AbstractObjectiveIn 2011, School of Medicine, University of California, Irvine was among the first schools to implement a 4-year ultrasound curriculum. We aimed to find the point-of-care ultrasound (POCUS) utilization pattern among University of California, Irvine alumni.
MethodsWe surveyed University of California, Irvine alumni from the class of 2011 and beyond. Survey questions included POCUS reliance, frequency of use, and comfort with image acquisition and interpretation compared with peers. The primary outcomes were self-reported comfort and reliance on POCUS.
ResultsWe received 93 responses from 624 surveyed alumni (response rate, 14.9%), of which 87 were analyzed. Although 46 respondents (52.9%) reported more reliance on POCUS, three (3.4%) relied on it less than their peers. At the same time, 72 (82.7%) and 67 (77.0%) felt more comfortable than their colleagues in obtaining and interpreting POCUS, respectively. No respondents felt less comfortable obtaining or interpreting POCUS than their peers. The frequency of POCUS use correlated directly with the frequency with which POCUS changed the responder’s case management (rho, 0.860; P<0.001). POCUS reliance also correlated with respondents’ comfort level in obtaining (rho, 0.321; P<0.001) and interpreting (rho, 0.378; P<0.001) POCUS results.
INTRODUCTIONUltrasound was first used as a medical diagnostic tool in the 1930s, and its applications have expanded into 20 medical specialties in the past decade [1–3]. During the past several years, ultrasound technology has advanced, allowing for better resolution and portability and spurring the birth of point-of-care ultrasound (POCUS), which is performed and interpreted in real-time by physicians [3]. This rapidly expanding field has revolutionized medicine by allowing physicians to obtain and interpret images at the bedside, complementing the physical exam and facilitating early diagnosis [3–5]. As the first line of diagnostic imaging worldwide, POCUS has become widely used in most specialities [4]. As ultrasound becomes more prevalent among specialties, residency program requirements are beginning to reflect this clinical change [4,5]. For specialties such as emergency medicine, obstetrics and gynecology (OBGYN), ophthalmology, physical medicine and rehabilitation (PM&R), psychiatry, neurology, radiology, and urology, the Accreditation Council for Graduate Medical Education (ACGME) now requires competency in ultrasound [4–6].
Despite the known benefits of bedside ultrasound in a patient evaluation, the utility of providing ultrasound education for faculty and residents remains a contentious issue within many specialties [5,6]. The increased use of POCUS in different fields and insufficient training warrant a standardized guideline for ultrasound in medical education. This ongoing paradigm shift in imaging and clinical practice has encouraged medical schools nationally to implement a fully integrated ultrasound curriculum [7–11]. Early exposure to ultrasound throughout undergraduate medical education not only augments student understanding of anatomy and physiology through real-life application, but also increases their comfort and competence with the technology [12–14].
The class of 2011 was the first class to have a longitudinal ultrasound curriculum at the University of California, Irvine. The goal of this study was to explore those alumni’s use, comfort, and reliance on ultrasound in their current specialty a few years after graduation.
METHODSUniversity of California, Irvine was one of the first medical schools to implement a 4-year longitudinal ultrasound curriculum. Students watch a minimum of two 30-minute web-based lectures before every session to supplement their preclinical schedule [14]. The 1st year consists of eight hands-on 1-hour sessions and a practical exam to assess student skill levels. A 1:4 ratio of 4th-year medical student instructors to students is maintained for each session, and a simplified list is given to each student at the beginning of class to ensure that all competencies are met [14]. Second-year students receive an additional 11 hours of hands-on ultrasound practice and have an objective structured clinical examination (OSCE) evaluation at the end of the year. By the end of their 2nd year, students are competent in obtaining ultrasounds and identifying pathology in the following systems: cardiovascular, gastrointestinal, genitourinary, respiratory, musculoskeletal, and head and neck. Ultrasound is implemented in 3rd- and 4th-year rotations and OSCEs. An additional 3rd- and 4th-year ultrasound clerkship is offered to students, and it requires a minimum of 75 scans/wk, quality assurance meetings, and participation in Ultrasound Journal Club [14].
We emailed an online voluntary survey to 624 alumni with a graduation date starting in 2011, the first graduating year after the longitudinal ultrasound curriculum was introduced. With 93 responses, we had a response rate of 14.9%. We collected the following data: year of graduation, specialty, reliance on POCUS in practice, frequency of POCUS utilization, and comfort with POCUS image acquisition and interpretation. According to our Institutional Review Board (IRB) guidelines, this study qualified for IRB exemption because no identifying information was collected. There was no risk or minimal risk to subjects for participating in this survey.
