Effect of fever or respiratory symptoms on leaving without being seen during the COVID-19 pandemic in South Korea
Article information
Abstract
Objective
Coronavirus disease 2019 (COVID-19) has notably altered the emergency department isolation protocol, imposing stricter requirements on probable infectious disease patients that enter the department. This has caused adverse effects, such as an increased rate of leave without being seen (LWBS). This study describes the effect of fever/respiratory symptoms as the main cause of isolation regarding LWBS after the COVID-19 pandemic.
Methods
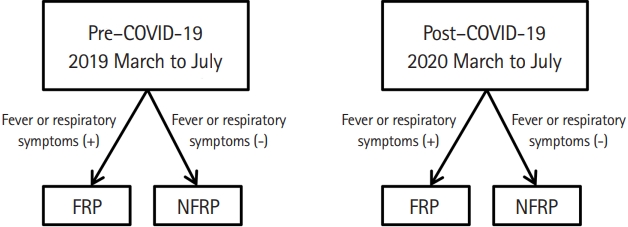
We retrospectively analyzed emergency department visits before (March to July 2019) and after (March to July 2020) the COVID-19 pandemic. Patients were grouped based on existing fever or respiratory symptoms, with the LWBS rate as the primary outcome. Logistic regression analysis was used to identify the risk factors of LWBS. Logistic regression was performed using interaction terminology (fever/respiratory symptom patient [FRP]×post–COVID-19) to determine the interaction between patients with FRPs and the COVID-19 pandemic period.
Results
A total of 60,290 patients were included (34,492 in the pre–COVID-19, and 25,298 in the post–COVID-19 group). The proportion of FRPs decreased significantly after the pandemic (P<0.001), while the LWBS rate in FRPs significantly increased from 2.8% to 19.2% (P<0.001). Both FRPs (odds ratio, 1.76; 95% confidence interval, 1.59–1.84 (P<0.001) and the COVID-19 period (odds ratio, 2.29; 95% confidence interval, 2.15–2.44; P<0.001) were significantly associated with increased LWBS. Additionally, there was a significant interaction between the incidence of LWBS in FRPs and the COVID-19 pandemic period (P<0.001).
Conclusion
The LWBS rate has increased in FRPs after the COVID-19 pandemic; additionally, the effect observed was disproportionate compared with that of nonfever/respiratory symptom patients.
INTRODUCTION
The novel coronavirus disease 2019 (COVID-19) has significantly affected the world. On March 11, 2020, the World Health Organization declared COVID-19 to be pandemic [1]. In response, South Korea implemented various national strategies, such as testing, tracing, and treating (the three Ts), as well as social distancing (internationally considered to be one of the most effective models) [2-4].
Emergency departments (EDs) in South Korea have established institution-level isolation protocols against COVID-19 [5,6]. These protocols necessitate enhanced requirements for probable infectious disease patients entering an ED [7]. consequently causing substantial delays in this critical process [8]. Although the implementation of enhanced isolation procedures in EDs has resulted in adverse effects—such as overcrowding [9] —no studies have described this effect in detail.
Leave without being seen (LWBS) was defined as leaving the ED before consulting a physician after triage. LWBS is one of the factors reflecting the failure of the ED process, long waiting times, and ED overcrowding [10,11]. LWBS results in a higher chance of revisitation, since patients’ problems are often left unresolved [12,13]. Moreover, patients with LWBS who require isolation—i.e., those with a higher likelihood of infection—may seek alternative care options, thereby risking the spread of infection to other health institutions.
The purpose of this study was to describe the effect of fever or respiratory symptoms as the main cause of isolation in patients with LWBS after the COVID-19 pandemic.
METHODS
Ethics statement
This was a retrospective study approved by the institutional review board of the Samsung Medical Center (No. 2020-12-042). Informed consent was waived since the study used only retrospective data.
Study design and setting
This study was conducted in the ED of a tertiary teaching hospital in Seoul, South Korea, with approximately 2,000 inpatient beds. The outpatient department has approximately 2 million visits per year; the annual number of patients in the ED is approximately 80,000.
