AbstractObjectiveThe global spread of the COVID-19 pandemic has affected all aspects of medicine, including orthopedic trauma surgery. This study aims to investigate whether COVID-19 patients who underwent orthopedic surgery trauma had a higher risk of postoperative mortality.
MethodsScienceDirect, the Cochrane COVID-19 Study Register, and MEDLINE were searched for original publications. This study adhered to the PPRISMA 2020 statement. The validity of the studies was evaluated using a checklist developed by the Joanna Briggs Institute. Study and participant characteristics, as well as the odds ratio, were extracted from selected publications. Data were analyzed using RevMan ver. 5.4.1.
ResultsAfter applying the inclusion and exclusion criteria, 16 articles among 717 total were deemed eligible for analysis. Lower-extremity injuries were the most common condition, and pelvic surgery was the most frequently performed intervention. There were 456 COVID-19 patients (6.12%) and 134 deaths among COVID-19 patients, revealing an increase in mortality (29.38% vs. 5.30%; odds ratio, 7.72; 95% confidence interval, 6.01ŌĆō9.93; P<0.001).
INTRODUCTIONThe World Health Organization (WHO) announced the discovery of a new condition, COVID-19, in early February 2020, before declaring a global pandemic in March 2020. The rapid global spread of the causative pathogen, SARS-CoV-2, has caused major changes to human life worldwide. Many countries in the Asia-Pacific region, including Australia, Korea, and Japan, were among the first to respond to the COVID-19 epidemic [1].
During the COVID-19 pandemic, emergency room visits decreased, particularly visits for trauma and surgical intervention in traumatology cases [2,3]. With this reduction in visits, patients more frequently received delayed care during the current pandemic [4]. Previous studies have shown that delaying surgery increases mortality and the risk of postoperative pneumonia in trauma patients [5].
The present study sought to conduct a systematic review and meta-analysis on postoperative mortality in COVID-19ŌĆōpositive and COVID-19ŌĆōnegative patients undergoing orthopedic trauma surgery. The present meta-analysis sought to investigate the odds ratio (OR) of mortality in this patient population by comparing statistics between COVID-19ŌĆōpositive and COVID-19ŌĆōnegative groups. We hypothesized that postoperative COVID-19ŌĆōpositive orthopedic trauma patients would have a higher risk of death than those tested negative for COVID-19.
METHODSSearch strategy and study selectionThe protocol of this review was registered in PROSPERO (International Prospective Register of Systematic Reviews) on September 27, 2022 (No. CRD42022359112). In accordance with recent PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) 2020 statement for identifying research through databases and registers, a systematic review of the mortality in orthopedic surgery owing to trauma during the COVID-19 pandemic was performed, as shown in Fig. 1 and Supplementary Material 1 [6]. The phrases ŌĆ£orthopedicŌĆØ AND ŌĆ£traumaŌĆØ AND ŌĆ£surgeryŌĆØ AND ŌĆ£COVID-19ŌĆØ were used to search the ScienceDirect and MEDLINE (via PubMed) databases for English-language studies that reported mortality among both COVID-19ŌĆōpositive and COVID-19ŌĆōnegative patients. The literature search was conducted on September 20, 2022. A search using MeSH (Medical Subject Headings) terms was carried out whenever possible using the combination of the search 1 (ŌĆ£orthopedic trauma surgeryŌĆØ [MeSH Terms] OR ŌĆ£orthopedic trauma surgeryŌĆØ [All Fields]) AND search 2 (ŌĆ£COVID-19 [MeSH Terms] OR ŌĆ£COVID-19ŌĆØ [All Fields]) strategies.
Inclusion and exclusion criteriaWe included observational studies like cohort, cross-sectional, and caseŌĆōcontrol studies but excluded review articles. The validity of the papers included in this study was evaluated using a series of inquiries based on a checklist in line with the kind of study created by the Joanna Briggs Institute [7,8], as shown in Supplementary Table 1 [9ŌĆō23] and Supplementary Table 2 [24]. Articles that did not fit the requirements for inclusion were rejected. The inclusion criteria formulated according to the PICO mnemonic for clinical research questions were as follows: (1) P (patient, population, problem): patients of all ages who underwent orthopedic trauma surgery; (2) I (intervention, prognostic factor, or exposure): COVID-19 infection (positive or negative polymerase chain reaction result); (3) C (comparison or intervention): none; and (4) O (outcome): postoperative mortality.
