Star in the storm: percutaneous stellate ganglion blockade for drug-refractory electrical storm in the emergency department
Article information
Dear Editor,
Electrical storms are an increasingly common presentation, especially in the developing world, where the incidence of coronary artery disease continues to increase. Prompt resuscitation and emergency care for these patients are critical and can determine whether they survive or not.
We would like to highlight two scenarios where refractory ventricular arrhythmias were successfully treated with ultrasound-guided (USG) stellate ganglion block (SGB). Informed consents for publication of the research details and clinical images were obtained from the patients.
The first was a 68-year-old female patient who presented to the emergency department (ED) with acute-onset palpitations and unresponsiveness for the last 1 hour. She had a history of extensive anterior wall myocardial infarction and had undergone percutaneous coronary intervention 2 years prior. She had a history of similar palpitations in the previous 1 year, for which she received electrical cardioversion. She also had a history of high-grade fever with a cough over the 2 days prior to presentation. Her other comorbidities included hypothyroidism, diabetes mellitus, and hypertension.
On arrival, she was tachycardic with a heart rate of 220 beats/min and without recordable blood pressure. Her electrocardiogram revealed a monomorphic ventricular tachycardia (VT) that was promptly cardioverted at 100 J and returned to a normal sinus rhythm. Hypokalemia and hypomagnesemia were excluded as the triggering etiology on laboratory investigations. She experienced another episode of unstable VT, for which multiple episodes of cardioversion at 200 J failed. She was subsequently treated with amiodarone (bolus and infusion) and propranolol. After no response, the patient was administered intravenous lidocaine 1.5 mg/kg. Over the next 10 minutes, the patient’s dyspnea increased, and she was treated with ventilatory and vasopressor support. She was sedated and paralyzed to decrease sympathetic stimulation. In view of sustained VT that was not electrical or chemical cardioversion, the decision was made to proceed with a bilateral SGB. With ultrasound guidance, approximately 8 mL of 0.2% ropivacaine was placed into the anterior surface of the longus coli muscle at the level of the C6 vertebra by a trained emergency medicine physician (EP) (Fig. 1). Eight minutes after this procedure, the VT subsided and reverted to a regular sinus rhythm.
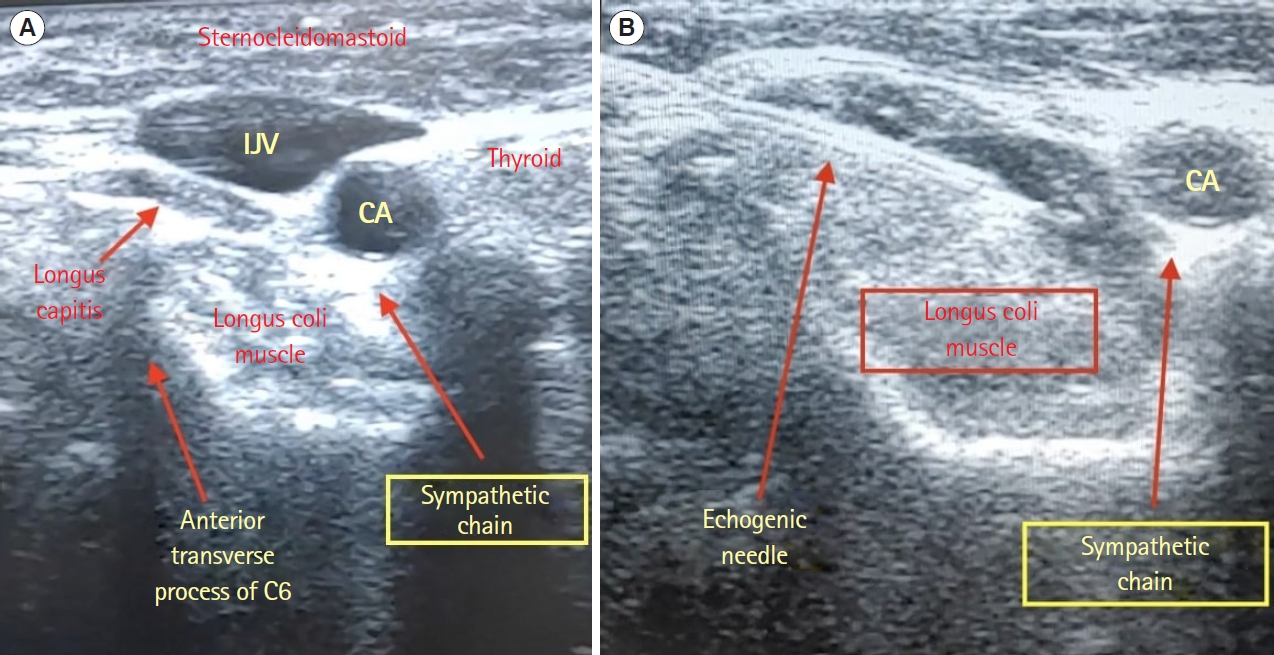
Ultrasound guided stellate ganglion blockade. (A) Ultrasound image obtained at the C6 level injection site for stellate ganglion block prior to injection of local anesthetic. (B) The spread of local anesthetic over the superior surface of the longus coli muscle. An echogenic needle is also visible. IJV, internal jugular vein; CA, carotid artery.
