AbstractObjectiveSteroids are used in cases of sepsis, especially in patients experiencing septic shock. However, clinical trials to date have reported contradictory results. Different patient endotypes and variations in the type and dose of steroid may be at fault for this discrepancy, and further investigation is warranted. In this paper, we propose a new DEXA-SEPSIS study design.
MethodsWe plan to conduct a multicenter, double-blinded randomized pilot study (DEXA-SEPSIS) investigating the feasibility and safety of early use of dexamethasone in sepsis. Participants will be high-risk septic patients presenting to the emergency department with a systolic blood pressure of <90 mmHg or serum lactate level of >2 mmol/L. Participants will be randomized to the following three groups: control, 0.1 mg/kg of dexamethasone, or 0.2 mg/kg of dexamethasone per day for 1 to 2 days. The primary outcome will be 28-day mortality. Secondary outcomes will include time to septic shock, shock reversal, additional steroid administration, number of ventilator-free days, use of continuous renal-replacement therapy, length of stay in the intensive care unit and/or hospital, delta Sequential Organ Failure Assessment score on days 3 and 7, superinfection, gastrointestinal bleeding, hypernatremia, and hyperglycemia.
INTRODUCTIONSepsis is defined as a life-threatening type of organ dysfunction caused by dysregulated host responses to infection [1]. Worldwide, it has high incidence and mortality rates and has become a public health problem [2-4]. Given these characteristics, the World Health Organization has announced sepsis management to be a global health priority [5]. Many drugs have been developed for treating sepsis, but none to date have shown clinical efficacy.
Low-dose steroids are recommended by current guidelines in cases of septic shock requiring ongoing vasopressor therapy, but the evidence in support of this approach is weak [6]. A survey of the available studies covering the effects of steroids in sepsis reveals that steroid dose, sepsis severity (as manifested by the mortality rate of the control group), and timing of steroid administration have varied between them. Steroids may be beneficial in patients with a higher baseline mortality rate [7,8] compared to those with a relatively lower mortality rate. Concomitantly, considering the immunosuppressant nature of steroids, they may actually be harmful when administered in the immunosuppressant phase of sepsis, i.e., usually the late phase of sepsis. Therefore, steroids could be more effective as early therapeutics.
Historically, high-dose steroids have been used to treat sepsis, but no ultimate survival gains have been reported in the literature as a result of this approach [9-11]. Subsequently, low-dose steroids were advocated for, but, in recent years, large and well-designed clinical trials have offered contradictory results [8,12], raising questions about the utility of steroids in septic shock. One meta-analysis has advocated for using a dose of steroids (200ŌĆō400 mg of hydrocortisone per day), which contrasts with the current guideline in sepsis [13]. This dose could be converted to 8 to 16 mg of dexamethasone; in patients weighing 80 kg, the dose would be 0.1 to 0.2 mg/kg. In addition, there is a small-sized randomized controlled trial that adopted a higher steroid dosage (0.2 mg/kg of dexamethasone) in sepsis than that used in the guideline, and the results favored steroid use, but the study lacked a group taking a routine dose of steroid [14]. In one animal study, the administration of 0.2 or 5 mg/kg of dexamethasone improved the survival rate more significantly than 0.1 mg/kg of dexamethasone [15]. Dexamethasone has only anti-inflammatory effects and has a longer half-life, which makes it easier to use in the emergency department. Moreover, another meta-analysis suggested that dexamethasone has the best therapeutic efficacy among various steroids [13].
Considering these results, we hypothesized that the effect of steroids on sepsis might differ according to the steroid dosage and the severity and phase of sepsis. In a pilot study investigating the validity of this hypothesis, we plan to assess the effect of early bolus administration of different doses of dexamethasone in high-risk septic patients.
METHODSEthical statementsThis study has been reviewed and approved by the Institutional Review Board of CHA Bundang Medical Center (No. CHA 2021-02-035), the Institutional Review Board of Samsung Medical Center (No. SMC-2021-03-078), and the Korean Food and Drug Agency.
Design and settingThe proposed study is a multicenter double-blinded randomized phase IIa pilot clinical trial that will be undertaken at two academic emergency departments in Korea. The trial protocol adheres to the Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) statement.
Operational definitionsSepsisThe definition of sepsis in this study will rely on the sepsis-3 definition, which contends that sepsis is a life-threatening type of organ dysfunction caused by a dysregulated host response to infection. Organ dysfunction can be identified as an acute change in the total Sequential Organ Failure Assessment (SOFA) score of Ōēź2 points consequent to the infection. High-risk sepsis patients are defined as sepsis patients with a systolic blood pressure of <90 mmHg or serum lactate level of >2 mmol/L.
Adverse eventsAdverse events will be defined as all adverse events that occur after a study participant is given the study drug. The causality between the events and the study drug does not need to be clear, but events considered as part of the clinical course of sepsis will be excluded.