Data synthesisIf possible, the data synthesis included information on patient mean age, sex, death rate, underlying disease, complications, intervention site, type of surgery, and hospital stay. The data were summarized in Microsoft Excel (Microsoft Corp) after their collection, and RevMan ver. 5.4.1 (Cochrane Collaboration) was used for statistical analysis. We performed planned subgroup analyses for the confounding variables, which included time points of patient outcome measurement (inpatient vs. 30-day follow-up) and age (<60 years vs. >60 years). Publication bias was measured by visual inspection of funnel plots and quantitatively using Egger test [25]. We considered findings significant if P<0.05. GRADE (Grading of Recommendations, Assessment, Development, and Evaluation) scores were used to evaluate the certainty of the evidence for each outcome [26]. A GRADE summary of the findings in Table 1 was generated using GRADEpro (GradePro Inc.) [27].
RESULTSDuring the literature search, 717 studies were discovered. After removing duplicates, 691 studies remained, and 32 potentially relevant studies were chosen for eligibility examination. This meta-analysis included 16 observational studies (10 retrospective cohort studies, five prospective cohort studies, and one crosssectional study). The majority of patients in these investigations were >60 years old. The study characteristics and postoperative mortality findings are shown in Table 2 [9ŌĆō24]. The most common injury sites were the hip and femur, followed by other lowerlimb sites such as the patella, tibia, ankle, foot, and upper limb. Supplementary Table 3 shows the types of injuries that required orthopedic surgery. Hemiarthroplasty, total hip arthroplasty, unspecified elective minor surgery, and open reduction and internal fixation of the femur were the major surgeries performed.
Five studies [15,18,20,21,24] compared the number of orthopedic surgeries performed during and before the start of the COVID-19 pandemic and discovered that the numbers of surgeries performed did not significantly differ. Nonetheless, postoperative mortality increased significantly during the pandemic.
During the COVID-19 pandemic, 7,795 injuries were reported (Supplementary Table 3), with 15 cases (0.19%) not being treated surgically. According to Table 2 [9ŌĆō24], we identified 6,996 COVID-19ŌĆōnegative patients (93.89%) and 456 COVID-19ŌĆōpositive patients (6.11%) among the 7,452 operative patients who underwent COVID-19 testing via polymerase chain reaction testing of a nasopharyngeal swab. Meanwhile, 134 COVID-19ŌĆōpositive patients (29.38%) died after surgery compared to 5.30% of the COVID-19ŌĆōnegative group, despite the small number of COVID-19ŌĆōpositive patients. The mortality rate of COVID-19ŌĆōpositive patients ranged from 14.28% to 50% among included studies.
Complications due to COVID-19 were most commonly reported as the primary cause of postoperative death among COVID-19ŌĆōpositive patients. The reported primary causes of postoperative death, complications, underlying disease, and mean hospital stay in both groups are shown in Table 3 [9ŌĆō24]. Eight studies [11ŌĆō15,19,20,22] did not report the cause of death in their research.
A total of 1,616 reported surgeries from seven studies [13,16ŌĆō18,20ŌĆō22] are shown in Supplementary Table 4. In contrast, nine studies [9ŌĆō12,14,15,19,23,24] did not specify the surgeries performed in their studies. Only Lim et al. [18] reported the type of anesthesia used in both groups.
