Targeted temperature management with hypothermia for comatose patients after cardiac arrest
Article information
Abstract
Targeted temperature management with mild hypothermia (TTM-hypothermia; 32–34 °C) is a treatment strategy for adult patients who are comatose after cardiac arrest. Robust preclinical data support the beneficial effects of hypothermia beginning within 4 hours of reperfusion and maintained during the several days of postreperfusion brain dysregulation. TTM-hypothermia increased survival and functional recovery after adult cardiac arrest in several trials and in realworld implementation studies. TTM-hypothermia also benefits neonates with hypoxic-ischemic brain injury. However, larger and methodologically more rigorous adult trials do not detect benefit. Reasons for inconsistency of adult trials include the difficulty delivering differential treatment between randomized groups within 4 hours and the use of shorter durations of treatment. Furthermore, adult trials enrolled populations that vary in illness severity and brain injury, with individual trials enriched for higher or lower illness severity. There are interactions between illness severity and treatment effect. Current data indicate that TTM-hypothermia implemented quickly for adult patients after cardiac arrest, may benefit select patients at risk of severe brain injury but not benefit other patients. More data are needed on how to identify treatment-responsive patients and on how to titrate the timing and duration of TTM-hypothermia.
INTRODUCTION
For a patient who is comatose after cardiac arrest, clinicians must immediately decide whether or not to manipulate temperature and whether to specifically target a lower-than-normal body temperature. Targeted temperature management with mild hypothermia (TTM-hypothermia) is a strategy in which treatment includes lowering the patient core temperature to 32 to 34 °C for a period of time, typically 24 hours in adults. The use of TTM-hypothermia has been supported by international guidelines since 2003 [1–4]. There is extensive preclinical data supporting the biological plausibility of a beneficial effect of TTM-hypothermia [5,6]. Multiple systematic reviews have summarized the clinical evidence for using TTM-hypothermia versus normothermia in cardiac arrest [7,8].
This review synthesizes the current understanding of TTM-hypothermia as a tool for treating adult cardiac arrest. First, laboratory data describe that the effective therapeutic window for TTMhypothermia probably is within 4 hours of return of spontaneous circulation (ROSC), with declining benefit later. Second, many plausible physiological mechanisms may mediate beneficial effects of TTM-hypothermia on neurological recovery, but few cardiac arrest trials measure these mediators. Third, some clinical studies in adults, children, and neonates support use of TTM-hypothermia in certain populations. Fourth, larger clinical trials in more heterogenous populations fail to detect any benefit from TTM-hypothermia, though all trials based on current practice barely achieve differential treatment of groups within 4 hours. Fifth, clinical studies suggest that TTM-hypothermia might have benefit for selected adult patients even if there is no detectable benefit for heterogenous groups of patients. Future clinical research must consider whether TTM-hypothermia is implemented within the therapeutic window and whether the enrolled patient population includes individuals likely to benefit from TTM-hypothermia.
PRECLINICAL DATA ON TIMING FOR TTM-HYPOTHERMIA
It is well-established that lowering the temperature of the brain as much as possible prior to ischemia will protect the brain from injury (Fig. 1) [8]. By reducing metabolic rate, this protective hypothermia reduces demand for oxygen and substrate thereby prolonging tolerance to interruption in supply [9]. However, protective hypothermia is only practical in clinical situations where ischemia is anticipated, such as during surgery requiring circulatory arrest [10]. Protective hypothermia is clinically relevant for treating adult cardiac arrest patients who may have been hypothermic prior to cardiac arrest: these patients have much higher chance of survival and recovery even after prolonged cardiac arrest [11].
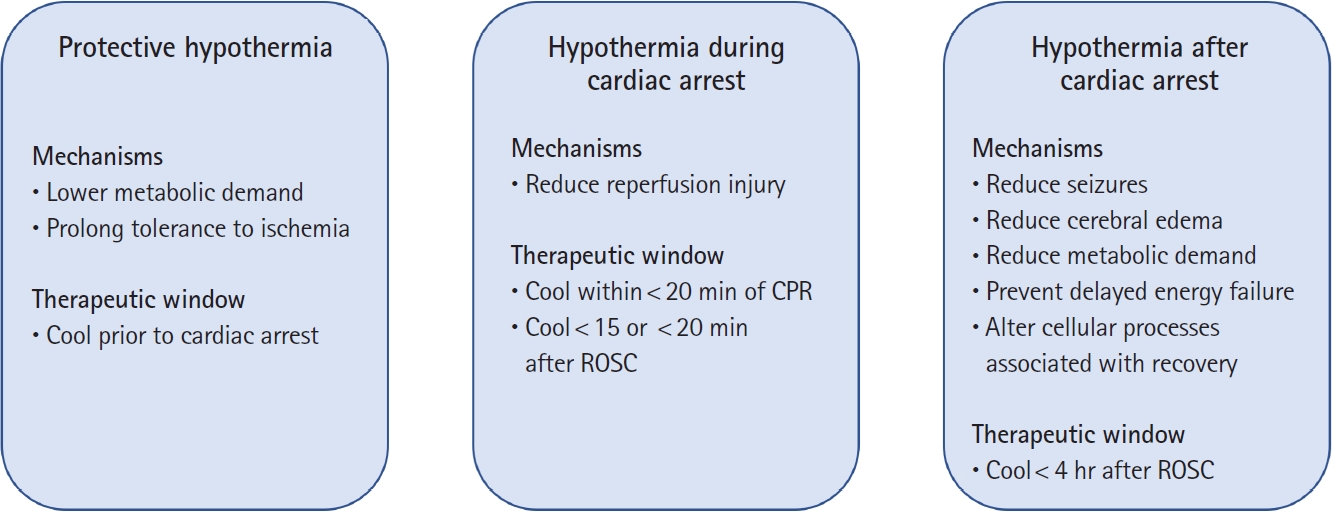
Targeted temperature management with mild hypothermia can benefit ischemic brain injury in different ways, depending on when it is delivered. Specifically, hypothermia can protect from brain injury, reduce reperfusion injury, or treat secondary brain injury. CPR, cardiopulmonary resuscitation; ROSC, return of spontaneous circulation.
