AbstractObjectiveWe investigated the effects of a quick Sequential Organ Failure Assessment (qSOFA)–negative result (qSOFA score <2 points) at triage on the compliance with sepsis bundles among patients with sepsis who presented to the emergency department (ED).
MethodsProspective sepsis registry data from 11 urban tertiary hospital EDs between October 2015 and April 2018 were retrospectively reviewed. Patients who met the Third International Consensus Definitions for Sepsis and Septic Shock criteria were included. Primary exposure was defined as a qSOFA score ≥2 points at ED triage. The primary outcome was defined as 3-hour bundle compliance, including lactate measurement, blood culture, broad-spectrum antibiotics administration, and 30 mL/kg crystalloid administration. Multivariate logistic regression analysis to predict 3-hour bundle compliance was performed.
ResultsAmong the 2,250 patients enrolled in the registry, 2,087 fulfilled the sepsis criteria. Only 31.4% (656/2,087) of the sepsis patients had qSOFA scores ≥2 points at triage. Patients with qSOFA scores <2 points had lower lactate levels, lower SOFA scores, and a lower 28-day mortality rate. Rates of compliance with lactate measurement (adjusted odds ratio [aOR], 0.47; 95% confidence interval [CI], 0.29–0.75), antibiotics administration (aOR, 0.64; 95% CI, 0.52–0.78), and 30 mL/kg crystalloid administration (aOR, 0.62; 95% CI, 0.49–0.77) within 3 hours from triage were significantly lower in patients with qSOFA scores <2 points. However, the rate of compliance with blood culture within 3 hours from triage (aOR, 1.66; 95% CI, 1.33–2.08) was higher in patients with qSOFA scores <2 points.
INTRODUCTIONThe Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) defines sepsis as a kind of life-threatening organ dysfunction caused by a dysregulated host response to infection [1]. This guideline also recommends the use of the quick Sequential Organ Failure Assessment (qSOFA) score as a simple bedside screening tool for sepsis outside intensive care units [2]. The qSOFA includes a systolic blood pressure (BP) of ≤100 mmHg, a respiratory rate of ≥22 breaths/min, and altered mentation, and a qSOFA score of ≥2 points is considered a positive result. Although the qSOFA score can be easily and reliably obtained during emergency department (ED) triage, many studies have reported concerns about the low sensitivity of qSOFA at triage for mortality prediction [3-9].
Sepsis is a medical emergency for which immediate recognition and resuscitation are critical for patient survival [10]. As such, the low sensitivity of qSOFA may lead to a delay in its diagnosis, which may in turn cause a delay in timely treatment. However, to the best of our knowledge, no study has reported delayed resuscitation associated with a qSOFA-negative result in sepsis patients. The hypothesis of this study was that compliance with sepsis bundle management may be delayed in patients with a qSOFA-negative result at triage [11]. As such, we evaluated the association between a qSOFA-negative result at triage and the delay in resuscitation efforts in ED sepsis patients.
METHODSDesign and settingThis study was a retrospective analysis using the multicenter prospective registry of the Korean Shock Society (KoSS). The KoSS registry was designed to evaluate the clinical characteristics, therapeutic interventions, and outcomes of ED patients with septic shock based on the sepsis definition of the 2012 Surviving Sepsis Campaign guideline and the 1991 consensus conference definition of the American College of Chest Physicians and the Society of Critical Care Medicine [11-13]. Eleven EDs participated in the KoSS registry from October 2015 to April 2018. The criteria for inclusion of patients in the KoSS registry were as follows: age of ≥19 years, directly visited participating EDs during the study period, diagnosed as having septic shock ≤6 hours after arrival, agreed to participate, had no advanced directives, and was not transferred to another facility.
Septic shock is defined by having a suspected or confirmed infection and evidence of refractory hypotension (persistent hypotension after intravenous fluid challenge) or hypoperfusion (hyperlactatemia) [14]. However, systemic inflammatory response syndrome criteria were not obligatory for enrollment. Since the registry was opened before the announcement of the new definition, not all patients in this study fulfilled the new Sepsis-3 definition of septic shock. We decided to include all patients who fulfilled the Sepsis-3 definition of sepsis. As such, we excluded patients with missing triage vital signs essential to calculate the qSOFA score, with missing 28-day survival data, and with a SOFA score <2 points, as these conditions do not comply with the Sepsis-3 definition.