Fig. 2 depicts the qualitative analysis of each studyŌĆÖs funnel plot to determine the degree of asymmetry. Egger regression test was calculated with P=0.34. A funnel plot and Egger test showed no evidence of publication bias. As shown in Figs. 3ŌĆō6 [9ŌĆō24], we established a forest plot and subgroup analysis to illustrate the significance among all studies included in our meta-analysis. We analyzed the 16 trials and established a random-effects model, resulting in an overall OR of 7.72 (95% confidence interval [CI], 6.01ŌĆō9.93; P<0.001; I2=0%). The test for subgroup differences in Figs. 4 and 5 [9ŌĆō24] indicated a statistically significant subgroup effect (P<0.05) for index hospitalization (OR, 8.67; 95% CI, 5.82ŌĆō12.91), 30-day follow-up (OR, 7.32; 95% CI, 4.30ŌĆō12.49), and in patients with a mean age of >60 years (OR, 7.75; 95% CI, 6.02ŌĆō9.97). Mortality in COVID-19ŌĆōpositive patients with a mean age of <60 years showed an increase in one study, but this increase was not statistically significant (OR, 5.75; 95% CI, 0.46ŌĆō72.30; P=0.18). As shown in Fig. 6 [13ŌĆō15,17,23], the incidence of venous thromboembolism (VTE) was increased among COVID-19ŌĆōpositive patients (OR, 4.08; 95% CI, 1.23ŌĆō13.58). According to these findings, COVID-19 positivity might increase the mortality rate and occurrence of thromboembolism in patients undergoing orthopedic surgery.
DISCUSSIONThis systematic review and meta-analysis looked at the death rate among COVID-19ŌĆōpositive and COVID-19ŌĆōnegative trauma patients undergoing orthopedic surgery. Most of the participants in this study were >60 years old. This finding is consistent with those of Atinga et al. [28], who found that geriatric trauma cases are increasing every year and now account for >25% of all significant trauma cases in the United Kingdom. Aging is associated with progressive physiological changes that affect various systems. Elderly people respond to trauma in a physiologically different manner than other people. Physiological responses in the elderly might vary due to co-occurring diseases, premorbid frailty, and prescribed drugs.
Previous research has linked hip fracture in the elderly to greater morbidity, a loss of autonomy in activities of daily living, a high rate of institutionalization, and mortality. Conservatively, mortality after hip fracture surgery is high in the first year, being approximately 30% of all cases [29ŌĆō31]. In this study, 70 of the 134 patients with postoperative deaths among 456 COVID-19ŌĆōpositive patients who underwent orthopedic surgery had a hip or femur fracture.
According to Supplementary Table 4, the most commonly performed procedure in this study was hip arthroplasty. Haskel et al. [32] discovered that hip fracture volume in the elderly did not decrease during the lockdown period, even in areas severely affected by COVID-19 outbreaks. Age, a large waist circumference, a lower skeletal muscle index, bone mass density, vitamin D level, physical function, nutritional status, and cognitive function are linked to hip fractures in the elderly [33,34].
VTE involves both pulmonary embolism and deep vein thrombosis, respectively, and occurs in 0.6% to 1.5% of patients undergoing total joint arthroplasty. The risk factors for VTE are described by Virchow triad, which are venous stasis, endothelial damage, and a hypercoagulable state. VTE is typically the result of the interaction of two or less causes. Venous stasis can occur both during and after surgery due to intraoperative immobilization. Prolonged immobility raises the possibility of VTE development [35].
Previous research found that COVID-19ŌĆōpositive patients had a higher mortality rate during hip and femur fracture surgery [36ŌĆō39]. Surgery within 48 hours of hospital admission does not correlate with a lower mortality rate in COVID-19ŌĆōpositive patients [13]. As shown in Table 3 [9ŌĆō24], the mean hospital stay length among COVID-19ŌĆōpositive patients undergoing hip and femur surgery was longer than that among COVID-19ŌĆōnegative patients. This result is in line with the study by Kayani et al. [37], which stated that hip surgery in COVID-19ŌĆōpositive patients was associated with a longer hospital stay, longer immobilization, more hospitalizations in the intensive care unit, an increased chance of peri-operative complications, and greater mortality rates. COVID-19ŌĆōpositive patients with a smoking history and multiple (>3) significant comorbidities have a higher risk of death. Identifying factors that contribute to a higher death rate may improve prognostic classification and interdisciplinary perioperative care.
