Comparison between an instructor-led course and training using a voice advisory manikin in initial cardiopulmonary resuscitation skill acquisition
Article information
Abstract
Objective
We compared training using a voice advisory manikin (VAM) with an instructor-led (IL) course in terms of acquisition of initial cardiopulmonary resuscitation (CPR) skills, as defined by the 2010 resuscitation guidelines.
Methods
This study was a randomized, controlled, blinded, parallel-group trial. We recruited 82 first-year emergency medical technician students and distributed them randomly into two groups: the IL group (n=41) and the VAM group (n=37). In the IL-group, participants were trained in “single-rescuer, adult CPR” according to the American Heart Association’s Basic Life Support course for healthcare providers. In the VAM group, all subjects received a 20-minute lesson about CPR. After the lesson, each student trained individually with the VAM for 1 hour, receiving real-time feedback. After the training, all subjects were evaluated as they performed basic CPR (30 compressions, 2 ventilations) for 4 minutes.
Results
The proportion of participants with a mean compression depth ≥50 mm was 34.1% in the IL group and 27.0% in the VAM group, and the proportion with a mean compression depth ≥40 mm had increased significantly in both groups compared with ≥50 mm (IL group, 82.9%; VAM group, 86.5%). However, no significant differences were detected between the groups in this regard. The proportion of ventilations of the appropriate volume was relatively low in both groups (IL group, 26.4%; VAM group, 12.5%; P=0.396).
Conclusion
Both methods, the IL training using a practice-while-watching video and the VAM training, facilitated initial CPR skill acquisition, especially in terms of correct chest compression.
INTRODUCTION
Basic life support (BLS) is crucial to patient survival after cardiac arrest: a relatively common condition and a leading cause of death—both inside and outside the hospital. In-hospital cardiac arrest occurs at a frequency of 1 to 5 events per 10,000 hospital admissions, with 15% to 20% of cases discharged alive [1]. Survival rates are increased two- to three-fold when first responders perform adequate cardiopulmonary resuscitation (CPR) [2].
However, the quality of CPR is often suboptimal, even among physicians and nurses trained in CPR [3-7]. Therefore, it is important to educate first responders, and appropriate training is a major concern. In this regard, CPR training methods have improved over the last few decades, having been gradually replaced by practice-oriented methods since the introduction of modern CPR in the 1960s [8]. One of these methods, termed “practice-while-watching” (PWW), minimizes instructor intervention, provides hands-on experience, and focuses on the curriculum. Several studies have reported that basic CPR psychomotor skills are acquired poorly after traditional instructor-led (IL) classes [9-12].
For this reason, many investigations have focused on new training methods, and several recent studies have reported that automated voice advisory manikins (VAMs) increase skill level by providing continuous verbal feedback during individual CPR training without an instructor [3,13-16].
However, most studies of VAM training have assessed participants undergoing CPR skill retraining. Thus, it is unclear whether VAM training is effective for initial acquisition of CPR skills. In addition, most studies have compared VAM with the traditional IL training methods. As mentioned above, more recent IL training methods, such as PWW, emphasize hands-on experience. Therefore, to reliably evaluate the effectiveness of CPR training, VAM training must be compared with IL training that uses the PWW, rather than with traditional IL training. Furthermore, many previous studies have used the 2005 resuscitation guidelines, and it is unknown whether VAM meets the “harder”, “faster”, and “deeper” chest-compression guidelines detailed in the 2010 guidelines.
We compared VAM training with PWW-based IL training in terms of initial CPR skill acquisition, as defined by the 2010 resuscitation guidelines.
METHODS
Study design
This was a randomized, controlled, blinded, parallel-group trial. The design compared PWW-based IL training with VAM training in terms of initial CPR skill acquisition. This study followed the 2010 CPR guidelines, and was approved by our university’s institutional review board. This work was supported by Pusan National University research grant, 2012.
Participants
In March 2014, we recruited first-year emergency medical technician students at the Dong-eui Institute of Technology in South Korea; ultimately, 82 participants were enrolled. All participants provided written consent. The participants had received basic education in CPR (lecture without practice) once or twice before this study, but they had received no formal training and had no certifications. They were distributed randomly into two groups; one group (n=41) received IL training that included PWW (IL group), and the other (n=41) received VAM training (VAM group). However, four participants in the VAM group did not undergo VAM training; thus, the final number of participants in the VAM group was 37.