Renal replacement therapyRenal replacement therapy will be defined in this study as therapy for patients with kidney failure that replaces the blood-filtering function of the kidneys.
Time to shock reversalTime to shock reversal will be defined in this study as the time (in hours) from a state of shock to shock reversal. A state of shock will be defined in this study as a condition that requires a vasopressor to maintain a mean arterial pressure >65 mmHg. Shock reversal will be defined in this study as a point at which the mean arterial pressure had remained >60 mmHg without any vasopressor and 24 hours have passed.
Eligibility criteria for study participationPatients visiting the emergency departments of CHA Bundang Medical Center and Samsung Medical Center who meet all the inclusion and exclusion criteria may be enrolled in this study (Table 1).
Trial protocolDescription of study flowThe present study will be conducted in two emergency departments in Seongnam and Seoul, Korea. We plan to enroll 30 patients in each group, for a total of 90 patients (Fig. 1). Informed consent will be obtained from each patient or their legally authorized representative if the patient meets the inclusion criteria and no exclusion criteria. After informed consent is obtained, randomization will be performed using a random number table. Patients will be treated with the study drug. The usual management for sepsis will be guided by the Surviving Sepsis Campaign international guideline [6].
Study interventionsPatients will be randomly assigned to one of three groups as follows: a control group (placebo), a 0.1 mg/kg of dexamethasone bolus group, and a 0.2 mg/kg of dexamethasone bolus group. The treatment groups will receive their allotted dexamethasone bolus amounts once per day for 1 to 2 days (Fig. 2).
Patients will be allocated to receive a bolus injection of either the intervention (0.1 mg/kg or 0.2 mg/kg of dexamethasone) or identical placebo (0.9% saline). The study infusion package will contain four ampules, each of which has 1 mL of content. The package of the 0.2 mg/kg of dexamethasone group consists of four ampules of dexamethasone, while the package of the 0.1 mg/kg of dexamethasone group consists of two ampules of dexamethasone and two ampules of normal saline; lastly, the package of the placebo group consists of four ampules of normal saline. All ampules will be opened and mixed with 6 mL of normal saline to create 10 mL of the study drug, and a volume of 0.1 times the patientŌĆÖs body weight will be injected to administer an appropriate dose of the drug while retaining the study blinding.
The appearance of the study infusion packages will be identical and there will be no markings on the package other than a four-digit code identifying the study number. Administration of the study drug could be repeated once in a 24-hour interval if there is no other routine use of steroids at the discretion of the treating physician.
Standard therapyKnown management options for sepsis, e.g., fluid, antibiotics, vasopressors, and respiratory care, should be used at the discretion of the treating physician. The use of steroids for the standard treatment of sepsis is possible without unblinding. However, the administration of etomidate during hospitalization will require the withdrawal of the patient from the study.
Randomization, concealment, and blindingPatients will be randomly assigned (1:1:1) via computer-generated permuted block randomization (block size of 3 and 6 to achieve between-group balance) to receive 0.2 mg/kg of dexamethasone, 0.1 mg/kg of dexamethasone, or a placebo. The randomization table will be prepared by a statistician working independently of the study. The investigators, research coordinators, treating physicians, nurses, and patients/family members will remain blinded to the allocated group.
Data collectionThe SOFA score and lactate level will be recorded before study enrollment. Then, during the study period, data will be acquired according to a predefined schedule (Table 2). All data will be collected by research coordinators who have been trained for sepsis registry work over years.
OutcomesPrimary and secondary outcomes will be assessed by a group-blinded research coordinator. Patient electronic medical records will be used to assess the outcomes, and final outcomes, such as 28-day or 90-day mortality, will be determined on the basis of medical records and telephone interviews.
Secondary outcomesSecondary outcomes will include 90-day all-cause mortality, time to septic shock, shock reversal, number of vasopressor-free days, use of continuous renal-replacement therapy, additional steroid administration, number of ventilator-free days, length of stay in the intensive care unit and/or hospital, delta SOFA score on days 3 and 7, superinfection (defined as a secondary infection within 28 days), gastrointestinal bleeding within 14 days, hyperglycemia (defined by a serum glucose level of >150 mg/dL within 7 days), and hypernatremia (defined by a serum sodium level of >150 mmol/L within 7 days).
Statistical analysis and sample size calculationPrimary data will be analyzed by intention-to-treat analysis. Data will also be presented stratified by center and the severity of septic shock according to the use of vasopressors. The statistical analysis will be performed by an independent and blinded statistician. Descriptive data will be presented using median and interquartile range values or mean┬▒standard deviation values, as appropriate. Treatment groups will be compared using the chi-squared test, Fisher exact test, Student t-test, Mann-Whitney U-test, one-way analysis of variance, or Kruskal-Wallis test with post-hoc analysis.