This review has some limitations. The majority GRADE rating in Table 1 was low because the evidence came from observational studies. Inaccurate studies with smaller sample sizes of COVID-19ŌĆōpositive patients may be influenced by chance. Of the 16 studies, only nine provided information about the type of surgery performed, eight reported the primary cause of postoperative death, and just one provided information about the type of anesthesia used in both groups. All of the included studies were conducted prior to the availability of COVID-19 vaccines.
In conclusion, the postoperative mortality rate among COVID-19ŌĆōpositive patients was 7.72 times greater than that of COVID-19ŌĆōnegative patients. Identifying risk factors for increased mortality may improve prognostic classification and perioperative interdisciplinary management. The findings of this study should be considered by the larger orthopedic community when developing guidelines for treating orthopedic trauma in specific populations in the COVID-19 era.
SUPPLEMENTARY MATERIALSupplementary materials are available at https://doi.org/10.15441/ceem.22.403.
Supplementary Table 1.Joanna Briggs Institute risk of bias quality assessment for cohort studies
Supplementary Table 2.Joanna Briggs Institute risk of bias quality assessment for cross-sectional studies
Supplementary Table 3.Indications for orthopedic surgery during the COVID-19 pandemic
Supplementary Material 1.PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) checklist.
REFERENCES1. Kurozumi T, Minehara H, Kim JW, Oh CW, Miclau EE, Balogh ZJ. Orthopaedic trauma care during the early COVID-19 pandemic in the Asia-Pacific region. OTA Int 2021; 4(1 Suppl):e119.
2. Pamungkas KM, Dewi PI, Dyatmika IK, Maharjana MA, Meregawa PF. The impact of the COVID-19 pandemic on trauma cases in the orthopedics and traumatology services: a systematic review. J Kedokt Kesehat Indones 2022; 13:68-78.
3. Nunez JH, Sallent A, Lakhani K, et al. Impact of the COVID-19 pandemic on an emergency traumatology service: experience at a tertiary trauma centre in Spain. Injury 2020; 51:1414-8.
4. Haleem A, Javaid M, Vaishya R, Vaish A. Effects of COVID-19 pandemic in the field of orthopaedics. J Clin Orthop Trauma 2020; 11:498-9.
5. Simunovic N, Devereaux PJ, Sprague S, et al. Effect of early surgery after hip fracture on mortality and complications: systematic review and meta-analysis. CMAJ 2010; 182:1609-16.
6. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021; 372:n71.
7. JBI. Critical appraisal tools for use in JBI systematic reviews: checklist for cohort studies [Internet]. JBI; 2020 [cited 2022 Sep 28]. Available from: https://jbi.global/critical-appraisaltools.
8. JBI. Critical appraisal tools for use in JBI systematic reviews: checklist for analytical cross sectional studies [Internet]. JBI; 2020 [cited 2022 Sep 28]. Available from: https://jbi.global/critical-appraisal-tools.
9. Andrzejowski PA, Howard A, Vun JSH, et al. COVID-19: the first 30 days at a UK level 1 trauma centre and lessons learnt. Cureus 2020; 12:e11547.
10. Beaven A, Piper D, Plant C, Sharma A, Agrawal Y, Cooper G. Thirty-day mortality for proximal femoral fractures treated at a U.K. elective center with a site-streaming policy during the COVID-19 pandemic. JB JS Open Access 2021; 6:e21.00009.
11. Balakumar B, Nandra RS, Woffenden H, et al. Mortality risk of surgically managing orthopaedic trauma during the COVID-19 pandemic. Bone Jt Open 2021; 2:330-6.
12. Clement ND, Hall AJ, Makaram NS, et al. IMPACT-Restart: the influence of COVID-19 on postoperative mortality and risk factors associated with SARS-CoV-2 infection after orthopaedic and trauma surgery. Bone Joint J 2020; 102-B:1774-81.