Induced mild hypothermia (32 to 35 °C) after ischemia also reduces final brain injury after global ischemia in multiple animal species (Fig. 1) [5,6]. Unlike protective hypothermia, deleterious effects of postischemia hypothermia increase for temperatures less than 30 °C without any additional neurological benefit [12]. Hypothermia should begin as soon as possible during or after reperfusion [13,14].
Postischemia hypothermia treatment has two targets with two different therapeutic windows: (1) reducing the immediate reperfusion injury and (2) reducing secondary brain injury (Fig. 1). Treating reperfusion injury requires hypothermia immediately within minutes during the reperfusion of previously ischemic brain and is effective even if the duration of hypothermia is brief [13–15]. Even 1 hour of TTM-hypothermia improves brain recovery, but delays longer than 15 minutes [13] or 20 minutes [14] after ROSC reduce any benefit. Furthermore, initiating hypothermia after 20 minutes of cardiopulmonary resuscitation (CPR) is less effective than after 10 minutes of CPR [15]. Hypothermia to treat reperfusion injury has prompted clinical studies of intra-arrest cooling. While rapid reductions in temperature are possible in small animals, technical challenges remain for delivering this intervention to patients [16–18].
Treating secondary brain injury requires manipulation of temperature over the hours and days after reperfusion when the brain is vulnerable. Too brief hypothermia (<5 hours) does not afford any detectable benefit [19,20] and durable benefit after global brain ischemia or hypoxia may require 48 hours or more of treatment [21,22].
Beneficial effects of prolonged TTM-hypothermia on behavioral outcomes and survival are reliable when hypothermia starts within 4 hours after reperfusion but not when treatments differ at 8 hours after reperfusion (Fig. 2) [19,23]. Likewise, histological signs of brain damage are reduced in all brain areas when TTM-hypothermia groups have different temperatures by 2 hours after reperfusion but not in the striatum when TTM-hypothermia is delayed for 6 hours nor in parts of the hippocampus when delayed for 12 hours [19,23]. Because this time window for initiating treatment is more easily achieved in adult humans, most clinical research has focused on TTM-hypothermia for treating secondary brain injury after cardiac arrest [24–29].
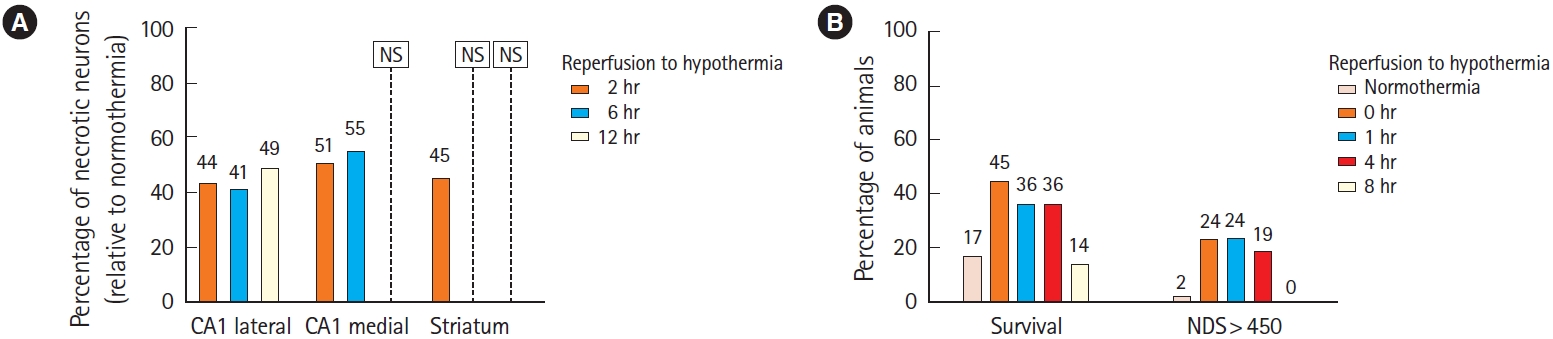
Preclinical data [19,23] illustrate that a 4-hour delay allows for treating ischemic brain injury with prolonged postischemia targeted temperature management with mild hypothermia but this benefit declines with 6- to 8-hour delay. (A) Histological protection of striatum (lower percentage of necrotic neurons) is present when hypothermia starts within 2 hours, but not after 6 hours. Protection of the medial CA1 region of the hippocampus decreases at 6 hours and is not detected at 12 hours [19]. (B) Survival after cardiac arrest increases when hypothermia starts 0 to 4 hours after cardiac arrest but declines with 8-hour delay. Behavioral recovery vanishes with 8-hour delay. [23]. NS, not significant; NDS, neurological deficit score (higher NDS is more favorable).