Participation in the KoSS registry was approved by the institutional review boards (IRBs) of the individual participating hospitals, and informed consent was obtained according to the Seoul National University Hospital IRB policy (No. 1408-003-599). This retrospective analysis was also approved by the IRB of Seoul National University Hospital (No. 2012-062-1179).
Data collectionAll KoSS registry data were collected using standardized web-based report forms offered by the research coordinators or physicians at each participating hospital. Among the 200 variables in the KoSS registry, the following data were relevant to this study: demographic characteristics (age and sex), predisposing factors (hypertension and diabetes mellitus), anatomic site of infection (respiratory, hepatobiliary, urinary, gastrointestinal, soft tissue, bone, and joint, mixed, other, or undetermined), vital signs (systolic BP, diastolic BP, heart rate, and body temperature) at triage and enrollment, mental status at triage and enrollment, time variables (triage time and enrollment time), severity measures (initial lactate and SOFA score), outcomes (ED length of stay, outside intensive care unit admission, mechanical ventilation, renal replacement therapy, and 28-day mortality), and 3-hour bundle components (lactate measurement, blood culture, antibiotics administration, and 30 mL/kg crystalloid administration). The time point when the patient was suspected of having sepsis by the physician was defined as the enrollment time. The specific time when each bundle component was delivered, except for crystalloid administration, was recorded in the registry. Fluid resuscitation was coded as whether 30 mL/kg of crystalloid was administered within 3 or 6 hours from triage.
Primary exposure was defined as a qSOFA score ≥2 points at ED triage. Four 3-hour bundle components were selected as the primary outcomes because the KoSS data were collected before the 2018 Update of Surviving Sepsis Campaign Bundle, which recommended a 1-hour bundle [15].
Statistical analysisContinuous variables were expressed as medians with interquartile ranges and categorical variables were expressed as percentages. The Wilcoxon rank-sum test was used to compare the continuous variables, and the chi-squared test was used to compare categorical variables between the two groups. The Wilcoxon signed-rank test was also used to compare continuous variables within the paired observations. A histogram using a density scale for the vertical axis with a kernel density curve added was used to visualize the temporal data distribution. A multivariate logistic regression analysis including age, sex, site of infection, and qSOFA score was constructed to predict each bundle component.
Two-tailed P-values <0.05 were considered to be statistically significant. All analyses were performed using either Stata ver. 14.2 (Stata Corp., College Station, TX, USA) or R Statistics (R Foundation for Statistical Computing, Vienna, Austria; http://CRAN.R-project.org).
RESULTSPopulation and baseline characteristicsAmong the 2,250 patients enrolled in the KoSS registry, 2,087 were included in our analysis following the exclusion of patients with missing data on primary exposure (n=2) and mortality outcomes (n=124) or with SOFA scores <2 points (n=37) (Fig. 1). Patients with qSOFA scores ≥2 points at triage totaled only 31.4% (656/2,087) of the study population.
The clinical characteristics of enrolled patients according to their qSOFA scores at triage are described in Table 1. Patients with qSOFA scores <2 points at triage were younger and had respiratory infections less frequently. Patients with qSOFA scores <2 points had higher BPs, lower heart rates, lower respiratory rates, and higher body temperatures at triage than patients with qSOFA scores ≥2 points. All qSOFA components were observed less frequently in patients with qSOFA scores <2 points. The time from triage to registry enrollment was longer among patients with qSOFA scores <2 points. Patients with qSOFA scores <2 points had higher BPs, lower heart rates, lower respiratory rates, and higher body temperatures at enrollment as well. Patients with qSOFA scores ≥2 points had higher initial lactate levels and SOFA scores. Patients with qSOFA scores ≥2 points also had a higher 28-day mortality rate (33.4% vs. 16.3%, P<0.001).
Bundle compliance ratesThe temporal distributions of enrollment, lactate measurements, blood cultures, and antibiotics administration are visualized in Fig. 2. The times from triage to enrollment, lactate measurement, and administration of antibiotics, respectively, were shorter among patients with qSOFA scores ≥2 points, while the time to blood culture was shorter among patients with qSOFA scores <2 points.
The bundle compliance profile according to qSOFA scores at triage is described in Table 2. Rates of sepsis bundle compliance with lactate measurement (92.5% vs. 96.7%), antibiotics administration (63.2% vs. 73.5%), and 30 mL/kg crystalloid administration (70.5% vs. 78.1%) within 3 hours from triage were significantly lower in patients with qSOFA scores <2 points. However, the rate of compliance with blood culture within 3 hours from triage (82.0% vs. 72.6%) was higher in patients with qSOFA scores <2 points. Also, 31.1% of patients with qSOFA scores ≥2 points received antibiotics prior to blood culture, which was significantly higher than the 16.6% of patients with qSOFA scores <2 points who did (Table 2).