13. Dallari D, Zagra L, Cimatti P, et al. Early mortality in hip fracture patients admitted during first wave of the COVID-19 pandemic in Northern Italy: a multicentre study. J Orthop Traumatol 2021; 22:15.
14. Egol KA, Konda SR, Bird ML, et al. Increased mortality and major complications in hip fracture care during the COVID-19 pandemic: a New York City perspective. J Orthop Trauma 2020; 34:395-402.
15. Fisher ND, Bi AS, Aggarwal V, Leucht P, Tejwani NC, McLaurin TM. A Level 1 Trauma CenterŌĆÖs response to the COVID-19 pandemic in New York City: a qualitative and quantitative story. Eur J Orthop Surg Traumatol 2021; 31:1451-6.
16. Hall AJ, Clement ND, Farrow L, et al. IMPACT-Scot report on COVID-19 and hip fractures. Bone Joint J 2020; 102-B:1219-28.
17. LeBrun DG, Konnaris MA, Ghahramani GC, et al. Hip fracture outcomes during the COVID-19 pandemic: early results from New York. J Orthop Trauma 2020; 34:403-10.
18. Lim JA, Thahir A, Amar Korde V, Krkovic M. The impact of COVID-19 on neck of femur fracture care: a major trauma centre experience, United Kingdom. Arch Bone Jt Surg 2021; 9:453-60.
19. Pass B, Vajna E, Knauf T, et al. COVID-19 and proximal femur fracture in older adults: a lethal combination? An analysis of the registry for geriatric trauma (ATR-DGU). J Am Med Dir Assoc 2022; 23:576-80.
20. Sobti A, Memon K, Bhaskar RR, Unnithan A, Khaleel A. Outcome of trauma and orthopaedic surgery at a UK District General Hospital during the COVID-19 pandemic. J Clin Orthop Trauma 2020; 11(Suppl 4):S442-5.
21. Thakrar A, Chui K, Kapoor A, Hambidge J. Thirty-day mortality rate of patients with hip fractures during the COVID-19 pandemic: a single centre prospective study in the United Kingdom. J Orthop Trauma 2020; 34:e325-9.
22. Wright EV, Musbahi O, Singh A, Somashekar N, Huber CP, Wiik AV. Increased perioperative mortality for femoral neck fractures in patients with coronavirus disease 2019 (COVID-19): experience from the United Kingdom during the first wave of the pandemic. Patient Saf Surg 2021; 15:8.
23. Zajonz D, Vaitl P, Edel M, et al. Effects of SARS-CoV-2 infections on inpatient mortality of geriatric patients after proximal femoral fracture surgery. Orthopadie (Heidelb) 2022; 51:573-9.
24. Greensmith TS, Faulkner AC, Davies PS, et al. Hip fracture care during the 2020 COVID-19 first-wave: a review of the outcomes of hip fracture patients at a Scottish Major Trauma Centre. Surgeon 2021; 19:e318-24.
25. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997; 315:629-34.
26. In: Schunemann H, Brozek J, Guyatt G, Oxman A, editors. GRADE handbook for grading quality of evidence and strength of recommendations [Internet]. The GRADE Working Group; 2013 [cited 2022 Sep 28]. Available from: https://guidelinedevelopment.org/handbook.
27. GRADEpro GDT: GRADEpro guideline development tool [software]. McMaster University and Evidence Prime; 2022 Available from: https://www.gradepro.org.
28. Atinga A, Shekkeris A, Fertleman M, Batrick N, Kashef E, Dick E. Trauma in the elderly patient. Br J Radiol 2018; 91:1087.
29. Civinini R, Paoli T, Cianferotti L, et al. Functional outcomes and mortality in geriatric and fragility hip fractures: results of an integrated, multidisciplinary model experienced by the ŌĆ£Florence hip fracture unitŌĆØ. Int Orthop 2019; 43:187-92.
30. Mariconda M, Costa GG, Cerbasi S, et al. The determinants of mortality and morbidity during the year following fracture of the hip: a prospective study. Bone Joint J 2015; 97-B:383-90.
