Predictors of poor prognosis in patients with heat stroke
Article information
Abstract
Objective
The predictors of poor prognosis in heat stroke (HS) remain unknown. This study investigated the predictive factors of poor prognosis in patients with HS.
Methods
Data were obtained and analyzed from the health records of patients diagnosed with heat illness at Ajou university hospital between January 2008 and December 2017. Univariate and multivariate analyses were performed to identify the independent predictors of poor prognosis.
Results
Thirty-six patients (median age, 54.5 years; 33 men) were included in the study. Poor prognosis was identified in 27.8% of the study population (10 patients). The levels of S100B protein, troponin I, creatinine, alanine aminotransferase, and serum lactate were statistically significant in the univariate analysis. Multiple regression analysis revealed that poor prognosis was significantly associated with an increased S100B protein level (odds ratio, 177.37; 95% confidence interval, 2.59 to 12,143.80; P=0.016). The S100B protein cut-off level for predicting poor prognosis was 0.610 μg/L (area under the curve, 0.906; 95% confidence interval, 0.00 to 1.00), with 86% sensitivity and 86% specificity.
Conclusion
An increased S100B protein level on emergency department admission is an independent prognostic factor of poor prognosis in patients with HS. Elevation of the S100B protein level represents a potential target for specific and prompt therapies in these patients.
INTRODUCTION
Recently, the occurrence rate of heat-related diseases has increased as the average annual temperature has risen globally [1,2]. The increase in the occurrence of heat-related illness secondary to global warming has become a threat to public health, especially among the elderly population [1,3-7]. Among heat-related illnesses (HRIs), heat stroke (HS) is classic and the most serious form of heat injury [8].
According to Kalaiselvan et al. [5] the incidence of HS, a leading cause of hospital mortality related to global warming, is also increasing [1,6]. HS is defined as a core temperature greater than 40°C and the occurrence of central nervous system abnormalities [7-9]. HS is largely divided into classic HS secondary to high external temperature and exertional HS secondary to physical exertion. The pathophysiology of HS involves the activation of numerous inflammatory and hemostatic pathways causing a systemic inflammatory response syndrome and multi-organ dysfunction syndrome [7,8,10,11]. Since progression of the disease is relatively rapid, rapid diagnosis and treatment are vital [12-17]. Severe damage to the central nervous system can result in permanent neurological disability or death. Moreover, the reported mortality is as high as 71% [7,8].
According to Zhao et al., disseminated intravascular coagulation and acute kidney injury are the predictors of major mortality in relation to the prognosis of HS [17-20]. Decreased mental status and delayed transport time from the scene to the final treatment hospital are also poor prognostic factors [1,12,13,15,21]. In association with procalcitonin, interleukin-6 and tumor necrosis factor-alpha are associated with poor prognosis, whereas melatonin can reduce the degree of HS [11,19,22-25]. However, these results are from relatively small studies, case reports, or laboratory experimental studies; therefore, further research is needed.
The S100B protein has a molecular weight of 21 kDa and a half-life of 30 minutes [26,27]. It plays a significant role in predicting the prognosis of various disease groups including traumatic brain injury [28-34]. Considering the pathophysiology of HS, the S100B protein might also be useful in predicting the prognosis of HS.
Nevertheless, the predictors of poor prognosis for HS remain unknown. The purpose of this study was to evaluate the predictors of poor prognosis in patients with HS.
METHODS
Study design and setting
This study was conducted retrospectively by collecting data from patients who visited an emergency medical center of a university-affiliated hospital between January 2008 and December 2017. The study was approved by Ajou Institutional Review Board (AJIRB-MED-MDB-18-282) and was exempt from the informed consent requirement.
The inclusion criterion was a confirmed diagnosis of consecutive HS. HS was defined when the patient had a history of exposure to a high-temperature environment and one or more of the following central nervous system manifestations: Glasgow Coma Scale (GCS) score <8, cerebellar symptoms, convulsions, and seizures. The diagnosis was established according to the patient’s history, clinical characteristics, physical examination, or body core temperature >40°C. The exclusion criteria were as follows: age <18 years, a previous diagnosis of a neuropsychiatric disease, a postcardiac arrest state, current head trauma, or melanoma, which could lead to an elevated serum S100B level. The patients included in this study were divided into those with a good prognosis or those with a poor prognosis. A poor prognosis was defined as the condition in which the patient could not live without assistance at hospital discharge (cerebral performance category score ≥3).
Data collection
Standardized extraction of demographic, clinical, laboratory, and radiological data from medical records was performed by two trained emergency physicians. The collected data included age; sex; pre-existing diseases; GCS score at admission; vital signs including maximum body core temperature from the scene to hospital admission, serum blood urea nitrogen level, creatinine level (mg/dL), aspartate aminotransferase/alanine aminotransferase level, creatine phosphokinase level, troponin I level, and partial thromboplastin/activated partial thromboplastin time; and poor prognosis including hospital mortality.