We used the Pearson chi-square test to determine differences between categorical variables and Spearman’s rho correlation coefficient to examine associations between ordinal variables. We used the one-sample Kolmogorov-Smirnov test to examine the distribution of the answers and analyzed all data using IBM SPSS ver. 26.0. (IBM Corp).
RESULTSNinety-three responders completed the survey (Table 1). Answers from six psychiatrists were excluded because POCUS has little application in this specialty. Emergency medicine (n=24, 27.6%), OBGYN (n=9, 10.3%), family medicine (n=8, 9.2%), pediatrics (n=7, 8.0%), and anesthesiology (n=6, 6.9%) were the most frequent specialties among the responders. The most frequent POCUS users were practicing in cardiology, pulmonology and critical care, PM&R, emergency medicine, and OBGYN (Fig. 1).
POCUS changed the practice of 70 responders (80.5%) at least once in the 3 months prior to the survey. The practice of responders from emergency medicine changed more frequently than that of other respondents as a result of POCUS exams (P<0.001). The frequency of POCUS changing the responder’s practice during the past three months correlated directly with the frequency of POCUS use (rho, 0.860; P<0.001).
Fig. 2 shows the reliance of responders on POCUS and their perceived comfort in obtaining and interpreting POCUS, compared with their peers in their current specialty. The distribution of answers showed a shift to the right and was not symmetrical (P<0.001). Although 46 responders (52.9%) found their reliance on POCUS to be more or much more than their peers, three (3.4%) relied less or much less on POCUS than peers in their specialty. At the same time, 72 (82.7%) and 67 (77.0%) felt more or much more comfortable than their peers with obtaining and interpreting POCUS, respectively. None of the responders felt less comfortable obtaining or interpreting POCUS than their peers in their current specialty. Reliance on POCUS correlated with the comfort level of the responder in obtaining (rho, 0.321; P<0.001) and interpreting (rho, 0.378, P<0.001) POCUS results.
DISCUSSIONThe results of our study show that University of California, Irvine graduates who underwent a longitudinal 4-year ultrasound curriculum reported higher comfort levels in obtaining and interpreting POCUS than their peers. This comparison was made by the participants themselves in relation to colleagues within their specialty. We also found that reliance on ultrasound correlated with the respondents’ comfort in obtaining and interpreting POCUS results. More than half of our respondents relied on POCUS and felt more comfortable obtaining and interpreting POCUS results than peers in their field. Very few, if any, were less reliant or comfortable than their peers. This suggests that a 4-year longitudinal ultrasound education during medical school would improve reliance on and use of POCUS in residency and beyond.
The number of times POCUS is used per week was heavily affected by what specialty the graduates went on to practice in, with cardiology, pulmonology and critical care, PM&R, and emergency medicine being the highest users of POCUS. These findings are not surprising because these specialties have many more validated applications for POCUS than the specialties lower on the list. We therefore asked respondents to assess their reliance and comfort with POCUS in comparison to peers in their field as a control for the overall differences in baseline POCUS use between specialties. Applications for ultrasound continue to grow each year across most fields of medicine, making familiarity and experience with ultrasound prior to postgraduate training an increasingly valuable skill [15–17]. Additionally, with ultrasound technology continuing to become more portable and affordable, it is expected that POCUS utilization will continue to rise [5,18–20].
A limitation of this study is that our data are inherently subjective because we asked respondents to assess their own reliance and comfort with POCUS relative to their peers. The respondents might vary in their self-awareness and judgment of ability and thus in their ability to accurately compare their own comfort and skill with that of their peers. In short, our data are open to several cognitive biases. One way to address this potential bias could be to include a control group by sending the same survey to physicians who graduated from a medical school without a 4-year ultrasound curriculum and looking for a statistically significant difference in reported comfort with POCUS between the groups. A potential follow-up study could aim to re-create these findings with objective data such as the number of POCUS scans logged or proficiency at POCUS on clinical milestones. This could be feasible if the scope of the study were scaled down to just one specialty, such as emergency medicine, in which it is common practice for residency programs to track the number of POCUS scans performed and include POCUS as part of the assessment for clinical competency.
In conclusion, this study shows that graduates of a 4-year longitudinal medical school ultrasound curriculum reported that they subjectively had higher reliance and comfort with POCUS than their peers in their respective specialties. POCUS is undoubtedly becoming more accessible and widely used across many if not all specialties, which supports the value of incorporating ultrasound into the medical school curriculum.
NOTESAUTHOR CONTRIBUTIONS
Conceptualization: APN, SS, JWR, JCF; Data curation: SS, APN; Formal analysis: SS; Investigation: APN, JCF; Methodology: APN, SS, JCF; Project administration: APN, JCF; Resources: JCF; Supervision: JCF; Validation: APN, SS; Visualization: SS; Writing–original draft: SS, MTN, MD; Writing–review & editing: all authors. All authors read and approved the final manuscript.