Thus, under ideal laboratory conditions with tight control over other treatments and with homogenous injury severities, TTM-hypothermia reliably reduces brain injury when experimental groups have different temperatures by 4 hours or less after reperfusion, and benefits increase with durations of TTM-hypothermia beyond 24 hours.
POTENTIAL MECHANISMS FOR BENEFICIAL EFFECTS OF TTM-HYPOTHERMIA
Experimental data do not identify a single mechanism mediating the beneficial effects of TTM-hypothermia on secondary brain injury. Temperature affects multiple pathophysiological processes that might influence brain recovery. Hypothermia attenuates many processes that are associated with brain injury but also stimulates other reparative processes. Experimental studies rarely determine whether or not these associated pathophysiological changes are in the causal pathway for the beneficial effects of lower temperature. Examples of pathophysiological processes that are influenced by temperature manipulation include seizures, brain edema, metabolic rate, and molecular processes.
Seizures and nonconvulsive status epilepticus occur frequently after cardiac arrest and are associated with worse outcomes [30,31]. Temperature is positively correlated with seizure frequency in animal models [32,33] and fever or increased temperature is a well-known trigger of seizures in humans [34]. Based on these observations, hypothermia has been used to treat refractory seizures, though supporting clinical evidence is compromised by mostly uncontrolled case series [35]. In a controlled clinical trial for patients with refractory seizures not resulting from cardiac arrest, TTM-hypothermia did reduce seizure duration and progression to persistent electroencephalography (EEG)-confirmed status epilepticus by 6 to 12 hours [36]. Induced hypothermia does reduce epileptiform discharges in posthypoxic sheep [37].
Cerebral edema and intracranial hypertension occur over the first few days after cardiac arrest [38–40], and radiographically apparent cerebral edema after cardiac arrest is associated with worse outcomes or even herniation and neurological death [41,42]. Hypothermia has been used to treat intracranial hypertension after traumatic brain injury [43,44] and other conditions [45,46]. Observational data confirm that intracranial pressure increases, sometimes to lethal levels, during rewarming after TTM-hypothermia in cardiac arrest patients [38]. Experimental data in animals demonstrate that TTM-hypothermia can reduce intracranial hypertension after reperfusion [47].
Metabolic demand exceeding substrate delivery adds to secondary brain injury. Episodes of hypotension, hypoxemia, or recurrent cardiac arrest occur in some patients during the first hours after cardiac arrest, and these episodes are associated with worse recovery [48,49]. Even without major clinical events, cerebral perfusion is impaired during the first 24 hours after an ischemic insult, and this impairment is associated with increased cerebral lactate production [50,51]. Decreased brain energy utilization of about 5% per °C may help the brain to tolerate secondary hypotensive, hypoxemic, or hypoperfusion insults [47,52].
Perhaps related to cerebral metabolic rate, delayed failure of brain energy utilization and increased cerebral lactate levels are apparent 1 to 2 days after insult in animals with poor outcome [49], and similar failure of cerebral energy utilization appears days after cardiac arrest in humans with poor outcome [53,54]. In some animal models, TTM-hypothermia prevents the failure of energy utilization that begins at 4 hours and peaks at 12 to 24 hours after reperfusion [50,55].
Potentially beneficial molecular and cellular processes are promoted by TTM-hypothermia. For example, patterns of gene expression differ between brains of animals during treatment with TTM-hypothermia [56], including increased expression of neurotrophic factors that are associated with reparative processes [57,58]. TTM-hypothermia induces activation of specific intracellular signaling pathways [59], alters brain microgliosis [60], and inhibits apoptotic cell death pathways in brain [61].
Thus, TTM-hypothermia has multiple plausible mechanisms whereby it may improve brain recovery after cardiac arrest, and many of these processes are associated with outcome for cardiac arrest patients. Regrettably, clinical trials of TTM-hypothermia rarely measure any of these pathophysiological mechanisms.
ADULT TRIALS DETECTING BENEFIT FROM TTM-HYPOTHERMIA
Several clinical trials support the use of TTM-hypothermia for adult cardiac arrest [24,25,62]. In one trial, 275 out-of-hospital cardiac arrest (OHCA) patients were assigned to TTM-hypothermia (32–34 °C, n=137) or usual temperature care (n=138) for 24 hours, followed by passive rewarming over approximately 8 hours [24]. TTM was initiated at a median of 105 minutes after ROSC, and temperatures differed between groups by 4 hours after ROSC. Patients reached target temperature a median of 8 hours (interquartile range [IQR], 4–16 hours) after ROSC. TTM-hypothermia patients had higher survival (59% vs. 45%) and favorable functional status at hospital discharge (55% vs. 39%)
The second trial assigned 77 OHCA patients to TTM-hypothermia (33 °C, n=43) or usual care (n=34) for 12 hours followed by rewarming over 6 hours (0.7 °C/hr) [25]. In this trial, temperatures differed between groups by 120 minutes after ROSC, and TTM-hypothermia patients had a mean temperature 33.3 °C by the time of intensive care unit (ICU) admission. TTM-hypothermia patients had higher survival (49% vs. 32%) and normal-minimal disability at hospital discharge (35% vs. 21%).