COVID-19 pandemic in South Korea
Although the first case of COVID-19 in South Korea was confirmed on January 20, 2020, the number of confirmed cases had rapidly increased by the end of February 2020. This was associated with an outbreak in a religious group in the city of Daegu [2,14,15]. Since then, there have been almost 40,000 confirmed cases of COVID-19, with 600 deaths (800 confirmed cases with 11 deaths per 1 million population) occurring during the third wave in December 2020 [16]. As a result, national strategies against COVID-19—such as social distancing—have been adjusted according to the current situation and number of confirmed cases [17].
ED isolation process
The preexisting isolation process was established after the Middle East respiratory syndrome outbreak in 2015 (Fig. 1), where only patients with suspected droplet or airborne infections—such as tuberculosis, chicken pox, measles, mumps, plague, and Middle East respiratory syndrome—were to be isolated. However, the criteria for isolation changed after COVID-19 cases appeared in South Korea; all patients with fever or respiratory symptoms, and a history associated with COVID-19, were to be isolated at the onset of the pandemic. A history associated with COVID-19 included contact with confirmed COVID-19 cases, or traveling to regions with known outbreaks.
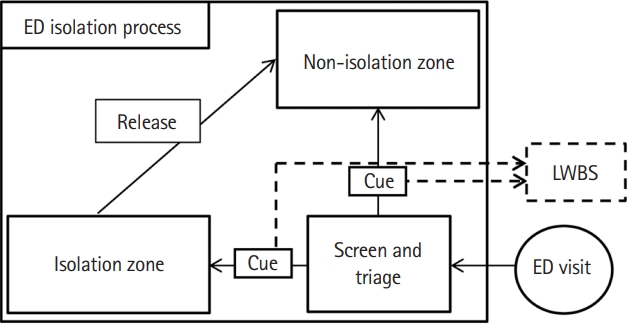
Emergency department (ED) isolation process. Leave without being seen (LWBS) was defined as leaving the ED before encountering a physician after screening and triage. Patients could encounter a physician right after entering medical zones (both isolation and nonisolation zones). Patients remain in queue after screening and triage.
Patients could encounter a physician right after entering medical zones (both isolation and nonisolation zones); as such, LWBS was observed while patients waited to enter the medical zone after screening and triage. In the isolation zone, patients could only undergo basic medical processes, including physical examination, plain chest radiography, blood testing, and electrocardiography; further evaluation via computed tomography, magnetic resonance imaging, and echocardiography was limited. Isolated patients were released following a negative test for COVID-19, or if presumed to be unlikely to have an infection after consulting a physician.
Selection of participants
The study population included all individuals who visited the ED between March and July of 2019 and 2020; nonmedical visits (certificates or prescriptions) were excluded. Revisits were regarded as additional cases, since patients who revisit the ED undergo the same procedures of triage and isolation, regardless of whether or not the chief complaint is the same.
The post–COVID-19 period was defined from March to July 2020, while the comparative pre–COVID-19 period was defined from March to July 2019 (Fig. 2). We categorized patients into two groups according to the presence of fever or respiratory symptoms (e.g., coughing, sputum, rhinorrhea, sore throat, and dyspnea), which represent the major symptoms of COVID-19 [18], and the main cause of isolation. Fever was defined as a body temperature > 37.5°C, which is the isolation criteria used in the center. Fever/respiratory symptom patients (FRPs) were defined as patients with, while nonfever/respiratory symptom patients (NFRPs) were defined as patients without fever or respiratory symptoms (Fig. 2).
Data collection and measurements
We collected the clinical data, ED visits, and discharge-related information from the electronic medical records. Patient information included age, sex, systolic blood pressure, heart rate, respiratory rate, body temperature at arrival, peripheral oxygen saturation, Korean Triage and Acuity Scale (KTAS) score [19], and chief complaint (with or without fever/respiratory symptoms). Discharge information comprised the particulars of ED discharge, including LWBS, discharge to home, death, transfer, and admission. The normal ranges for vital signs were set as follows: systolic blood pressure, 100–160 mmHg; respiratory rate, 12–20 breaths/min; heart rate, 60–100 beats/min; and peripheral oxygen saturation at room air, > 95% [20].