REFERENCES1. Sudol-Szopinska I, Martinoli C, Panas-Goworska M. History page: leaders in MSK radiology Karl Dussik, 1908-1968: pioneer of MSK ultrasonography. Semin Musculoskelet Radiol 2021; 25:184-5.
2. Zagzebski J. WE-G-211-03: development of ultrasound imaging equipment. Med Phys 2012; 39(6Part28):3964.
3. Lane N, Lahham S, Joseph L, Bahner DP, Fox JC. Ultrasound in medical education: listening to the echoes of the past to shape a vision for the future. Eur J Trauma Emerg Surg 2015; 41:461-7.
4. Counselman FL, Sanders A, Slovis CM, Danzl D, Binder LS, Perina DG. The status of bedside ultrasonography training in emergency medicine residency programs. Acad Emerg Med 2003; 10:37-42.
5. Leidi A, Rouyer F, Marti C, Reny JL, Grosgurin O. Point of care ultrasonography from the emergency department to the internal medicine ward: current trends and perspectives. Intern Emerg Med 2020; 15:395-408.
6. Shokoohi H, Duggan NM, Adhikari S, Selame LA, Amini R, Blaivas M. Point-of-care ultrasound stewardship. J Am Coll Emerg Physicians Open 2020; 1:1326-31.
7. Nelson BP, Narula S, Argulian E, Bhagra A, Narula J. Including insonation in undergraduate medical school curriculum. Ann Glob Health 2019; 85:135.
8. Dietrich CF, Hoffmann B, Abramowicz J, et al. Medical student ultrasound education: a WFUMB position paper, part I. Ultrasound Med Biol 2019; 45:271-81.
9. Hoffmann B, Blaivas M, Abramowicz J, et al. Medical student ultrasound education, a WFUMB position paper, part II: a consensus statement of ultrasound societies. Med Ultrason 2020; 22:220-9.
10. Rempell JS, Saldana F, DiSalvo D, et al. Pilot point-of-care ultrasound curriculum at Harvard Medical School: early experience. West J Emerg Med 2016; 17:734-40.
11. Phelps A, Wan J, Straus C, Naeger DM, Webb EM. Incorporation of ultrasound education into medical school curricula: survey of directors of medical student education in radiology. Acad Radiol 2016; 23:830-5.
12. Eroglu O, Coskun F. Medical students’ knowledge of ultrasonography: effects of a simulation-based ultrasound training program. Pan Afr Med J 2018; 30:122.
13. Menegozzo CA, Cazolari PG, Novo FD, Colleoni R, Utiyama EM. Prospective analysis of short- and mid-term knowledge retention after a brief ultrasound course for undergraduate medical students. Clinics (Sao Paulo) 2019; 74:e1087.
14. Fox JC, Anderson CL, Ahmed SS, et al. Effect of a medical student emergency ultrasound clerkship on number of emergency department ultrasounds. West J Emerg Med 2010; 11:31-4.
15. Bahner DP, Goldman E, Way D, Royall NA, Liu YT. The state of ultrasound education in U.S. medical schools: results of a national survey. Acad Med 2014; 89:1681-6.
16. Baribeau Y, Sharkey A, Chaudhary O, et al. Handheld point-of-care ultrasound probes: the new generation of POCUS. J Cardiothorac Vasc Anesth 2020; 34:3139-45.
17. Fu JY, Krause C, Krause R, et al. Integration of point-of-care ultrasound training into undergraduate medical curricula: a perspective from medical students. J Med Educ Curric Dev 2016; 3:JMECD.S38240.
18. Dewar ZE, Wu J, Hughes H, et al. A comparison of handheld ultrasound versus traditional ultrasound for acquisition of RUSH views in healthy volunteers. J Am Coll Emerg Physicians Open 2020; 1:1320-5.