Both of these trials focused on very select patients with OHCA that included shockable cardiac rhythms. This is a population with a more favorable prognosis compared to the entire population of cardiac arrest patients but represented only about 8% of all screened patients in one trial [24]. In addition, both trials compared TTM-hypothermia to usual care, and usual care permitted fever for many patients. Finally, both trials were efficacy proof-of-concept trials at single centers that could not be blinded, stopped early for logistical reasons, did not regiment decisions on withdrawal of life sustaining treatments (WLST), and may have had other unmeasured sources of bias. These methodological limitations, along with the relatively small total number of patients randomized, raised concerns about the reproducibility of the findings [63].
The more recent HYPERION (Therapeutic Hypothermia after Cardiac Arrest in Nonshockable Rhythm) trial specifically examined the treatment effect for TTM-hypothermia in patients after either OHCA or in-hospital cardiac arrest (IHCA) with nonshockable rhythms [62]. Investigators randomly assigned 584 patients to TTM-hypothermia (33 °C) or normothermia (36.5–37.5 °C) for 24 hours followed by rewarming at 0.25 to 0.5 °C/hr. Median time from ROSC to randomization for TTM-hypothermia was 232.5 minutes (IQR, 178–276.5 minutes). The goal of 33±0.5 °C was obtained a median of 317 minutes (IQR, 214–477 minutes) after randomization. TTM-hypothermia patients had higher rates of favorable functional recovery (10.2% vs. 5.7%), though survival was not reliably different (19.7% vs. 16.8%).
One trial compared 24 hours versus 48 hours of TTM-hypothermia in adult OHCA. This trial randomly assigned 351 patients resuscitated from OHCA to 24 hours (n=176) or 48 hours (n=175) of TTM-hypothermia (33 °C), followed by rewarming at 0.5 °C/hr [29]. Target temperature was achieved a median of 281minutes (IQR, 217–360 minutes) after ROSC for the 48-hour group and 320 minutes (IQR, 241–404 minutes) after ROSC for the 24-hour group. Favorable functional recovery (69% vs. 64%) and survival (73% vs. 66%) at 6 months were numerically higher for the 48-hour group but differed less than the 15% absolute difference the trial could detect.
ADULT TRIALS DETECTING NO BENEFIT FROM TTM-HYPOTHERMIA
Subsequent clinical trials in adults improved many methodological flaws in the original studies supporting TTM-hypothermia. Particular attention was placed on rigorous randomization, obtaining a complete larger multicenter cohort, and regimenting decisions about WLST.
In the TTM Trial, 939 OHCA patients were randomly assigned to TTM-hypothermia (33 °C, n=473) or near-normal temperature control (TTM-36 °C; n=466) for 28 hours, followed by controlled rewarming at 0.5 °C/hr [26]. Temperatures differed between groups by 3 to 5 hours after randomization, but randomization was allowed up to 4 hours after ROSC. The time from ROSC until groups differed in temperature treatment is not clear. WLST was discouraged prior to 72 hours, and prognostic assessments were provided after 72 hours by a clinician blinded to treatment and using established criteria. TTM-hypothermia and TTM-36 °C patients had similar survival (50% vs. 52%) and good functional recovery at 180 days (46% vs. 48%).
In the TTM2 Trial, 1,861 OHCA patients were randomly assigned to TTM-hypothermia (33 °C, n=930) or to active fever prevention (n=931) for 28 hours, followed by controlled rewarming at 0.5 °C/hr [27]. Median time from ROSC until randomization was 136 minutes (IQR, 103–170 minutes) for TTM-hypothermia, and this group reached ≤34 °C at a median of 3 hours after randomization. Temperatures in treatment groups were separated by 4 to 5 hours after randomization. Again, WLST was regimented and measured. TTM-hypothermia and fever prevention patients had similar survival at 6 months (50% vs. 52%) and good functional recovery at 180 days (45% vs. 45%).
In a trial examining hypothermia for IHCA patients, 242 patients were randomly assigned to TTM-hypothermia (n=123) or normothermia (n=119) for 24 hours followed by controlled rewarming at 0.25 °C/hr [28]. Mean±standard deviation time from randomization to a temperature<34 °C was 4.2±2.8 hours, with mean±standard deviation time from arrest to intervention of 2.2±1.3 hours. Temperatures were separated by 3 to 4 hours after beginning the intervention. TTM-hypothermia patients had similar 6-month survival (27% vs. 29%) and favorable functional recovery (23% vs. 24%).
A few questions remain about these trials. First, was the intervention applied quickly enough? TTM-hypothermia used in the recent trials represented contemporary clinical practice in Europe, but many patients had TTM regimens selected upon ICU admission rather than during initial emergency care [26–28]. Thus, treatment groups may not have had robustly different temperatures for 5 to 6 hours after ROSC. This is longer than the 4 hours therapeutic window for efficacy of hypothermia in animal studies [19,23] and longer than the delay in the original efficacy trials [23,24].