The length of stay (LOS) and bed occupancy rate (BOR) during the pre– and post–COVID-19 periods were also examined. The BOR was defined as the total number of patients in the ED, divided by the number of licensed ED beds [21]. The waiting time (WT) was defined as the time spent outside the medical zone (both isolation and nonisolation) after screening and triage (Fig. 1). For LWBS patients, WT was defined as the time from triage to LWBS; for non-LWBS patients, WT was defined as the time from triage to entering the medical zone. The distribution of LWBS was demonstrated based on WT. Areas are designated for patients to queue and wait before entering the ED—which may contribute to prolonged WT and thus LWBS (Fig. 1).
Outcomes
The primary outcome was LWBS among ED patients, defined as leaving the ED while waiting to enter the medical zone (both isolation and nonisolation) after screening and triage.
Statistical analysis
We used logistic regression analysis to identify the risk factors of LWBS. Risk factors with P-values<0.05 in univariate logistic regression analyses were selected and included in multivariate analysis. After analyzing the effects of the post–COVID-19 period and FRPs on targeted outcomes, the differences in effects on FRPs between the pre– and post–COVID-19 periods were further examined through interaction analysis; logistic regression for the interaction between FRPs and the post–COVID-19 period was performed using interaction terminology (FRP × post–COVID-19).
The WT data was heavily skewed; thus, the Kruskal-Wallis test was performed. The P-values for the WT and LWBS were calculated using the Kruskal-Wallis and chi-squared tests, respectively. Welch two-sample t-test was used to calculate the P-values for LOS and BOR.
All statistical analyses were performed using R statistical software ver. 4.0.3 (R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
Characteristics of study subjects
In total, 34,492 and 25,798 visits were included in the pre–COVID-19 and post–COVID-19 periods, respectively. Table 1 shows the distribution of demographics in patients admitted to the ED; there were significantly fewer young patients (<18 years, P<0.001) than older patients (>18 years, P<0.001) during the post–COVID-19 period. High KTAS scores (4 or 5, less emergent, 55.0%; KTAS 4, 46.3%; KTAS 5, 8.8%) were more frequent than low KTAS scores (1 to 3, 45.0%; KTAS 1, 0.4%; KTAS 2, 5.2%; KTAS 3, 39.4%), and there were significantly fewer FRPs during the post–COVID-19 period (P<0.001); a very small effect size was observed. Both the rate and frequency of LWBS significantly increased during the post–COVID-19 period (P<0.001).
Main results
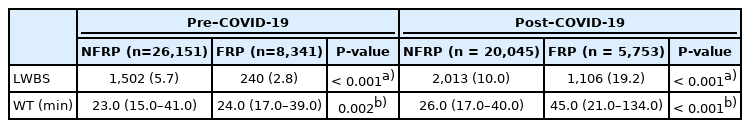
LWBS and WT
There were 240 (2.8%) and 1,106 (19.2%) LWBS cases involving FRPs during the pre–COVID-19 and post–COVID-19 periods, respectively. The median WTs were 24.0 minutes (range, 17.0–39.0 minutes) during the pre–COVID-19 period, and 45.0 minutes (range, 21.0-134.0 minutes) during the post–COVID-19 period (Table 2). Fig. 3 shows the changes in the LWBS rate, as well as the proportion of waiting patients per 10-minute increase in WT. The highest LWBS rate during the post–COVID-19 period was 5.21%, seen after a WT of 20 to 30 minutes. The LWBS rate within 60 minutes was higher during the post–COVID-19 period than the pre–COVID-19 period (Fig. 3).

Rate of leave without being seen (LWBS) and proportion of waiting patients in the emergency department by 10-minute waiting time intervals. The rate of LWBS within 60 minutes was higher in the (A) post–COVID-19 period than in the (B) pre–COVID-19 period. Waiting time was the time from triage to entering the medical zone (both isolation and nonisolation) or LWBS.