Multivariate logistic regression showed a qSOFA-negative result was independently associated with lower compliance with lactate measurement (adjusted odds ratio [aOR], 0.47; 95% confidence interval [CI], 0.29–0.75), antibiotics administration (aOR, 0.64; 95% CI, 0.52–0.78), and 30 mL/kg crystalloid administration (aOR, 0.62; 95% CI, 0.49–0.77) within 3 hours from triage (Table 3). Also, compliance with blood culture within 3 hours from triage was significantly higher among patients with qSOFA-negative results (aOR, 1.66; 95% CI, 1.33–2.08; P<0.001).
DISCUSSIONIn this study, we found that a qSOFA-negative result at ED triage is associated with low compliance with lactate measurement, broad-spectrum antibiotics administration, and 30 mL/kg crystalloid administration within 3 hours in sepsis patients.
Singer et al. [1] recommended that clinicians monitor clinical conditions, reevaluate patients for possible sepsis, and calculate full SOFA scores for those patients with suspected infection and an initial qSOFA-negative result. Additionally, they emphasized that failure to attain a qSOFA score of ≥2 points should not lead to a delay in any other care aspects. However, in this study, sepsis patients with qSOFA-negative results (qSOFA score <2 points) at triage were subsequently recognized as having sepsis and later received the resuscitation bundle, composed of lactate measurement, antibiotics administration, and 30 mL/kg crystalloid administration less frequently and later than patients with a qSOFA of 2 or greater.
Sepsis is a medical emergency in which early identification and appropriate immediate management improve outcomes [16,17]. Therefore, the 2018 update of the Surviving Sepsis Campaign recommended that all 3- and 6-hour bundles be initiated even within 1 hour [15]. Assuming sepsis was recognized and the participating clinicians decided to include the patient in the KoSS registry, then patients with qSOFA-negative results at triage required a median of 65 minutes to be recognized as having sepsis. Lactate measurement, antibiotics administration, and 30 mL/kg crystalloid administration were significantly delayed in patients with qSOFAnegative results, while blood culture was performed earlier for these patients. There are several possible explanations for this difference. First, patients with fever (initial body temperature ≥38°C) are more likely to receive a blood culture test early, and patients with qSOFA-negative results had fever more frequently (624/1,431 [43.6%] vs. 243/656 [37.0%], P=0.005) (Table 1). Among patients with fever, the time to blood culture was similar between patients with qSOFA scores <2 points (45.9 minutes) and those with qSOFA scores ≥2 points (48.1 minutes, P=0.193) (Supplementary Table 1). However, the time to blood culture was significantly delayed in patients without fever (85.2 vs. 45.9 minutes, P<0.001). Furthermore, among patients without fever, the time to blood culture was delayed more in patients with qSOFA-positive results (102.7 vs. 76.5 minutes, P<0.001). We think that this delay is due to the lack of priority of blood culture tests for treatments required to maintain hemodynamic stability in these critically ill patients. The Surviving Sepsis Campaign recommended that the administration of appropriate antibiotic therapy should not be delayed in order to obtain blood cultures [15]. In this study, patients with qSOFA scores ≥2 points apparently had a greater severity, which led to early initiation of life-saving treatments such as lactate measurements, antibiotics administration, and fluid boluses. Blood culture tests may have been delayed due to these treatments, especially in EDs with limited resources. As mentioned in the results section, the fact that more patients with qSOFA scores ≥2 points received antibiotics prior to blood culture also supports this opinion.
We have shown that qSOFA-negative results were associated with delayed resuscitative measures. More importantly, patients with qSOFA-negative results at triage accounted for 68.6% of the sepsis cases in this study. Additionally, more than half of the sepsis patients with mortality (233/452, 51.5%) had qSOFA scores <2 points at triage. Many studies performed in an ED setting consistently reported a low prevalence of patients with qSOFA-positive results for sepsis [3-9]. Although the severity of patients with qSOFA-negative results was lower than of patients with qSOFA-positive results, the 28-day mortality rate of these patients was as high as 16.3% in this study.
