The predictive value of point-of-care ultrasonography versus magnetic resonance imaging in assessing medial meniscal tears in patients with acute knee injury
Article information
Abstract
Objective
Musculoskeletal ultrasound is increasingly used as the modality of choice in diagnosing many medical situations. The present study aimed to compare the accuracy of point-of-care ultrasonography (POCUS) and magnetic resonance imaging (MRI) to detect acute medial meniscus tears in knee.
Methods
The prospective study was conducted on patients with suspected medial meniscus tears in knee in the emergency department. In the absence of a knee fracture on x-ray, POCUS on the knee was performed. All patients underwent POCUS and MRI of the knee followed by arthroscopy. POCUS findings were then compared to MRI findings to diagnose medial meniscus tears.
Results
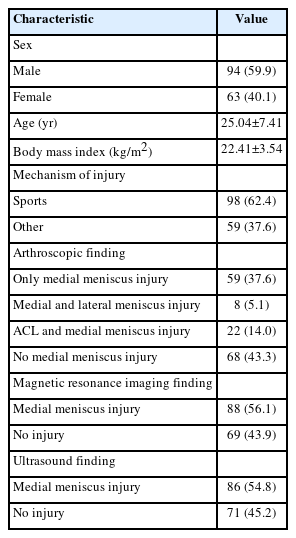
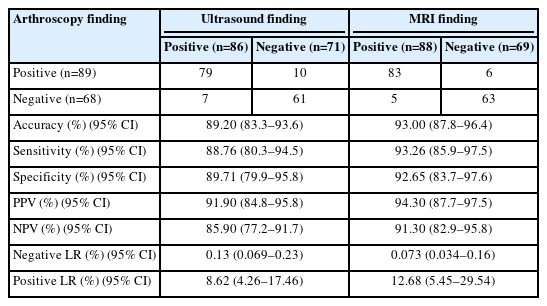
A final total of 157 patients with a mean age of 25.04±7.41 years was included. Out of 157 patients, 94 (59.9%) were male. Medial meniscus tears were detected in 89 patients (56.7%) using arthroscopy as the gold standard. The sensitivity, specificity, positive and negative predictive values, and accuracy of POCUS to detect medial meniscus tears were 88.8% (95% confidence interval [CI], 80.3%–94.5%), 89.7% (95% CI, 79.9%–95.8%), 91.9% (95% CI, 84.8%–95.8%), 85.9% (95% CI, 77.2%–91.7%), and 89.2% (95% CI, 83.3%–93.6%), respectively. The diagnostic accuracy of MRI to detect medial meniscus injury was 93.0% (95% CI, 87.8%–96.4%).
Conclusion
The present study demonstrated that POCUS is an accurate and reliable diagnostic tool alternative to MRI in detecting medial meniscal tears. POCUS had acceptable sensitivity, specificity, and accuracy in detecting meniscal injuries and could be performed as an effective immediate investigation to guide further modalities in patients with acute knee trauma.
INTRODUCTION
Knee trauma is a common complaint in emergency department (ED) patients [1]. Meniscus tears, especially medial injuries, are among the most frequent knee injuries. The meniscus consists of two crescent-shaped pads of thick cartilage and acts as a shock absorber between the tibia and femur while cushioning and stabilizing the knee joint. The structures also help stabilize the knee joint, keeping movements smooth and protecting the bones from wear and tear [1,2]. According to previous studies, meniscal tears affect 23 to 61 of 100,000 people in the general population, mostly due to trauma and degenerative changes [2,3].
Magnetic resonance imaging (MRI) has been considered the best noninvasive diagnostic imaging for this purpose [4]. However, despite its accuracy, MRI is not only expensive and unavailable in some medical centers, but also requires extended waiting periods [5,6]. In addition, it cannot be administered on patients with cardiac pacemakers, metallic implants, or those who suffer from claustrophobia [4–7]. On the other hand, arthroscopy stands as the gold standard diagnostic tool primarily used for diagnosing and treating intraarticular knee injuries [8,9]. While it offers precision, the procedure is invasive, costly, and requires a hospital stay [1,2,9].
Recently, bedside ultrasonography (US) has been increasingly performed to investigate patients with suspected soft tissue or bone injuries due to its accuracy and diagnostic value in ED settings [10,11]. Since knee structures are superficial, they are easily and quickly assessed with US [2,12,13], which is a noninvasive, inexpensive, dynamic, readily available, and real-time modality [14,15]. US has been used to diagnose knee meniscal tears for over two decades [2,14,16]. Point-of-care US (POCUS) can be used efficiently and without being time-consuming in ED settings, especially in patients with trauma [2,10].