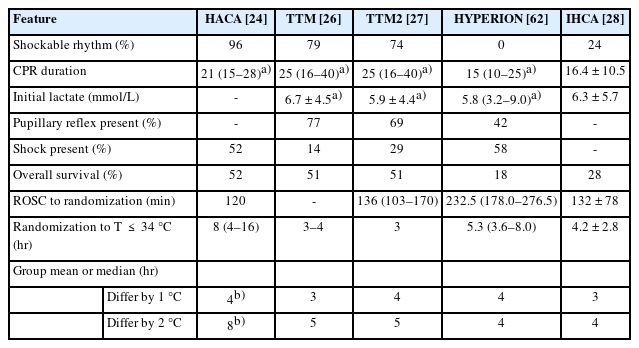
Second, are the enrolled patients representative of all cardiac arrest patients (Table 1) [24,26–28,62]? TTM and TTM2 included patients with presumed cardiac cause of cardiac arrest and excluded patients resuscitated from unwitnessed asystole. These criteria resulted in a very “cardiac” cohort with shockable rhythms in 79% [26] and 74% [27], respectively, and with ST elevation myocardial infarction in 41% [26] and 41% [27], respectively. This is a very important group of OHCA patients, and perhaps represents the group from which the largest proportion of survivors arise. However, randomized cohorts exclude many patients encountered at most clinical centers, for whom clinicians also must decide on TTM treatment.
TTM-HYPOTHERMIA IN NEONATES AND CHILDREN
Use of TTM-hypothermia in adult cardiac arrest is also informed by clinical studies in children and neonates. Extrapolation from children to adults should recognize that therapeutic effects may differ in the developing brain relative to the adult brain. Also, the underlying insult leading to cardiac arrest may be quite different between these populations. Regardless, cardiac arrest in children and hypoxic-ischemic brain injury in neonates provide opportunity to test the efficacy of TTM-hypothermia for improving brain recovery after global hypoxia-ischemia.
The clinical evidence for use of TTM-hypothermia after hypoxic-ischemic brain injury (HIBI) in neonates is very robust. A recent systematic review identified 28 randomized trials enrolling neonates who underwent TTM-hypothermia (n=1,832) or normothermia (n=1,760) [64]. Survival was higher for TTM-hypothermia infants (74% vs. 63%) with similar results across several subgroups and methods of cooling.
There are several key differences between the clinical use of TTM-hypothermia in neonates and adults. First, the initiation of treatment for HIBI is sooner than usual for adult cardiac arrest. Most trials enroll neonates with HIBI within 6 hours of birth and as soon as possible [64]. Because neonates have a large body surface area relative to body volume, rapid control of temperature is much easier than in adult cardiac arrest. Thus, delays in achieving separation of treatment groups were not an issue in clinical trials. Secondly, clinicians treat HIBI with TTM-hypothermia for 72 hours. This longer duration of treatment spans more of the time period when seizures, cerebral edema, and other clinical sequelae of brain ischemia are expected. Finally, determining outcomes after HIBI in neonates is less often confounded by WLST as it is in adults.
Differential treatment of children after cardiac arrest was less rapid in two concurrent multicenter THAPCA (Therapeutic Hypothermia After Pediatric Cardiac Arrest) trials testing TTM-hypothermia for OHCA and IHCA [65,66]. These trials assigned children to TTM-hypothermia (33 °C) or normothermia for 48 hours followed by rewarming at ≤0.25 °C/hr. In THAPCA-IHCA, 329 patients were randomly assigned to TTM-hypothermia (n=166) or normothermia (n=163) [66]. This trial reported a median of 6.4 hours after ROSC to reach goal temperature for TTM-hypothermia and 5.7 hours for normothermia. This trial did not detect the planned 15% absolute increase in one-year survival (49% vs. 46%) nor survival with a favorable behavioral score (36% vs. 39%) between groups.
In THAPCA-OHCA, 295 patients were randomly assigned to TTM-hypothermia (n=155) or normothermia (n=140) [65]. In this trial median time to target temperature range was 7.6 hours (IQR, 6.2–9.6 hours) for TTM-hypothermia patients and 7.4 hours (IQR, 6.2–9.8 hours) for normothermia patients [67]. This trial did not detect the planned 15% absolute increase in 1-year survival (38% vs. 29%) or survival with a favorable behavioral score (20% vs. 12%), though the hazard of mortality was lower for TTM-hypothermia in survival analysis, and Bayesian analyses of the trial support a beneficial effect of TTM-hypothermia [68].
If time to differential treatment is a confounder, all of these trial data might reveal effects if adjusted for time to hypothermia. However, post hoc analyses by time to target temperature are difficult, because patients who are in greater shock, vasodilated, or who have greater impairment of reflexes cool more rapidly than patients who are more intact [69,70]. Thus, shorter time to a hypothermic target temperature and lower temperature on hospital arrival are independently associated with worse outcomes, obscuring any treatment effect of TTM-hypothermia [71].
Illustrating this confounder and its interaction with treatment group, a post hoc analysis of the THAPCA-OHCA trial found that patients in the TTM-hypothermia group who achieved shortest times to goal temperature had longer estimated duration of chest compressions, received more epinephrine doses, and had higher first lactate levels [67]. Conversely, patients in the normothermia group with the shortest time to goal temperature had lower lactate levels. With limited sample sizes, adjustment for all of these interactions may not be possible, and post hoc analyses of pediatric and adult OHCA trials do not show a clear interaction of time to cooling and hypothermia for outcomes [67,72].
In summary, clinical trials in neonates demonstrate how TTMhypothermia can improve recovery from HIBI when treatment groups have different temperatures within 6 hours and treatment continues for 72 hours, but trials of TTM-hypothermia for 48 hours in children share many implementation challenges with adult trials.