31. Downey C, Kelly M, Quinlan JF. Changing trends in the mortality rate at 1-year post hip fracture: a systematic review. World J Orthop 2019; 10:166-75.
32. Haskel JD, Lin CC, Kaplan DJ, et al. Hip fracture volume does not change at a New York City level 1 trauma center during a period of social distancing. Geriatr Orthop Surg Rehabil 2020; 11:2151459320972674.
33. Liu LK, Lee WJ, Chen LY, et al. Association between frailty, osteoporosis, falls and hip fractures among community-dwelling people aged 50 years and older in Taiwan: results from ILan Longitudinal Aging Study. PLoS One 2015; 10:e0136968.
34. Steingrimsdottir L, Halldorsson TI, Siggeirsdottir K, et al. Hip fractures and bone mineral density in the elderly: importance of serum 25-hydroxyvitamin D. PLoS One 2014; 9:e91122.
35. Santana DC, Emara AK, Orr MN, et al. An update on venous thromboembolism rates and prophylaxis in hip and knee arthroplasty in 2020. Medicina (Kaunas) 2020; 56:416.
36. Freitas T, Ibrahim A, Lourenco A, Chen-Xu J. Mortality in COVID-19 patients after proximal femur fracture surgery: a systematic review and meta-analysis. Hip Int. 2022 Aug 12 [Epub]. https://doi.org/10.1177/11207000221116764.