In addition, the POCUS examination does not contain ionizing radiation and can be used for focused evaluation in pain and trauma sites, especially in patients with contraindications for MRI [3,4]. POCUS is a suitable alternative to MRI and is faster and cheaper for investigating meniscal tears. Therefore, POCUS has been suggested for the examination of meniscal injuries, but the diagnostic value of US for knee meniscal tears remains controversial [1,3,4]. According to previous studies, a wide range of sensitivity and specificity of US for the diagnosis of meniscal injuries has been reported [1,15–17]. In addition, several studies have demonstrated the diagnostic accuracy of US to be poor and inappropriate compared to MRI for diagnosing meniscal tears [2,18,19], while some have shown them to be very useful and suitable [8,12,20].
This study was conducted in the ED, and POCUS was performed by the attending emergency medicine doctor. The method was compared with arthroscopy as the gold standard, which was not performed in previous studies. Therefore, considering that knee injuries are common in patients referred to the ED and with the presence of controversial findings in previous studies, the purpose of this study was to compare the accuracy of POCUS and MRI to detect medial meniscus tears in patients with acute knee injury, with arthroscopy as the reference (gold standard).
METHODS
Ethics statement
This study was approved by the Ethics Committee of Isfahan University of Medical Sciences (No. IR.MUI.MED.REC.1398.220). Informed consent was obtained from all the participants.
Study design and setting
This prospective cross-sectional study was conducted in the ED of Kashani Hospital (Isfahan, Iran), between February 2021 and May 2022.
Participants
Patients with acute knee trauma with suspected medial meniscus tear by historical and clinical examinations were evaluated. Patients with symptoms such as pain, tenderness, swelling, knee locking, and loss of stability were considered for suspected medial meniscus damage. A convenience sample of patients was enrolled.
Patients older than 18 years presented within 5 days after knee injury planned to undergo arthroscopy after MRI and were willing to participate in the study were included. Patients with multiple trauma, knee fractures, unstable hemodynamics, and a history of a previous medial meniscus injury or knee surgery were excluded, as were those who did not continue with follow-up.
Study protocol
All subjects underwent knee joint POCUS and MRI followed by arthroscopy. Initially, knee x-rays of two views (anteroposterior and lateral) were performed. Knee POCUS were subsequently performed if there was no fracture detected on radiographic imaging. POCUS was performed with an L12-5 liner probe (5–12 MHz) of a standard ultrasonography machine (Philips Affiniti 50, Philips) in the ED by one of four emergency medicine specialists trained in the musculoskeletal US. They had more than 10 years of experience in emergency medicine and received a 2-hour lecture training and a 4-hour practical training that included an assessment of the medial compartment of the knee by an experienced US musculoskeletal radiologist.
The patient was laid in a supine position for the POCUS exam. The probe was placed diagonally in the long axis just above the medial joint access axis, while the knee joint was in 90° flexion. The medial meniscus was observed as a wave between the two hyperechoic parts (distal thigh and proximal leg). A homogeneous meniscus without fluid surrounding it was considered normal. Medial meniscus tears are indicated by a hypoechoic band or stripe within the meniscus, leading to meniscal heterogeneity (Fig. 1).
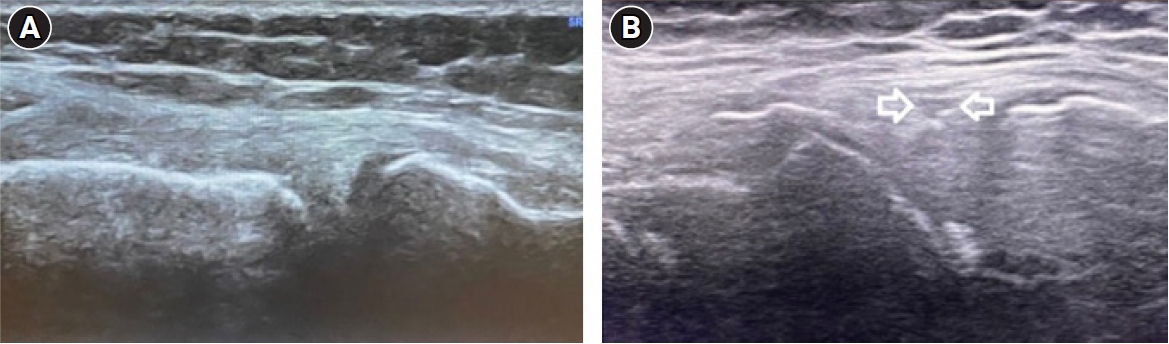
Point-of-care ultrasonography image. (A) Normal medial meniscus. (B) Medial meniscus tear (arrows). F, femur; T, tibia; M, medial meniscus.
Knee arthroscopy was performed within 2 weeks after the POCUS examination. MRI was performed before arthroscopy using a GE Tesla machine (GE Healthcare) with a Quadknee coil specific for the knee. The MRI images were interpreted by a radiologist blinded to the POCUS results using a 30°, 4-mm-diameter oblique arthroscope.