Any discrepancy between the datasets extracted by the two emergency physicians was resolved by a third physician. Laboratory studies including evaluation of the serum S100B protein level were performed when the patient visited the emergency department. The serum S100B protein level was measured using a quantitative immunoassay analyzer (Modular Analytics E170; Roche Diagnostics, Indianapolis, IN, USA). The cut-off value provided by the manufacturer was 0.105 μg/L, and the lower detection limit was 0.005 μg/L.
Statistical analysis
All data are expressed as means±standard deviation or as medians (interquartile range), as appropriate. The significance of intergroup differences was assessed by using Fisher exact tests for categorical variables and Mann-Whitney U-tests for continuous variables. Multiple logistical regression analysis was performed to identify the factors that could be considered independent predictors of poor prognosis after HRI using the forward stepwise method with the likelihood ratio test. We constructed a multivariate model using variables that were selected from the univariate analysis (P<0.05) and factors known to be associated with factors of poor prognosis after HRI: the time from the highest body temperature to normal body temperature and levels of serum S100B protein, creatinine, alanine aminotransferase, lactate, and troponin I. A P-value <0.05 was considered statistically significant. Receiver operating characteristic curves were constructed to establish the cut-off points for the serum S100B protein level with the optimal sensitivity and specificity in predicting poor prognostic factors in patients with HS. The statistical analysis was performed using PASW Statistics ver. 18.0 (SPSS Inc., Chicago, IL, USA).
RESULTS
Forty-eight patients with HS were included in the present study. After excluding 12 patients with missing data of the S100B protein level, 36 patients were finally included.
Baseline patient characteristics
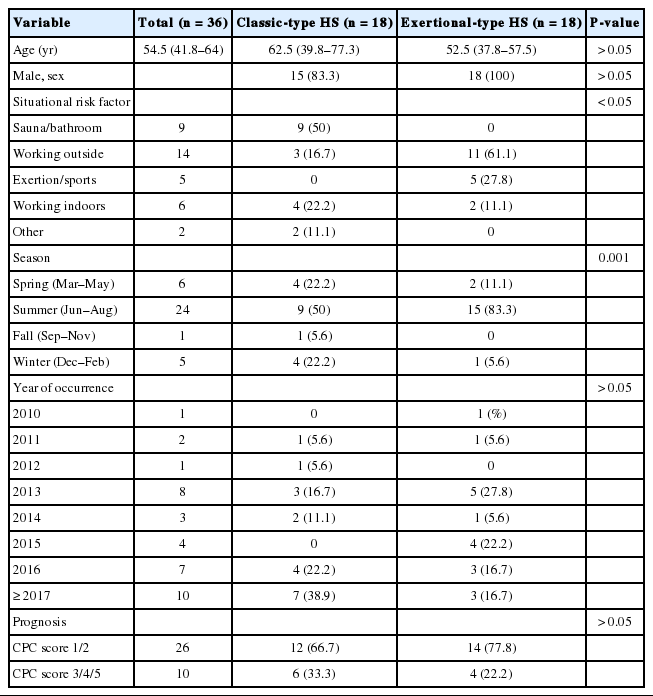
Patients’ median age was 54.5 (41.8–64) years, and 33 patients (91.7%) were men. The incidence of poor prognosis was 27.8% (10 patients including 2 patients who died). Eighteen patients each had classic and exertional-type HS. Other patient characteristics are shown in Table 1.
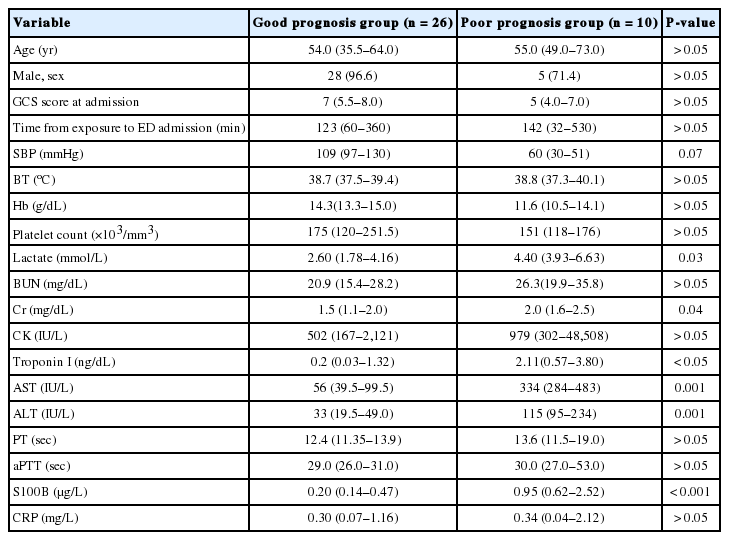
Comparisons of characteristics between the good and poor prognosis groups
The S100B protein levels were significantly higher in the poor prognosis group than in the good prognosis group (median [interquartile range], 0.95 [0.62 to 2.52] vs. 0.20 [0.14 to 0.47]; P<0.001) (Fig. 1). There were statistically significant differences in the serum levels of creatine, lactate, troponin I, aspartate aminotransferase, and alanine aminotransferase and the systolic blood pressure between the two groups (Table 2).

