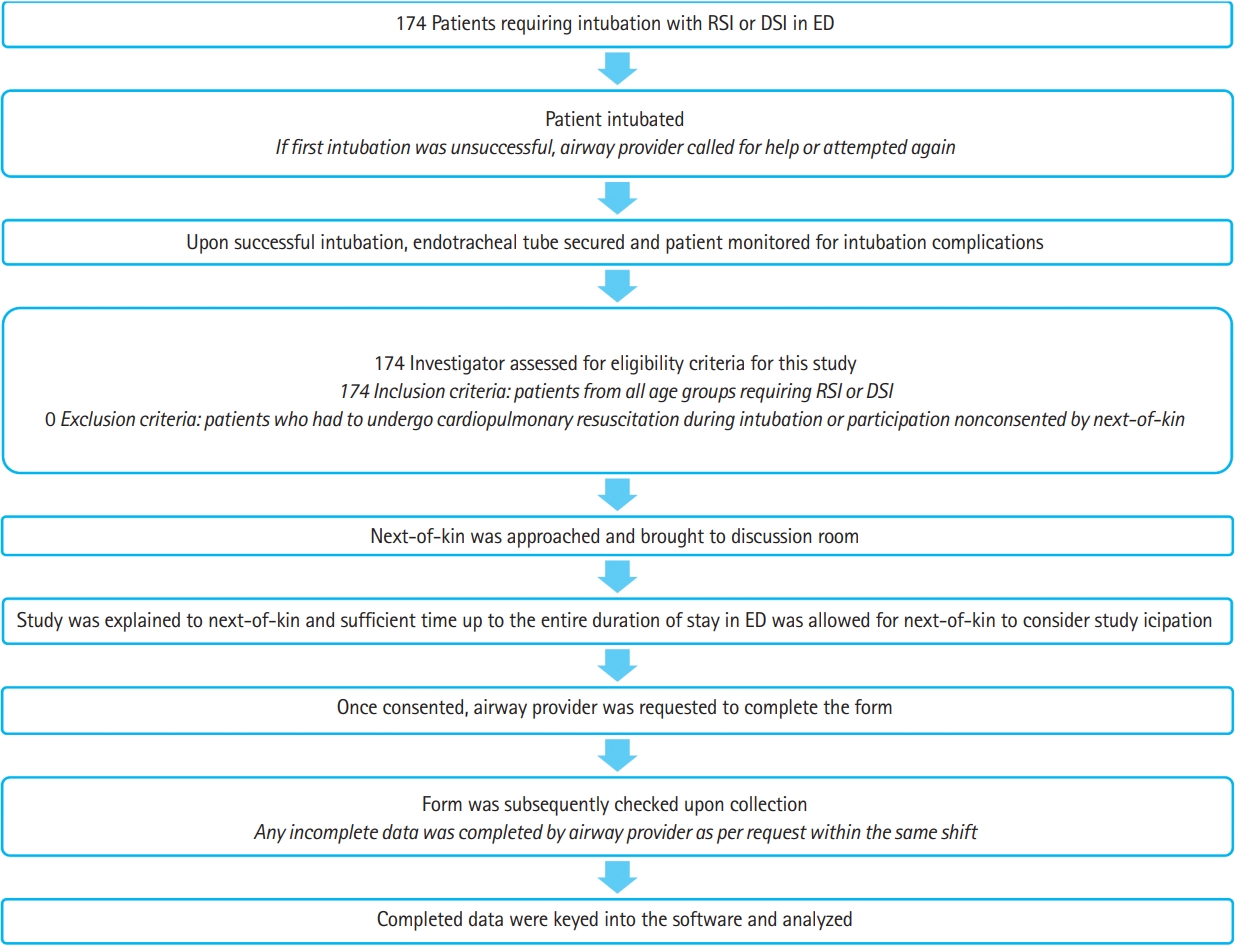
Table 1.Association between the airway providers’ and patients’ parameters with the number of intubation attempts
Table 2.Association between the HEAVEN criteria with the number of intubation attempts
Table 3.Association between the anatomical factors of the HEAVEN criteria and difficult airway view
Table 4.Association between the HEAVEN criteria and the intubation attempt >1, and the complications of intubation
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||