Logistic regression
Univariate analysis demonstrated that LWBS in ED patients was significantly related to the proportion of FRPs, post–COVID-19 period, age, high KTAS score, and normal vital signs; sex was not significantly associated with LWBS in ED patients (Table 3). FRPs (odds ratio, 1.76; 95% confidence interval, 1.59–1.84) and the post–COVID-19 period (odds ratio, 2.29; 95% confidence interval, 2.15–2.44) were significantly associated with LWBS. Additionally, LWBS was associated with higher KTAS scores (4 or 5, less emergent) (P<0.001). Age group was also significantly associated with LWBS (P<0.001) (Table 3).
Interaction of FRPs and the post–COVID-19 period
We compared the effect size of FRPs and the post–COVID-19 period on the primary outcome using the interaction term (FRP × post–COVID-19). A significant interaction was observed between FRPs and the post–COVID-19 period regarding the LWBS rate (P<0.001) (Fig. 4).

Differences in the effect of fever/respiratory symptom patients (FRPs) on leave without being seen (LWBS) between the pre– and post– COVID-19 periods. Logistic regression of the primary outcome was performed using interaction terminology (FRP×post–COVID-19). The interaction plot of the COVID-19 group and LWBS is seen. The P-value for the interaction term (FRP×post–COVID-19) according to LWBS was <0.001. NFRP, non-fever/respiratory symptom patient.
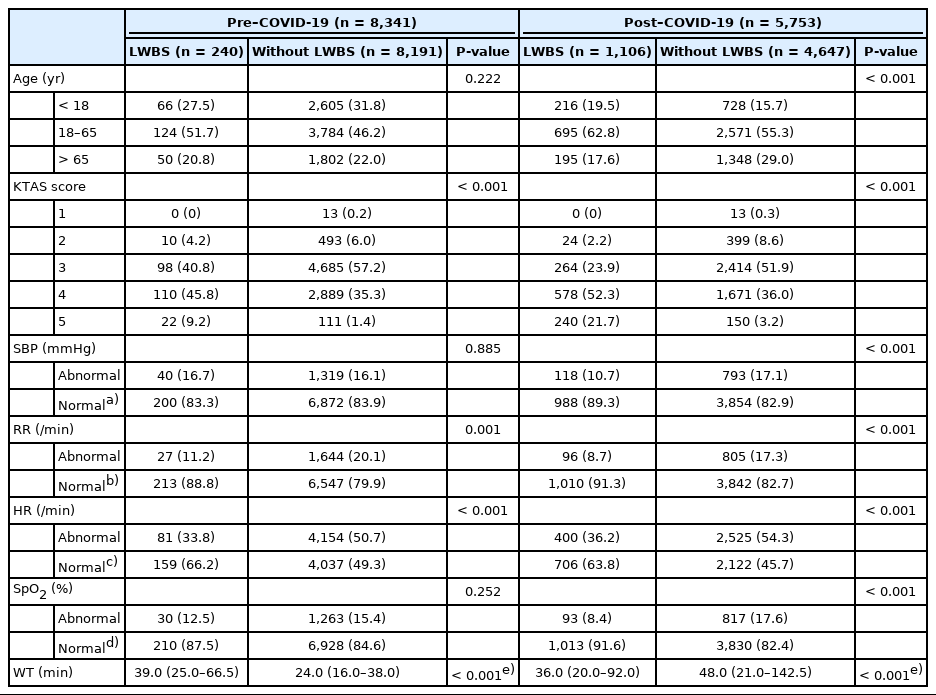
Subanalysis of FRPs
We subanalyzed the differences between FRPs who did and did not LWBS during the pre–/post–COVID-19 periods (Table 4). The proportion of low KTAS scores (4 or 5; less emergent) was higher in FRPs who LWBS during the post–COVID-19 period than in other groups. The median WT was shorter when FRPs did LWBS (36 minutes; range, 20–92 minutes) than when they did not LWBS (48 minutes; range, 21–142.5 minutes) during the post–COVID-19 period (P<0.001). Conversely, the median WT was longer when FRPs did LWBS (39 minutes; range, 25–66.5 minutes) than when they did not LWBS (24 minutes; range, 16–38 minutes) during the pre–COVID-19 period (P<0.001) (Table 4).