RAPID INDUCTION OF HYPOTHERMIA IN ADULTS
Several adult trials demonstrate the feasibility of very rapid initiation of TTM-hypothermia, but these trials treated patients differently only for a short period of time. In a trial of an intranasal cooling intervention, temperatures were lower in the intervention group between 25 and 182 minutes after ROSC, but there was no change in 90-day survival (17.8% vs. 15.6%) or good functional recovery (16.6% vs. 13.5%) [18].
Rapid infusions of cold intravenous fluids in the ambulance after ROSC can quickly reduce temperature [72,73]. A trial of postROSC cold intravenous fluids allowed patients to reach target temperature about 1 hour faster than usual care patients but did not treat patients differently after hospital arrival [16]. Rapid infusion of cold intravenous fluids during OHCA also reduced core temperature by the time of hospital arrival [17]. All the trials using cold intravenous fluid either after ROSC [16,73,74] or during arrest [17] are complicated by an apparent adverse effect of fluids on cardiopulmonary function, including higher risk of death at the scene, rearrest, or pulmonary edema at the hospital.
Thus, rapid initiation of TTM-hypothermia is possible, but trials to date result in temperature differences between groups for only 1 to 2 hours, and all patients were treated similarly during the key therapeutic windows (Fig. 1). Consequently, these trials did not detect changes in neurological recovery [16,17,73,74].
ILLNESS SEVERITY INFLUENCES TREATMENT EFFECT OF TTM-HYPOTHERMIA
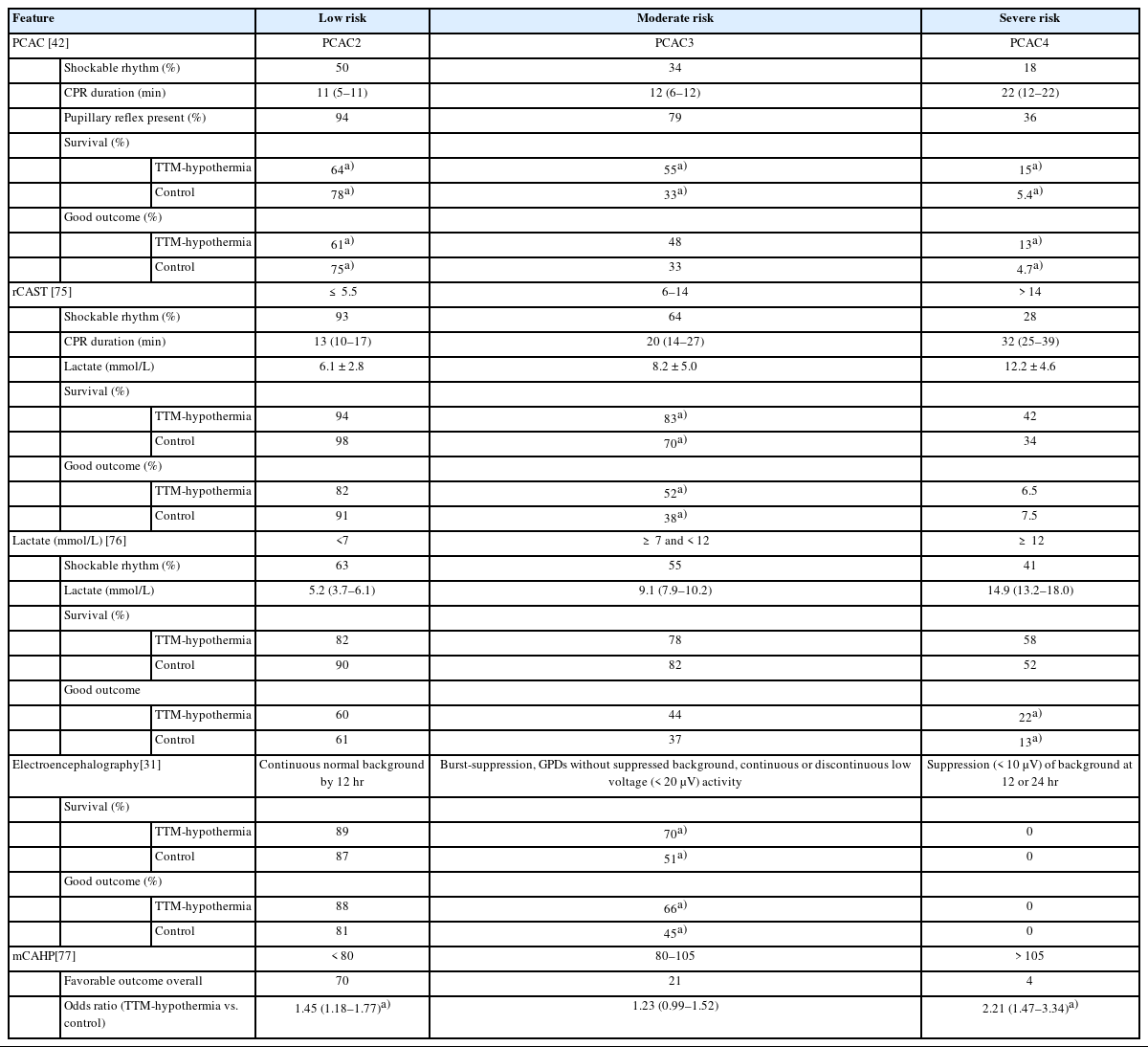
One interpretation of conflicting clinical trial results is that TTMhypothermia offers less benefit for certain cohorts of adult patients, such as the cardiac population in TTM and TTM2 trials with high probability of good outcome [26,27], but may be more beneficial for other cohorts of patients with lower probability of good outcome, such as the more frequent respiratory arrest population in the HYPERION trial [62]. Observational studies support a differential treatment effect for TTM-hypothermia across subgroups, and these studies have an advantage over the clinical trials in that they include a more diverse cohort of patients (Table 2) [31,42,75–77].