If a considerable number of sepsis patients have qSOFA-negative results at initial presentation, which is associated with delayed recognition and treatment delivery, an additional screening tool should be considered. The repeated assessment of the qSOFA score may be an alternative. Kievlan et al. [18] reported using in-hospital mortality data that repeated qSOFA measurements improve predictive validity for sepsis compared to a single qSOFA measurement. However, they used repeated qSOFA measurements performed over 48 hours, which is not appropriate in emergency situations. In this study, only 23.5% of patients with qSOFA-negative results at triage had qSOFA scores ≥2 points at enrollment. Seymour et al. [2] reported that the addition of serum lactate levels significantly improved the predictive validity of qSOFA and had a discriminative ability for in-hospital mortality in patients with a qSOFA score of 1 point. A previous study [8] also reported that adding lactate ≥2 mmol/L significantly increased sensitivity (61.9% vs. 90.9%) of qSOFA for 28-day mortality. Ho and Lan [19] reported that this approach could have a higher predictive ability comparable to that of the standard SOFA score. We contend that emergency physicians should be aware that the qSOFA score derived from triage vital signs is not sensitive enough to identify patients at high risk for in-hospital mortality and suggest the measurement of serum lactate levels in patients with suspected infection to determine whether early resuscitation is warranted [20].
Our study had several limitations. Data from a multicenter prospective registry were analyzed in this study. However, a considerable number of patients were not enrolled in the chosen registry because written informed consent was required by the local IRB policy. Those patients who refused to participate might have had different clinical characteristics. Furthermore, the KoSS registry was intended to include patients with septic shock. Although we enrolled patients who fulfilled the new definition of Sepsis-3, those patients enrolled in this study may have a higher severity than general ED patients with sepsis, and we may have included more patients with the qSOFA component of hypotension. However, sepsis patients with greater disease severity and likelihood of hypotension are more likely to benefit from bundle therapy. When we analyzed patients who met the septic shock criteria of Sepsis-3, the results were similar to those of this study. Finally, the purpose of this study was to confirm that a qSOFA-negative result was associated with a delay in bundle therapy, not to confirm the effects of such a delay on mortality. All components of the bundles are not equally effective and not supported by solid evidence [21]. However, this issue is beyond the scope of this paper.
In conclusion, we found that a qSOFA-negative result at ED triage is associated with low compliance with lactate measurement, broad-spectrum antibiotics administration, and 30 mL/kg crystalloid administration within 3 hours for sepsis patients.
SUPPLEMENTARY MATERIALSupplementary material is available from: https://doi.org/10.15441/ceem.22.230.
Supplementary Table 1.Time from triage to blood culture according to fever and qSOFA score at triage
REFERENCES1. Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 2016; 315:801-10.
2. Seymour CW, Liu VX, Iwashyna TJ, et al. Assessment of clinical criteria for sepsis: for the third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 2016; 315:762-74.
3. Tusgul S, Carron PN, Yersin B, Calandra T, Dami F. Low sensitivity of qSOFA, SIRS criteria and sepsis definition to identify infected patients at risk of complication in the prehospital setting and at the emergency department triage. Scand J Trauma Resusc Emerg Med 2017; 25:108.
4. Goulden R, Hoyle MC, Monis J, et al. qSOFA, SIRS and NEWS for predicting inhospital mortality and ICU admission in emergency admissions treated as sepsis. Emerg Med J 2018; 35:345-9.
5. Henning DJ, Puskarich MA, Self WH, et al. An emergency department validation of the SEP-3 sepsis and septic shock definitions and comparison with 1992 consensus definitions. Ann Emerg Med 2017; 70:544-52.
6. Moskowitz A, Patel PV, Grossestreuer AV, et al. Quick Sequential Organ Failure Assessment and systemic inflammatory response syndrome criteria as predictors of critical care intervention among patients with suspected infection. Crit Care Med 2017; 45:1813-9.
7. Freund Y, Lemachatti N, Krastinova E, et al. Prognostic accuracy of Sepsis-3 criteria for in-hospital mortality among patients with suspected infection presenting to the emergency department. JAMA 2017; 317:301-8.
8. Kim KS, Suh GJ, Kim K, et al. Quick Sepsis-related Organ Failure Assessment score is not sensitive enough to predict 28-day mortality in emergency department patients with sepsis: a retrospective review. Clin Exp Emerg Med 2019; 6:77-83.
9. Perman SM, Mikkelsen ME, Goyal M, et al. The sensitivity of qSOFA calculated at triage and during emergency department treatment to rapidly identify sepsis patients. Sci Rep 2020; 10:20395.