ED LOS and BOR
There was a significant decrease in the mean LOS (mean change, 0.42 hours; pre–COVID-19, 7.06 hours; post–COVID-1, 6.64 hours; P<0.001), as well as the mean BOR, during the post–COVID-19 period (mean change, 19%; pre–COVID-19, 66.2%; post–COVID-19, 46.5%; P<0.001).
DISCUSSION
Healthcare and ED systems worldwide—including screening and isolation procedures—have been detrimentally affected by the recent COVID-19 pandemic [22,23]. Changes in these procedures have affected patients visiting the ED [9,24], and although these changes were established to protect vulnerable patients from those with potential infections [25], a substantial proportion of these potentially infected patients are severely ill, requiring urgent care.
This study is the first analysis of LWBS in ED patients after the COVID-19 pandemic, and is similar to a previous study wherein low acuity, young age, and normal vital signs were also found to be associated with LWBS [10]. In particular, FRPs (representing isolated patients) and the post–COVID-19 period were significantly associated with LWBS (Fig. 4). It may be interpreted that FRPs—who may require more urgent medical attention than NFRPs—are forgoing the opportunity to receive medical treatment and visiting other locations in general without appropriate medical consultation. While our efforts to protect other patients have proven successful [25], a considerable proportion of patients may be exposed to unequal medical services and suboptimal care.
Since the WT of FRPs during the post–COVID-19 period was significantly longer than that of other groups, the bottleneck phenomenon at the isolation zone may explain the LWBS findings in this cohort. Our study demonstrated that the number of isolation zones was insufficient when considering the increasing number of isolated patients due to the strict isolation criteria; nevertheless, the total ED volume, LOS, and overcrowding in the ED decreased during the post–COVID-19 period. Redistribution and reallocation of ED resources should be considered to resolve this gridlock, as EDs should protect both FRPs and NFRPs.
Implementing additional resources at a community level for FRPs is not only required in EDs. Regarding infection control, LWBS in patients who require isolation could be more dangerous than in those who do not, as they still have the potential to transmit infection and can thus continue the spread of disease. To monitor FRPs who leave the ED before encountering a physician, a tracking and supervising system is suggested to reduce secondary infections by providing timely alternative testing and treatment options; furthermore, we suggest creating a parallel system for FRPs—such as 24-hour clinics or hospitals—specialized to treat fever. The increase in LWBS rate represents a problem within the public health system, not just hospitals.
The study had several limitations; first, it was limited by its single-center, retrospective design. The isolation process is an institutional-level system that is not standardized according to a national-level strategy; therefore, large multicenter studies should be performed to identify general characteristics and trends of LWBS in the post–COVID-19 era. Still, designing a randomized trial on LWBS is difficult, as we cannot set a control group.
Second, the situation of FRPs in this study may differ from those of isolated patients in the real world. Although the presence of fever or respiratory symptoms is the main cause of isolation after the COVID-19 pandemic, there are many other causes of isolation associated with COVID-19; these include contact confirmed COVID-19 case, or traveling to regions with known outbreaks. However, it is difficult to consider all factors, since they change over time and differ according to the patient’s individual situation.
Third, this study did not describe the patient’s condition after LWBS; therefore, it is difficult to follow-up and predict the prognosis of patients with LWBS, except in the case of revisitation. Although it remains unknown whether LWBS has a poor effect on prognosis, it is evident that these patients do not receive proper medical care. Further research should therefore be conducted regarding the prognosis of patients with LWBS.
In conclusion, the LWBS rate increased in FRPs after the COVID-19 pandemic, and the effect observed was disproportionate compared with that in NFRPs.
Notes
No potential conflict of interest relevant to this article was reported.
References
Article information Continued
Notes
Capsule Summary
What is already known
At post–COVID-19, the isolation processes of emergency departments (EDs) involve enhanced requirements for probable infectious disease patients entering an ED, consequently inducing substantial delays in this critical process. The implementation of enhanced isolation processes in EDs has caused adverse effects such as overcrowding.
What is new in the current study
Leaving without being seen rate has increased post–COVID-19 pandemic. The effect of the pandemic on leave without being seen was more prominent in the patients with fever or respiratory symptoms.