37. Kayani B, Onochie E, Patil V, et al. The effects of COVID-19 on perioperative morbidity and mortality in patients with hip fractures. Bone Joint J 2020; 102-B:1136-45.
Fig.┬Ā1.PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) 2020 statement flowchart of the search strategy and selection of studies. 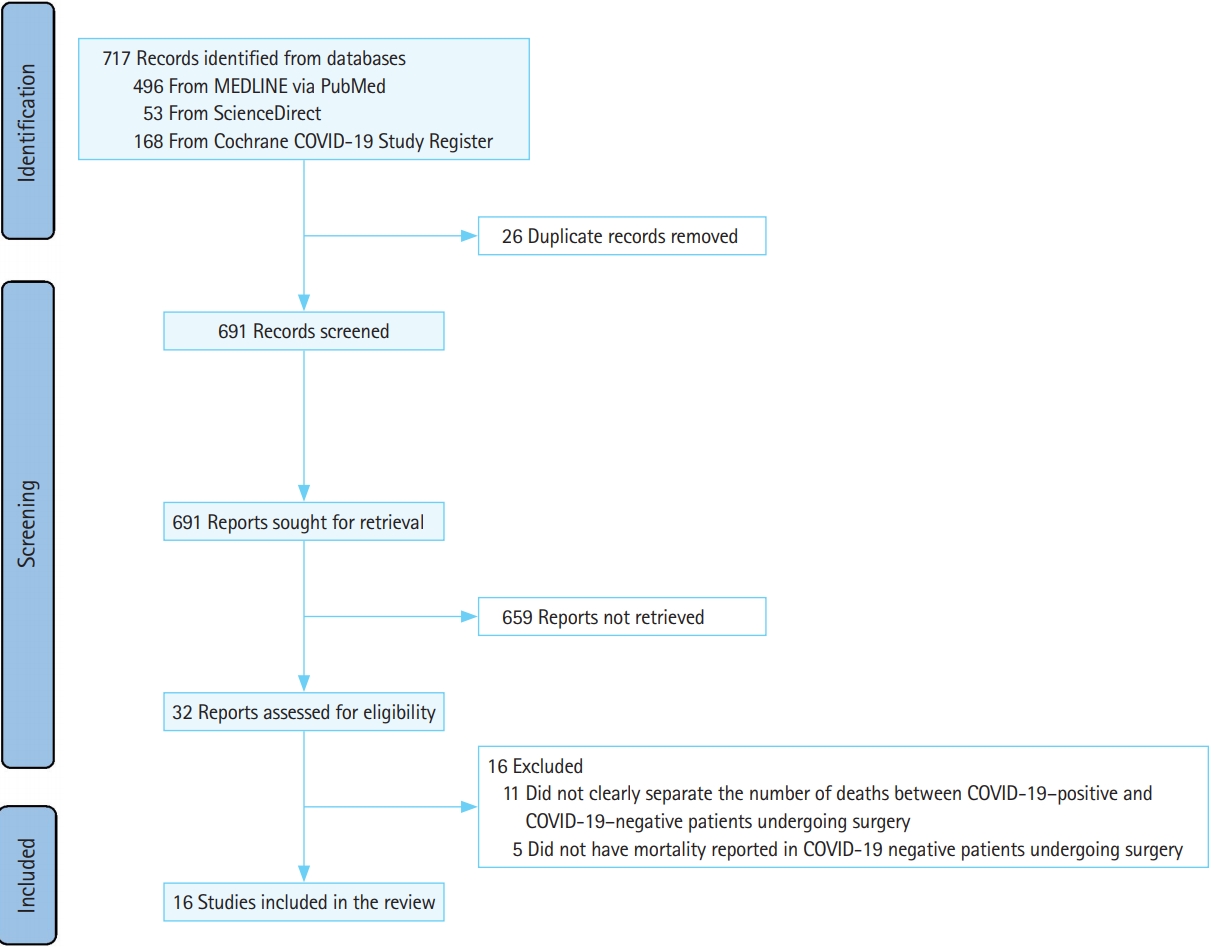
Fig.┬Ā2.No publication bias is visible in the funnel plot of the selected studies. This figure displays the qualitatively evaluated asymmetry findings from each study. OR, odds ratio. 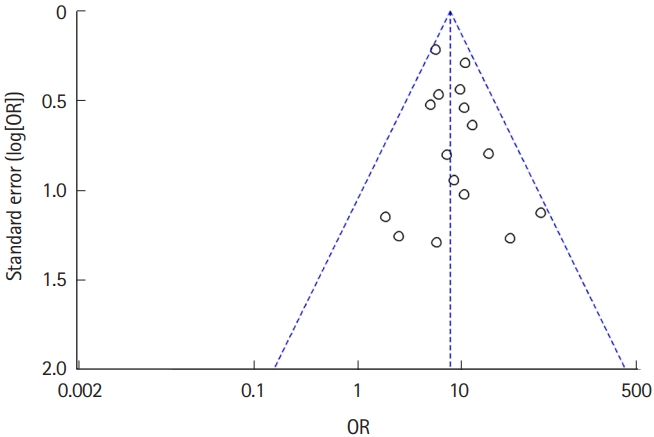
Fig.┬Ā3.Forest plot of all the articles included in this study. M-H, Mantel-Haenszel test; Random, random-effects model; CI, confidence interval. 
Fig.┬Ā4. Postoperative mortality of (A) during index hospitalization and (B) 30-day follow-up. M-H, Mantel-Haenszel test; Random, random-effects model; CI, confidence interval. 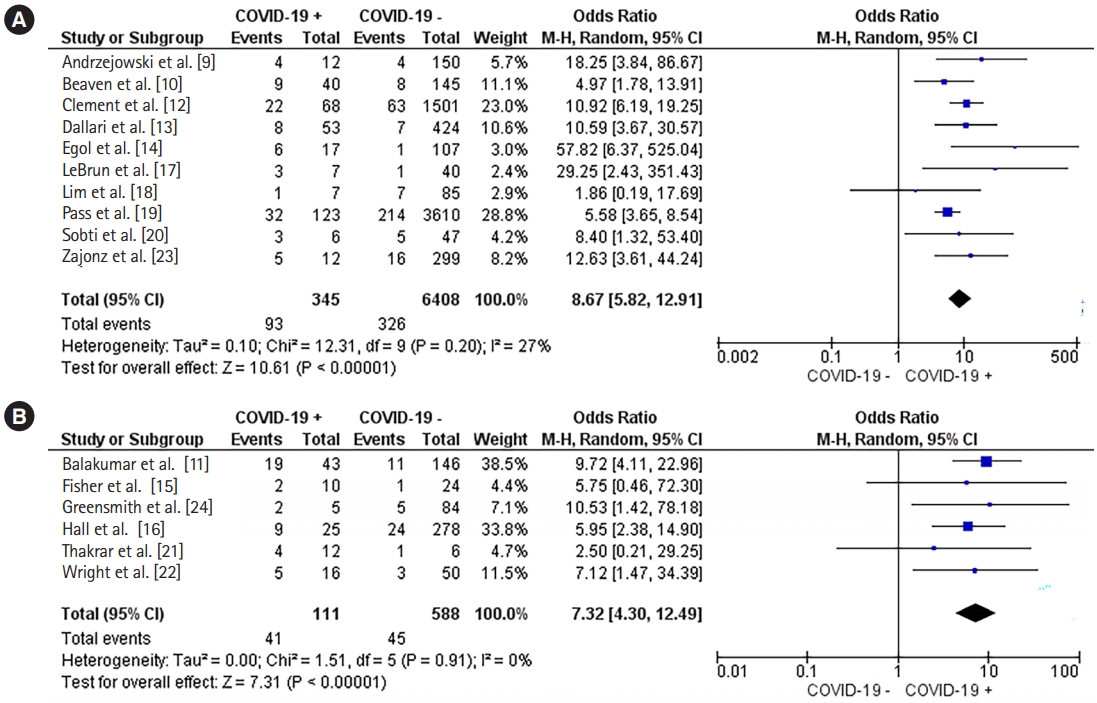
Fig.┬Ā5.Postoperative mortality in the patients with a mean age of (A) >60 years and (B) <60 years. M-H, Mantel-Haenszel test; Random, random-effects model; CI, confidence interval. 