10. Rhodes A, Evans LE, Alhazzani W, et al. Surviving Sepsis Campaign: international guidelines for management of sepsis and septic shock. 2016. Intensive Care Med 2017; 43:304-77.
11. Dellinger RP, Levy MM, Rhodes A, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock. 2012. Crit Care Med 2013; 41:580-637.
12. Shin TG, Hwang SY, Kang GH, et al. Korean Shock Society septic shock registry: a preliminary report. Clin Exp Emerg Med 2017; 4:146-53.
13. Bone RC, Balk RA, Cerra FB, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest 1992; 101:1644-55.
14. Lee MS, Shin TG, Kim WY, et al. Hypochloraemia is associated with 28-day mortality in patients with septic shock: a retrospective analysis of a multicentre prospective registry. Emerg Med J 2021; 38:423-9.
15. Levy MM, Evans LE, Rhodes A. The Surviving Sepsis Campaign bundle: 2018 update. Crit Care Med 2018; 46:997-1000.
16. Seymour CW, Gesten F, Prescott HC, et al. Time to treatment and mortality during mandated emergency care for sepsis. N Engl J Med 2017; 376:2235-44.
17. Liu VX, Morehouse JW, Marelich GP, et al. Multicenter implementation of a treatment bundle for patients with sepsis and intermediate lactate values. Am J Respir Crit Care Med 2016; 193:1264-70.
18. Kievlan DR, Zhang LA, Chang CH, Angus DC, Seymour CW. Evaluation of repeated quick Sepsis-Related Organ Failure Assessment measurements among patients with suspected infection. Crit Care Med 2018; 46:1906-13.
19. Ho KM, Lan NS. Combining quick Sequential Organ Failure Assessment with plasma lactate concentration is comparable to standard Sequential Organ Failure Assessment score in predicting mortality of patients with and without suspected infection. J Crit Care 2017; 38:1-5.