Comparison of S100B protein levels between the good and poor prognosis groups. The box plots show the median S100B protein levels in each group. The median level in the poor prognosis group is about five times higher than that in the good prognosis group (0.95 [0.62 to 2.52] vs 0.20 [0.14 to 0.47] µg/L; P<0.001).
Analysis of factors associated with poor prognosis
Multivariate logistic regression analysis showed that only the serum S100B protein was independently associated with poor prognosis in patients with HS (B 5.18; S.E. 2.16; 95% CI 2.59-12,143.80; P=0.016). The optimal cut-off value of the S100B protein level for predicting poor prognosis was 0.610 μg/L (Fig. 2). The sensitivity and specificity for this cut-off value were 86% and 86%, respectively. The receiver operating characteristic curve is shown in Fig. 2.

Receiver operating characteristics curve for the S100B protein level and poor prognosis of heat stroke. An S100B protein level cut-off of 0.610 µg/L predicted poor prognosis in patients with heat stroke with 86% sensitivity and 86% specificity (area under the curve, 0.91 [95% confidence interval, 0.79 to 1.00]; p=0.001).
DISCUSSION
In the present study, we observed that the S100B protein level was increased in patients with HS. In addition, an S100B protein level >0.61 μg/L predicted poor prognosis in these patients. An increase in the S100B protein level is a poor prognostic factor in diseases associated with the brain, including stroke, traumatic brain injury, and acute carbon monoxide poisoning [28-34]. The S100B protein is also a factor in predicting the prognosis and degree of injury in various diseases in which brain injury occurs, and it showed potential usefulness as a prognostic factor in this study. The S100B protein concentration in the poor prognosis group was 0.95 (0.62 to 2.52) μg/L, which is about five times higher than the value (0.20 [0.14 to 0.47]) μg/L in the good prognosis group. Considering the fact that the pathophysiology of HS is multiorgan injury accompanied by a systemic inflammatory response syndrome and acute brain injury occurs because of a high core temperature, our result is important and meaningful, as it suggests that the S100B protein is a prognostic factor with regard to HS.
Our results showed that the S100B protein level, age, GCS score, systolic blood pressure, prothrombin time, activated partial thromboplastin time, troponin I level, and creatinine level, which are known prognostic factors for HS, were not independent prognostic factors for HS in the logistic regression analysis, although they were statistically significant in the univariate analysis [15,17-19,35-37]. These results were contrary to those of previous studies. Further research is needed to confirm these findings because our study had a small sample size and did not differentiate between exertional and classic-type HS.
Regarding the baseline patient characteristics, the sauna/bathroom was the most common situational risk factor in classic HS. In the sauna and bathroom, as humidity increases, the effectiveness of evaporative cooling from sweating decreases. In these instances, sweating only exacerbates dehydration, which might encourage the development of classic HS [38]. Classic HS occurs irrespective of hot weather or the season if the patient is exposed to hot and humid conditions such as those in a sauna. Therefore, public saunas and bathrooms are important risk factors for the development of classic HS.
Identification of prognostic factors in the early stage of HS is important to achieve the optimal therapeutic effect because it is the basis on which prompt treatment can be started [7,12,16,21,39]. Early identification of S100B protein levels in the emergency department as a prognostic factor might play a role in the active treatment of patients with HS in its early stage. High S100B protein levels are likely to indicate a critical condition requiring prompt treatment in patients with HS because a rapid decrease in core body temperature is critical to preventing the progression of brain injury in patients with HS. Therefore, measurement of the S100B protein levels will be helpful in further studies on brain injuries associated with HRI.
The limitations of our study are as follows. First, although the study period was relatively long, a limited number of subjects was included in the present study; therefore, our findings cannot be generalized. Additionally, we excluded 12 patients because of missing S100B protein data. However, we believe that our report is the first to show the association of the S100B protein level with HS as a prognostic factor. Second, follow-up assessment of the S100B protein level was conducted in a small number of patients in this study; thus, we could not investigate how great a decrease in body core temperature affected a decrease of the S100B protein level. Future prospective studies are required to investigate this topic. Third, although our study was conducted at the final treatment hospital, it was difficult to confirm the final recovery of some patients because of transfers to other hospitals for rehabilitation treatment, which may have affected the outcomes. Lastly, the chart analysis was retrospective.
In conclusion, to our knowledge, this is the first study to evaluate the S100B protein level as a prognostic factor in HS. An increased S100B protein concentration was a prognostic factor for HS in the present study. Although the pathophysiology of HS remains to be elucidated, the possibility of S100B protein as a prognostic factor in HS is worth investigating to determine the best treatment of HS. Early identification of poor prognostic factors and rapid treatment may improve the prognosis in patients with HS. However, further research is required to confirm our findings.
Notes
No potential conflict of interest relevant to this article was reported.
References
Article information Continued
Notes
Capsule Summary
What is already known
Decreased mental status and delayed transport time from the scene to the final treatment hospital are poor prognostic factors in patients with heat stroke.
What is new in the current study
An increased S100B protein level is an independent prognostic factor of poor prognosis in patients with heat stroke.