Study protocol
Training
In the IL group, participants were trained in “single-rescuer, adult CPR” according to the American Heart Association (AHA)’s BLS course for healthcare providers. The participants were assigned at a ratio of four students per BLS-certified instructor and two students per manikin. The IL course lasted a total of 1 hour, which consisted of a 40-minute PWW video followed by 20 minutes of explanation and correction of CPR skills by instructors. The instructors and participants were blinded to the fact that this training was being compared with the VAM training method.
In the VAM group, all subjects received a 20-minute lesson from an advanced life support instructor about the principles of CPR and CPR skills (how to compress and breathe), as described in the 2010 guidelines. After the lesson, the students were informed of when they were scheduled for practice. On schedule, each student trained individually with the VAM (Resusci Anne Skills Station; Laerdal Medical, Stavanger, Norway) for 1 hour, receiving real-time feedback about the compressions and ventilations; other than this feedback from the VAM, no additional instructor intervention or guidance was given to the participants. The VAM course comprised three sections: compressions, ventilation using a pocket mask, and compression/ventilation (30:2). After each section had been completed, the VAM informed the participant whether they passed. If the subjects passed, they could proceed to the next section. If the subjects failed, they repeated the same section or were allowed to choose another section. We recommended that the participants practice all three sections for a total of 1 hour only, even if they had failed to pass a section within that time. If they passed the three sections in less than 1 hour, the VAM course was considered finished, regardless of the time remaining. Only when the students did not pass was the total practice time given as 1 hour.
After the training, all subjects were evaluated as they performed basic CPR according the standard protocol (30 compressions, 2 ventilations) for 4 minutes using a CPR simulator (Resusci Anne Skill Reporter, Laerdal Medical) (Fig. 1). They used their own pocket mask in ventilation.
Measurements
To assess the students’ compression skills, we measured the total number of compressions, the compression rate per minute, the mean compression depth (mm), the proportion of chest compressions that were of appropriate depth (>5 cm), the number and proportion of correct hand positions, the number and proportion of incomplete releases, and the mean hands-off time. In addition, we measured the proportion of participants with a mean compression depth ≥50 mm (2010 guideline) and the proportion of participants with a mean compression depth ≥40 mm (2005 guideline).
To assess the students’ ventilation skills, we measured the total number of ventilations, the mean ventilation volume, and the proportion of ventilations of the appropriate volume (500 to 800 mL). In addition, we measured the proportion of participants with a mean ventilation volume of 500 to 800 mL.
Statistical analysis
All analyses were performed using IBM SPSS Statistics ver. 21 (IBM Corp., Armonk, NY, USA). Categorical data were reported as absolute numbers (with proportions), and the chi-squared test was used to compare groups. Continuous data were reported as medians (with interquartile range), and the Mann-Whitney rank-sum test was used to compare groups; ANCOVA was used to control for confounding variables.
RESULTS
General characteristics
A total of 82 first-year emergency medical technician students were recruited, and 41 subjects were assigned randomly to each group. However, four individuals in the VAM group were excluded because they had not trained using the VAM. The general characteristics of each group are shown in Table 1. Although sex and height differed between the groups, neither of these factors had a significant influence as a confounding variable in the comparison of CPR psychomotor skills between groups (Table 1). None of the subjects had attended any CPR training sessions before the study, besides one or two similar CPR lectures.
Effect of IL training and VAM training methods on chest compression measurements
The proportions of participants with a mean compression depth ≥50 mm was 34.1% in the IL group and 27.0% in the VAM group, while the proportion of students with a mean compression depth ≥40 mm had increased significantly in both groups compared with the proportions of participants with ≥50 mm (82.9% in the IL group and 86.5% in the VAM group). No significant difference was detected between the groups in either regard (Table 2).