Using initial clinical severity to stratify patients, one series from a single North American center took advantage of practice variation after the 2013 TTM Trial to compare 1,319 OHCA and IHCA patients treated with TTM-hypothermia (33 °C, n=728) versus TTM at 36 °C (n=591) [42]. For 184 patients with severe cerebral edema on admission and 234 patients with a highly malignant EEG, outcomes were poor regardless of TTM treatment. Among 911 patients with neither severe cerebral edema nor highly malignant EEG, there was an interaction between TTM-hypothermia choice and clinical severity measured using the Pittsburgh Cardiac Arrest Category (PCAC) score. PCAC uses clinical exam to define patients as moderate coma with preserved brainstem reflexes (PCAC2), moderate coma with severe cardiopulmonary dysfunction (PCAC3) and deep coma with missing brainstem reflexes (PCAC4). TTM-hypothermia was associated with higher survival for PCAC3 (55% vs. 33%) and PCAC4 (15% vs. 5%) patients, higher good functional recovery for PCAC3 patients (24% vs. 6%) and higher recovery without severe disability for PCAC4 patients (13% vs. 5%). Conversely, TTM at 36 °C was associated with higher survival (78% vs. 64%) and survival without severe disability (75% vs. 61%) for PCAC2 patients.
A separate clinical severity score was used to stratify 1,111 OHCA patients undergoing TTM in the nationwide Japanese Association for Acute Medicine OHCA database [75]. The revised postcardiac arrest syndrome for therapeutic hypothermia (rCAST) score uses historical and clinical information at hospital admission to describe patients as low severity (≤5.5), moderate severity (≥6 and ≤14.5), or high severity (≥14.5). Patients were treated with TTM-hypothermia (33–34 °C) or higher temperature (35–36 °C). Among moderate-severity patients, TTM-hypothermia was associated with higher 30-day survival (83% vs. 70%) and good functional recovery (52% vs. 38%). However, there was no association of temperature choice with survival or functional recovery for low-severity or high-severity patients.
Initial blood lactate levels in the same Japanese database stratified 435 patients into mild (<7 mmol/l, n=139), moderate (≥7 and <12 mmol/l, n=182) or severe (≥12 mmol/l, n=114) groups [76]. Among severe patients but not among mild or moderate patients, TTM-hypothermia (32–34 °C) compared to TTM at higher temperatures (35–36 °C) was associated with higher 30-day survival (58% vs. 52%) and favorable functional recovery (22% vs. 13%), even when comparisons were adjusted for other patient characteristics.
EEG defined mild, moderate, and severe encephalopathy in a series of 479 OHCA and IHCA patients from five hospitals [31]. Mild encephalopathy comprised a continuous EEG background, and severe encephalopathy comprised a prolonged suppression of background. Other patterns and suppressed background becoming continuous by 24 hours were considered moderate. TTM-hypothermia was associated with good outcome in moderate-encephalopathy patients (66% vs. 45%), but not in those with mild (88% vs. 81%) or severe (0% vs. 0%) encephalopathy. This study had several limitations, including the fact that EEG was sometimes obtained after initiation of TTM regimen and was more often missing among the 36 °C group.
Another analysis used historical factors about the resuscitation in the modified Cardiac Arrest Hospital Prognosis score to define mild (<80), moderate (≥80 and <105), or severe (≥105) risk groups among 2,723 OHCA patients in the Sudden Death Expertise Center registry and 4,202 OHCA patients in the Resuscitation Outcomes Consortium database [77]. In both databases and in pooled data, TTM at 33 to 36 °C was associated with both survival and favorable functional recovery in low and severe risk groups, but this association was weaker in moderate-severity groups.
Thus, observational data from multiple cohorts suggest that the treatment effect of TTM-hypothermia depends on illness severity. The groups of patients who appear to benefit from TTM-hypothermia differ in many respects from the cohorts of patients enrolled in clinical trials that did not detect benefit (Table 1) [24,26–28,62].
Clinicians should consider that imaging, EEG, or clinical exam can identify some patients whose brain injury is so severe that they will do poorly regardless of any current therapy [31,42,75]. Clinical or laboratory features also can identify mildly injured patients whose favorable prognosis is not affected by choice of TTM regimen [31,76,77] or who may even do better with TTM at 36 °C instead of TTM-hypothermia [42]. Future studies need to consider that individual patient characteristics may determine the treatment effect of TTM-hypothermia, and research should explore how to select the best regimen and duration of treatment for each individual patient.