Fig.┬Ā6.Occurrence of venous thromboembolism in COVID-19ŌĆōpositive and COVID-19ŌĆōnegative groups. M-H, Mantel-Haenszel test; Random, random-effects model; CI, confidence interval. 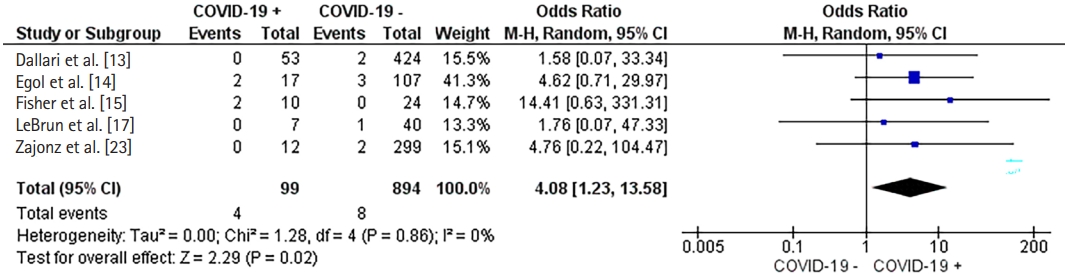
Table┬Ā1.GRADE summary of findings
Table┬Ā2.Study characteristics and postoperative mortality
Table┬Ā3.Incidence of venous thromboembolism, underlying disease, complications, and length of hospital stay in COVID-19ŌĆōpositive and COVID-19ŌĆōnegative groups
COPD, chronic obstructive pulmonary disease; t-ICH, traumatic intracranial hemorrhage; IHD, ischemic heart disease; CKD, chronic kidney disease; AF, atrial fibrillation; NOF, neck of femur; AHF, acute heart failure; UTI, urinary tract infection; ARF, acute renal failure; PE, pulmonary embolism; MI, myocardial infarction; ARDS, acute respiratory distress syndrome; DVT, deep vein thrombosis; UGIB, upper gastrointestinal bleeding; SUO, sepsis of unknown origin; PUD, peptic ulcer disease; GERD, gastroesophageal reflux disease; BPH, benign prostatic hyperplasia; CAD, coronary artery disease; GI, gastrointestinal. |
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||