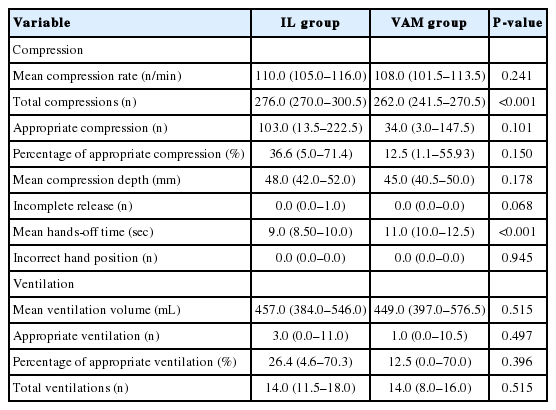
The mean compression depths and proportion of appropriate compressions were higher in the IL group, but neither difference was significant (mean compression depth—IL group 48 mm vs. VAM group 45 mm, P=0.178; proportion of appropriate compressions—IL group 36.6% vs. VAM group 12.5%, P=0.15). The total number of chest compressions was significantly higher in the IL group (IL group 270 vs. VAM group 262, P<0.001). The mean hands-off time was significantly shorter in the IL group (IL group 9 seconds vs. VAM group 11 seconds, P<0.001). No significant differences were detected in any other variables (Table 3).
Effects of IL training and VAM training methods on ventilation measurements
There was no difference in mean ventilation volume between the two groups. The proportion of ventilations of the appropriate volume was relatively low in both groups, and the groups did not differ significantly in this regard (IL group 26.4% vs. VAM group 12.5%, P=0.396). The proportion of participants with a mean volume of 500 to 800 mL was similar in both groups (IL group 34.1% vs. VAM group 29.7%, P=0.378). No significant differences were observed in any other variables (Tables 2, 3).
DISCUSSION
Evidence suggests that IL training may not prepare students adequately to perform CPR skills [17-19], and the VAM has been shown to facilitate adult healthcare providers in acquiring and retaining CPR skills such as chest compression. On the other hand, it has been reported that the VAM method is not superior to the IL-training method with regard to more complex skills like ventilation [12,14,20]. However, most studies in this field have assessed adults who were retraining in CPR; furthermore, few studies used the 2010 CPR guidelines to compare the IL and VAM training methods. Therefore, most previous investigations have assessed the traditional IL training method without PWW. In this study, we compared PWW-based IL training with the VAM training method, using the 2010 CPR guidelines for initial CPR skill acquisition.
In the present study, although the mean compression depths did not satisfy the 2010 guidelines in either group, the depths approached 50 mm in both groups (48 mm in the IL group vs. 45 mm in the VAM group). Nonetheless, the proportion of participants with a mean compression depth ≥50 mm was relatively low in both groups. In the 2005 criteria, a mean compression depth of only ≥40 mm was required; if these criteria had been applied in the present study, both groups would have shown a significantly greater proportion of participants with appropriate mean compression depths (82.9% in the IL group vs. 86.5% in the VAM group). Mpotos et al. [21] combined VAM training with the PWW demonstration video (the so-called SL method) and compared this training with the IL training method. The authors showed that the proportion of participants with a mean compression depth ≥40 mm was similar in each group (70% in the IL group vs. 79% in the SL group). Although effective to some extent, neither training method fully met the 2010 guidelines regarding chest compressions.
The BLS course for initial skill acquisition usually lasts around 4 hours; however, in the present study, we used the AHA’s “single-rescuer, adult CPR” BLS course for healthcare providers. This course lasts a total of 1 hour; therefore, to ensure equity between groups, participants in the VAM group were also allowed one hour training time. This short training time may have been the reason that neither training method fully met the 2010 guidelines. Alternatively, the cause may have been rescuer fatigue. Several studies have suggested that rescuer fatigue leads to inadequate compression rates or depth [22,23], and that significant fatigue and shallow compressions are common after 1 minute of performing CPR. This study assessed the students as they carried out CPR for 4 minutes; therefore, fatigue may have been a factor.
On the other hand, the depths did approach 50 mm, and the proportion of participants with mean compression depths ≥40 mm exceeded 80% in both groups. Therefore, we believe that both training methods are effective for teaching students chest compression skills, but that instruction in these skills requires greater emphasis to meet the 2010 guideline criteria.
Kardong-Edgren et al. [3] compared the HeartCode program with IL training methods. The program functions as follows: after students have learned CPR theory via an individual e-learning course, they undergo CPR training using the VAM. The authors showed that the VAM was superior to IL training. However, the participants in that study had been trained previously, and they were assessed after retraining. It may be that auditory feedback is more helpful to participants familiar with CPR having previous training. Other studies have shown that the VAM is superior to IL training in terms of chest compression [13,15,16,24,25]. However, these studies also assessed participants after retraining.