REAL-WORLD IMPLEMENTATION AND DE-IMPLEMENTATION OF TTM-HYPOTHERMIA
Overall survival improved for cardiac arrest patients in many places after implementation of TTM in the early 2000s [78,79]. However, it is impossible to determine if this trend for improvement resulted from the effects of temperature or simply from the adoption of more comprehensive and optimistic protocols of care in this population. Changes in practice after the TTM Trial [25] provides another opportunity to assess the effects of TTM-hypothermia, because many places de-implemented TTM-hypothermia protocols in favor of normothermia but presumably maintained other aspects of protocolized post-cardiac arrest care.
Single centers have reported worsened outcomes with de-implementation of TTM-hypothermia. In 782 OHCA patients transported to one North American center from 2010 to 2017, 453 received targeted temperature management with either TTM-hypothermia (33 °C, n=258) prior to 2014 or TTM at 36 °C (n=195) from 2014 to 2017 [80]. TTM-hypothermia was associated with a nonsignificant higher survival (45% vs. 36%) and significantly higher favorable functional recovery (40% vs. 30%). One Australian institution routinely treated patients who had ventricular fibrillation OHCA with TTM-hypothermia (33 °C) prior to 2013 (n=24) but adopted a practice of TTM at 36 °C after 2014 (n=52) [81]. TTM-hypothermia was associated with higher survival (71% vs. 58%) and favorable functional status at hospital discharge (71% vs. 56%). These investigators noted that patients treated at 36° had higher rates of fever and less reliable maintenance of target temperature.
Larger datasets show similar trends. In the Australia New Zealand Intensive Care Society Adult Patients Database, investigators were able to compare patients admitted to the ICU after OHCA from prior to December 2013 (n=4,450) and after December 2013 (n=5,184) [79]. Temperature data suggest lower temperatures were targeted prior to 2013 and rates of fever increased after 2013. While the overall survival did not differ between the two time periods (47.6% vs. 46.6%), there was a trend for improving survival over time prior to 2013 (1.3%/yr) that reversed after 2013 (–0.6%/yr).
These de-implementation studies are complex to interpret because many other aspects of cardiac arrest care change over time, and implementation of TTM-hypothermia may be correlated with secular trends in resuscitation and also with many other post-cardiac arrest practices such as sedation or timing of prognostic testing. For example, in 3,925 patients from the registry of the Paris Sudden Death Expertise Center, rates of TTM use at any temperature (33–36 °C) declined from 55% in 2011 to 37% in 2017 [82]. During this interval, rates of survival to ICU discharge increased (from 20% to 26%) and favorable functional recovery did not change (from 19% to 23%). However, during this time period, rates of bystander CPR and the proportion of patients with no-flow time ≤3 minutes increased while the proportion of patients with post-reperfusion shock decreased. During the whole time period, receipt of TTM was associated with higher survival from the ICU (37% vs. 20%) and favorable functional recovery (33% vs. 15%), even when adjusting for the other secular trends.
Thus, reports suggest possible risks to abandoning TTM-hypothermia [79–82]. However, the available data do not reveal whether these effects are mediated by choice of goal temperature, by an associated change in practice style, or by changes in the patient characteristics over time.
CONCLUSION
Implementation of TTM-hypothermia after 2002 transformed the clinical care of adults with coma after resuscitation from cardiac arrest, and survival for patients admitted to the intensive care after cardiac arrest increased over the next two decades. Subsequent methodologically more rigorous trials in adults have not detected any benefit, prompting speculation that the regimen of care determines outcome more than the particular target temperature for the enrolled cohorts.
Post hoc analyses and observational data suggest some explanations for these findings. Adult trials may enroll many patients who are not likely to respond to TTM-hypothermia. Treatment effects may differ between strata of patients with different illness severity. TTM-hypothermia may have smaller or no effect on patients with milder severities and no effect on patients who are completely devastated. Despite the feasibility of rapid temperature manipulation, larger multicenter trials based in the ICU do not clearly achieve separation of treatment between groups within the therapeutic window of 4 hours of reperfusion suggested by preclinical data. Finally, the 24-hour TTM intervention most studied in adults is less than the optimal duration in animals or the effective durations in neonates or children. Ideally, any treatment would be titrated to the needs and response of the individual patient.
At this time, TTM-hypothermia is one tool for the care of select patients after cardiac arrest. If initiated rapidly, it can reduce seizures, brain edema and reduce metabolic demand when oxygen delivery is impaired. Using TTM-hypothermia in patients with risks of these temperature-sensitive problems would be reasonable practice based on preclinical and observational data. Aggressive critical care with or without TTM-hypothermia may be sufficient for many patients who resemble the cohorts enrolled in recent large trials, particularly those with clinical features suggesting >50% probability of survival. Future trials should enroll patients with well-defined injury, measure putative mediators of TTM effects or temperature-sensitive conditions, and focus on titration of temperature depth and duration-based patient condition.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
FUNDING
The author’s institution receives research grants from the National Institutes of Health to study resuscitation including hypothermia.
References
Article information Continued
Notes
Capsule Summary
What is already known
Many guidelines recommend targeted temperature management with hypothermia for patients who are comatose after cardiac arrest, but recent large clinical trials could not detect benefits from hypothermia.
What is new in the current study
This review summarizes how hypothermia when implemented quickly during or after reperfusion treats specific pathophysiology that may be present in some patients after cardiac arrest. Patients enrolled in clinical trials vary in severity, and many patients may not have hypothermia-sensitive pathology. Observational data suggest hypothermia might benefit subgroups of patients who can be identified with clinical exam, imaging, or electroencephalography.