The patient later tested positive for COVID-19 and was shifted to the isolation intensive care unit (ICU) for further care. She experienced no further episodes of VT. However, she progressed to septic shock secondary to pneumonia and passed away.
The second case was that of a 42-year-old diabetic male patient with ischemic cardiomyopathy and an ejection fraction of 35%. The man presented to the ED with chief complaints of chest pain and profuse sweating for the past day. He had a history of coronary artery bypass graft to the left anterior descending and left circumflex arteries 2 years prior. His heart rate was 198 beats/min, and his blood pressure was 90/60 mmHg. His respiration rate was 32 breaths/min, and he had a peripheral oxygen saturation of 88% on room air. Further examination revealed an elevated jugular venous pressure and bilateral crepitations. Cardiac monitoring showed a monomorphic VT, for which he received multiple attempts at synchronized cardioversion, which failed to convert the rhythm. After the second cardioversion, the patient experienced brief episode of ventricular fibrillation, and defibrillation was carried out at 200 J followed by return of a pulse.
Antiarrhythmics of intravenous lidocaine, amiodarone, and metoprolol therapy were also ineffective. The patient was placed in the supine position with the neck extended and the head turned to the right side. Under portable USG, 6 mL of 1% lignocaine was placed anterolaterally into the longus coli muscle by the EP. Gentle pressure was applied to facilitate caudal spread of the anesthetic to reach the C7 to T1 level. Horner syndrome confirmed success of the block. Resolution of VT on the cardiac monitor started at 6 minutes and lasted 8 hours. A repeat episode at that point was successfully converted by electrical cardioversion. The patient was eventually transferred to the ICU for further management, and he remained free of arrhythmia for the remainder of his ICU stay.
Electrical storms (ESs), one of the most lethal of all cardiac arrhythmias, are defined by ≥3 episodes of sustained VT, ventricular fibrillation, or appropriate shocks from an implantable cardioverter defibrillator within 24 hours [1].
ESs are usually associated with undesirably high levels of sympathetic stimulation, which is only worsened by repeated attempts at electrical cardiac resynchronization therapy. The presence of an old infarct and scar tissue leads to increased propensity for electrical instability [2]. ESs are associated with significant morbidity and mortality and often require aggressive treatment to increase chances of survival and recovery [3].
In treatment of ES, simultaneously stabilizing the hemodynamic status and correcting the underlying cause should be prioritized. It is often difficult to identify a specific trigger of ES. It may be precipitated by acute myocardial ischemia, electrolyte disturbances (e.g., hypokalemia, hypomagnesemia, hyperkalemia), worsening heart failure, sepsis, and poor compliance with antiarrhythmic medications [4,5]. Antiarrhythmic medication along with β-blockers (intravenous propranolol) remain the standard treatment for ES, although evidence has shown esmolol also to be effective [6,7].
An SGB was initially considered to address ventricular arrhythmias because most sympathetic innervation to the heart occurs through the postganglionic fibers of the right and left stellate ganglia. Myocardial infarctions may lead to partial denervation of these fibers and paradoxically induce a supersensitivity to catecholamines, increasing heart vulnerability to the electrical induction of ventricular arrhythmias [8]. Sympathetic denervation counteracts this pathological process by reducing the amount of norepinephrine released at the ventricular level and increasing the ventricular fibrillatory threshold [9].
A retrospective study of 30 patients with drug-refractory ES concluded that percutaneous bedside USG SGB is a safe procedure and must be considered to stabilize ventricular arrhythmia [10]. This position was further strengthened by a 2017 systematic review by Meng et al. [11], which concluded that SGB is very effective for acute treatment of ES. Nademanee et al. [2] compared traditional antiarrhythmic therapy to cardiac sympathetic blockade (via SGB) and showed that the latter is far superior in treating ES. This finding has led to the recommendation that SGB always be considered in cases of drug-resistant electrical storm.
A variety of other therapies (including neuromodulation with thoracic epidural anesthesia, spinal cord stimulation, or cardiac sympathetic denervation) can also yield a curative effect in certain situations when standard treatments are inefficacious [5]. However, these procedures are often beyond the scope of services available in an ED. SGBs were traditionally performed by anesthesiologists and pain management specialists across the country. With the advent of EPs trained in USG blocks, the role of peripheral nerve blocks in the ED is increasing beyond the typical use in pain management. Thorough knowledge of neck anatomy, appropriate needle tracking, and steady hand-eye coordination coupled with regular practice provide a short learning curve for these relatively safe and life-saving procedures [12].
The authors would like to highlight the need for recognition of alternative treatment modalities such as SGB, which may be potent additions to the EP toolbox in management of drug-refractory ventricular arrhythmias. USG SGB is a step toward minimally invasive resuscitation that can be performed at the bedside by trained EPs to reduce the ventricular arrhythmia burden in an acute stage.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
FUNDING
None.
AUTHOR CONTRIBUTIONS
Conceptualization: SB; Formal analysis: all authors; Writing–original draft: all authors; Writing–review & editing: all authors. All authors read and approved the final manuscript.