The hands-off time was shorter, and the total number of chest compressions greater, in the IL group than in the VAM group. Other studies have reported no significant difference between groups in this regard [3,15,24-26]. However, most of these studies used the 2005 CPR guidelines. The 2005 guidelines recommended chest compressions of 38 to 51 mm, whereas the 2010 guidelines recommend ≥50-mm compression depth. Thus, the 2010 guidelines place greater emphasis on chest compressions than the 2005 guidelines. These changes may have encouraged IL instructors to teach deeper compressions, as well as faster return to compressions after ventilation. This shorter hands-off time may have increased the total number of compressions in the IL group. Therefore, IL instruction may result in more appropriate intervention and superior CPR skills. Both mean compression depth and proportion of appropriate compressions were higher in the IL group, although this difference was not significant; it may be that these differences were the result of the changes in the guidelines too. The instructors may have emphasized chest compressions more strongly, resulting in deeper mean compression depth and a greater appropriate compression in the IL group. Conversely, studies using the 2005 guidelines have reported deeper chest compressions and a higher proportion of appropriate compressions in the VAM group [13,15,18,24,25,27].
The percentage of ventilations of adequate volume was relatively low in both groups. Kardong-Edgren et al. [3] showed similar results; indeed, their percentage was low (≤50%) despite adequate volume being defined as 400 to 1,000 mL [23].
Several studies have reported that ventilation is difficult, and people are reluctant to perform it [28-30]. Furthermore, CPR skills (especially in ventilation) decrease over time, and they rapidly deteriorate shortly after training [14,28].
For this reason, neither training method is sufficiently effective for teaching ventilation skills. On a related note, Isbye et al. [24] studied the bag-valve mask in ventilation, and showed that ventilation skill was superior after IL training than after VAM training. These authors suggested that bag-valve mask use is a more complex skill than chest compressions. When learning a complex skill, it is often helpful if the student watches others perform the skill first, and if this observational learning is combined with physical guidance [27].
If combined with additional instructor feedback, VAM training might provide effective training in chest compression skills for first-time learners of CPR; this may reduce the burden on instructors.
Our study had several limitations. Firstly, our sample size may have been too small to detect some effects. Secondly, the quality of the instructor-provided CPR training was not evaluated. However, all instructors had completed the AHA’s BLS instructor course, and had undergone many other BLS courses. For this reason, we believe that the quality of the CPR training was similar. Thirdly, although the participants had not received previous formal CPR training, they had received simple CPR education once or twice before participating in our study. However, because they were first year students, and had not completed a CPR course, we considered all participants as initial CPR students, rather than as experienced paramedical staff undergoing retraining. Finally, the course time differed between the two groups (IL group, 60 minutes; VAM group, maximum 80 minutes). However, as mentioned above, if the students passed three sections, they were permitted to finish the course early in the VAM group; only when they did not pass was the practice time given as 1 hour. Because the finishing time was measured individually without supervisor, we did not know the exact mean practice time. However, we believe that it was similar between the two groups.
In conclusion, even though both the PWW-based IL training and the VAM training methods did not fully meet the 2010 CPR guidelines, both methods were effective for initial CPR skill acquisition, especially for teaching chest compression. However, neither method taught ventilation satisfactorily. Therefore, chest compression should be emphasized more strongly in training, and further studies are required into ventilation skill training.
Notes
No potential conflict of interest relevant to this article was reported.
Acknowledgements
This work was supported by Pusan National University Research Grant, 2012.
References
Article information Continued
Notes
Capsule Summary
What is already known
Automated voice advisory manikins (VAMs) increase skill level by providing continuous verbal feedback during individual cardiopulmonary resuscitation (CPR) training without an instructor. However, most studies of VAM training have assessed participants undergoing CPR skill retraining.
What is new in the current study
Neither instructor-led nor VAM training fully met the 2010 CPR guidelines; nonetheless, both methods facilitated initial CPR skill acquisition, especially in terms of chest compression. However, neither method was satisfactory in teaching ventilation.