Fig. 1.Percentage of responders by specialty in point-of-care ultrasound (POCUS) utilization patterns. The numbers represent the number of responders (n=82, one missing data). 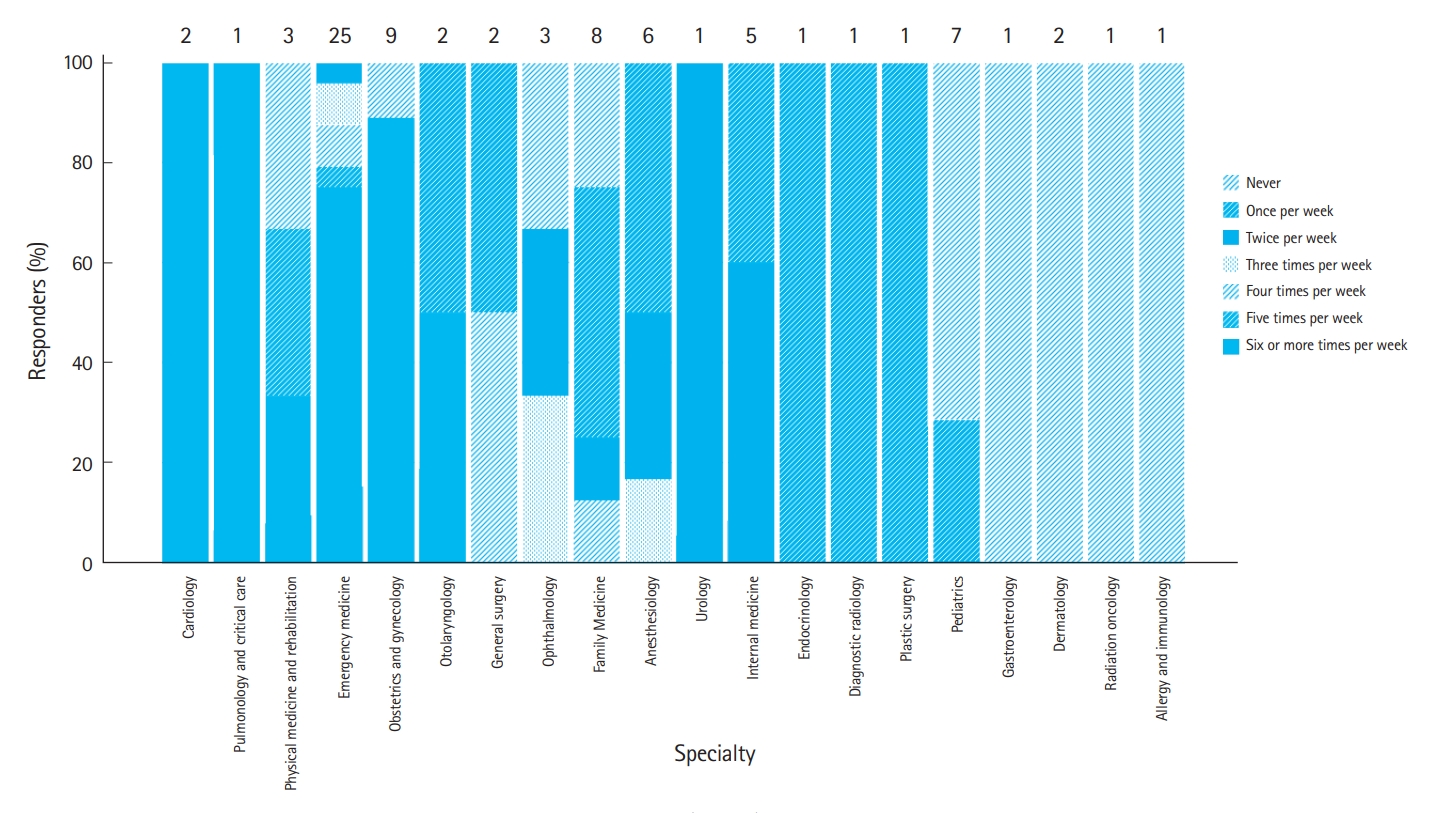
Fig. 2.Percentage of responders’ reliance on point-of-care ultrasound (POCUS) and perceived comfort obtaining and interpreting POCUS, compared with peers in the same specialty. 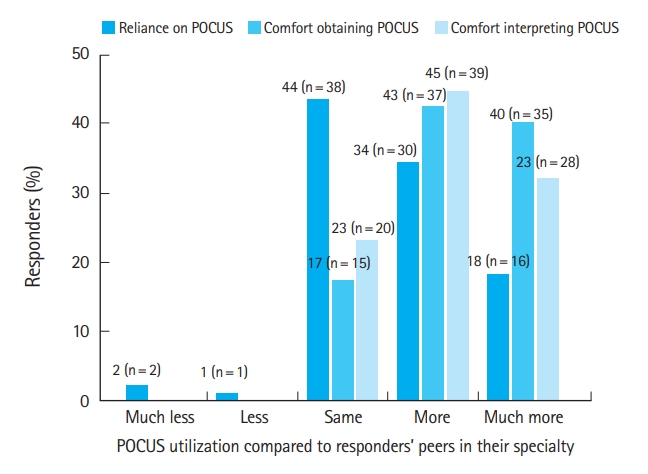
Table 1.Survey questions and distribution of responders’ answers (n=93)
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||