A Kaplan-Meier survival curve with the log-rank test will be used in the time-to-event analysis. Multiple testing corrections will be performed with the Bonferroni method. Since this is a phase IIa study, a sample size calculation will not be required. The sample size would be 102 patients, considering a dropout rate of 10% and allocation of 30 patients to each group.
P<0.05 will be considered statistically significant, and all statistical analyses will be two-sided. All analyses will be performed using R ver. 3.6.3 (R Foundation for Statistical Computing, Vienna, Austria) and Stata ver. 17.0 (StataCorp., College Station, TX, USA).
Data safety and monitoringThe data safety and monitoring board for this study will be composed of two clinicians and one statistician working independently of this study. These individuals will verify adherence to trial procedures and the accuracy of data collection according to national and international requirements and Good Clinical Practice guidelines. This assessment will be performed on a monthly basis by each participating center. They will check the case report forms and verify they are consistent with the source of documentation. They will also confirm that the study process complies with the study protocol.
DISCUSSIONThe current guideline about sepsis suggests using intravenous corticosteroids for adults with septic shock and an ongoing requirement for vasopressor therapy [6]. However, it also noted that the optimal dose, timing of initiation, and duration of corticosteroids remain uncertain. The use of dexamethasone is recommended in patients with COVID-19 or bacterial meningitis without the use of vasopressor therapy and in those with postoperative nausea and vomiting as a single bolus. Given these facts, we propose the use of dexamethasone in the early phase of high-risk sepsis in patients not on vasopressor therapy, which is the motive behind conducting this study.
The results of this phase II study could lead to the design, development, and conduct of a phase III trial powered to evaluate the effects of the use of early dexamethasone in high-risk sepsis patients.
NOTESREFERENCES1. Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 2016; 315:801-10.
2. Rudd KE, Johnson SC, Agesa KM, et al. Global, regional, and national sepsis incidence and mortality, 1990-2017: analysis for the Global Burden of Disease Study. Lancet 2020; 395:200-11.
3. Vincent JL, Sakr Y, Singer M, et al. Prevalence and outcomes of infection among patients in intensive care units in 2017. JAMA 2020; 323:1478-87.
4. Kim J, Kim K, Lee H, Ahn S. Epidemiology of sepsis in Korea: a population-based study of incidence, mortality, cost and risk factors for death in sepsis. Clin Exp Emerg Med 2019; 6:49-63.
5. Reinhart K, Daniels R, Kissoon N, Machado FR, Schachter RD, Finfer S. Recognizing sepsis as a global health priority: a WHO resolution. N Engl J Med 2017; 377:414-7.
6. Evans L, Rhodes A, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Crit Care Med 2021; 49:e1063-143.
7. Annane D, Sebille V, Charpentier C, et al. Effect of treatment with low doses of hydrocortisone and fludrocortisone on mortality in patients with septic shock. JAMA 2002; 288:862-71.
8. Annane D, Renault A, Brun-Buisson C, et al. Hydrocortisone plus fludrocortisone for adults with septic shock. N Engl J Med 2018; 378:809-18.
10. Sprung CL, Caralis PV, Marcial EH, et al. The effects of highdose corticosteroids in patients with septic shock: a prospective, controlled study. N Engl J Med 1984; 311:1137-43.
11. Bone RC, Fisher CJ Jr, Clemmer TP, Slotman GJ, Metz CA, Balk RA. A controlled clinical trial of high-dose methylprednisolone in the treatment of severe sepsis and septic shock. N Engl J Med 1987; 317:653-8.
12. Venkatesh B, Finfer S, Cohen J, et al. Adjunctive glucocorticoid therapy in patients with septic shock. N Engl J Med 2018; 378:797-808.
13. Zhang S, Chang W, Xie J, Wu Z, Yang Y, Qiu H. The efficacy, safety, and optimal regimen of corticosteroids in sepsis: a Bayesian network meta-analysis. Crit Care Explor 2020; 2:e0094.
Fig.┬Ā3.Primary and secondary outcomes. ICU, intensive care unit; SOFA, Sequential Organ Failure Assessment. 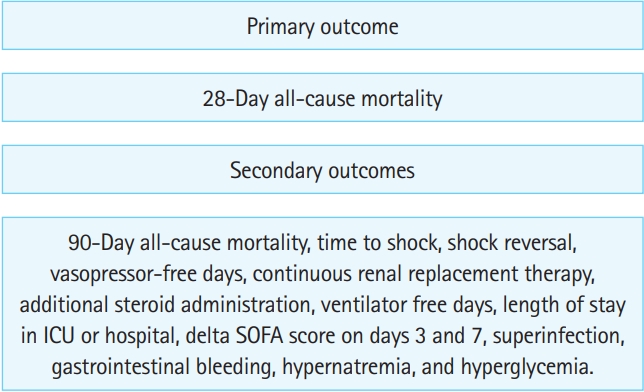
Table┬Ā1.DEXA-SEPSIS study inclusion and exclusion criteria
Table┬Ā2.Study schedule |
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||