Fig. 1.Patient-selection flowchart. SOFA, Sequential Organ Failure Assessment; qSOFA, quick Sequential Organ Failure Assessment. 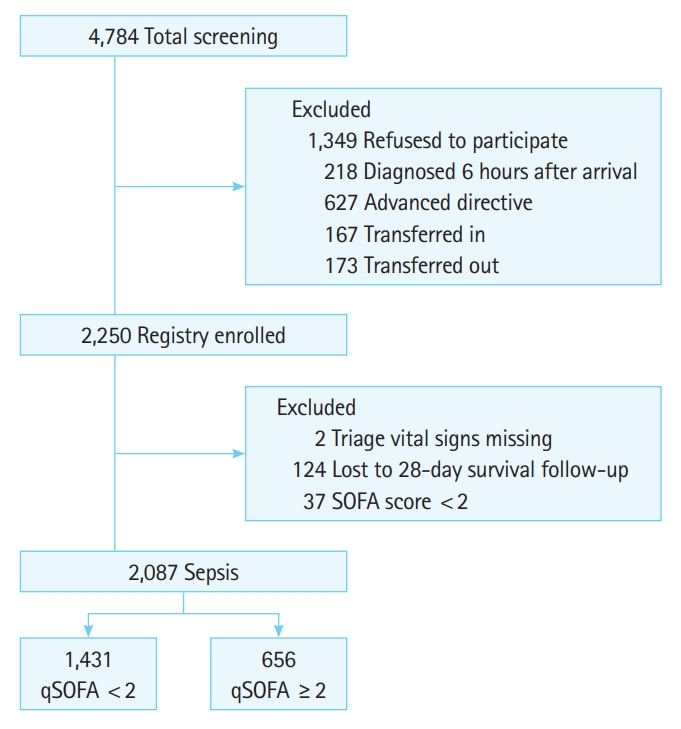
Fig. 2.Histogram using a density scale for the vertical axis and adding a kernel density curve to visualize the temporal distributions of each time variable between patients with quick Sequential Organ Failure Assessment (qSOFA) scores <2 points and qSOFA scores ≥2 points. Time to (A) enrollment, (B) lactate measurement, (C) blood culture, and (D) antibiotics. 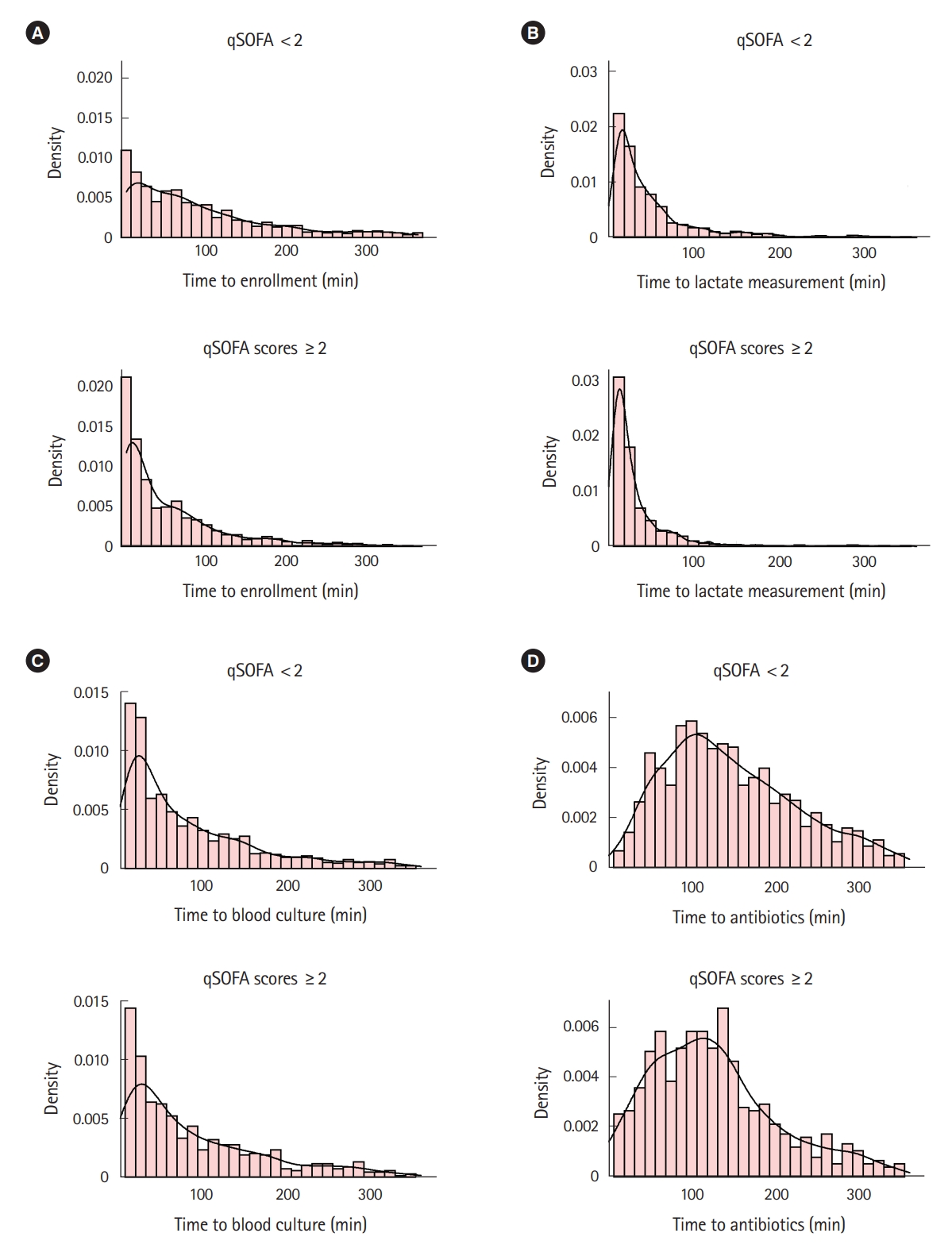
Table 1.Clinical characteristics of sepsis patients according to qSOFA score at triage (n=2,087)
Values are presented as median (interquartile range) or number (%). Continuous variables were compared by the Wilcoxon rank-sum test and categorical variables were compared by the chi-squared test. qSOFA, quick Sequential Organ Failure Assessment; BP, blood pressure; SOFA, Sequential Organ Failure Assessment; ED, emergency department; ICU, intensive care unit. Table 2.Bundle compliances of sepsis patients according to qSOFA scores at triage (n=2,087)
Values are presented as median (interquartile range) or number (%). Continuous variables were compared by the Wilcoxon rank-sum test and categorical variables were compared by the chi-squared test. qSOFA, quick Sequential Organ Failure Assessment. Table 3.Adjusted odds ratio of a qSOFA-negative result for predicting compliance with each bundle component (n=2,087)a)
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||