Knee arthroscopy was performed by one of three faculty orthopedic surgeons. All arthroscopic cases in this center were performed by these orthopedists, who were blinded to the imaging results. Arthroscopic findings were used as the standard reference for assessment of the knee. Demographic data (age, sex), POCUS and MRI results, and arthroscopic reports were collected. Finally, POCUS and MRI results were compared with arthroscopy.
Sample size
A sample size of 136 was calculated at a confidence interval of 95% with a sensitivity of 85% based on the results of a previous study [2] with an error level of 0.06. Therefore, the study population of 157 patients was selected for an anticipated dropout rate of 15% to ensure an adequately powered study.
Statistical analysis
All data were analyzed using IBM SPSS ver. 25.0 (IBM Corp) and presented as number (percentage) or mean±standard deviation. Receiver operating characteristic analysis was used to evaluate the diagnostic value of POCUS and MRI. The accuracy, sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), positive likelihood ratios (LRs), and negative LRs of POCUS and MRI for detecting medial meniscus tears were calculated. A significance level of <0.05 was considered in all analyses.
RESULTS
A total of 167 subjects with suspected medial meniscus tear were enrolled in the study. Of them, 157 patients with acute blunt knee trauma were included, and 10 subjects were excluded due to a lack of follow-up for arthroscopy (Fig. 2). The subjects had a mean age of 25.04±7.41 years (range, 15–51 years); 94 (59.9%) were male and 63 (40.1%) were female. Ninety-eight patients (62.4%) suffered sports injury. Medial meniscus tears were detected in 89 patients (56.7%) using arthroscopy as the gold standard. The demographic and clinical findings are reported in Table 1.
Compared with arthroscopic findings, sensitivity, specificity, NPV, PPV, and positive and negative LRs of the POCUS and MRI in the diagnosis of medial meniscus tear are shown in Table 2. Overall, POCUS exhibited a sensitivity, specificity, PPV, NPV, and accuracy of 88.8% (95% confidence interval [CI], 80.3%–94.5%), 89.7% (95% CI, 79.9%–95.8%), 91.9% (95% CI, 84.8%–95.8%), 85.9% (95% CI, 77.2%–91.7%), and 89.2% (95% CI, 83.3%–93.6%) for medial meniscus tears, respectively.
POCUS and MRI could not diagnose 10 and six medial meniscus injuries, respectively. In addition, seven and five false-positive subjects of medial meniscus tears were reported with POCUS and MRI, respectively (Table 2).
DISCUSSION
Recently, the image quality of US has dramatically improved. Therefore, musculoskeletal US has increasingly been used as the diagnostic method in sports medicine, trauma, anesthesiology, and pain medicine. The efficacy of POCUS as the primary triage tool in diagnosing various ligamentous injuries has been demonstrated in multiple studies [2]. The current study demonstrated that 56.7% of subjects with suspected meniscus injury (using arthroscopy as the gold standard modality) had meniscus tears in the knee. A medial meniscus tear was observed in 15.3% to 88% of medial knee injury patients [8]. In addition, the current study revealed that sensitivity, specificity, PPV, and NPV of POCUS in detecting medial meniscus tears were 88.8%, 89.7%, 91.9%, and 85.9%, respectively. The diagnostic accuracy of POCUS and MRI for detection of medial meniscus injuries was 89.2% and 93.0%, respectively.
Elshimy et al. [13] evaluated 60 patients with clinical suspicion of meniscal tear planned for knee arthroscopy. For detecting medial meniscal tears, POCUS and MRI exhibited a sensitivity of 93.8% and 90.6%, specificity of 96.4% and 92.9%, PPV of 96.8% and 93.6%, NPV of 93.1% and 89.7%, and overall accuracy of 95.0% and 91.7%. Cook et al. [7] demonstrated that US and MRI for diagnosing meniscus injuries had sensitivity of 91.2% and 91.7%, specificity of 84.2% and 66.7%, PPV of 94.5% and 84.6%, NPV of 76.2% and 80.0%, and accuracy of 89.5% and 81.1%.
For Dong et al. [1], in a meta-analysis that included seven prospective studies (472 patients), the pooled sensitivity, specificity, and accuracy of US in diagnosing meniscal tears were 88.80% (95% CI, 82.83%–92.87%), 84.66% (95% CI, 75.89%–90.64%), and 93% (95% CI, 91%–95%), respectively. A meta-analysis by Dai et al. [15] evaluated the role of US in assessing meniscal injury. The sensitivity and specificity of the US were 0.88 (95% CI, 0.84–0.91) and 0.90 (95% CI, 0.86–0.93), respectively. In another meta-analysis, Xia et al. [16] demonstrated that US for the detection of meniscal tears exhibited sensitivity, specificity, and area under the curve of 0.775 (95% CI, 0.747–0.801), 0.838 (95% CI, 0.818–0.857), and 0.9107 (95% CI, 0.8625–0.9589), respectively. They determined that US could be used to examine meniscal knee injuries. Although these studies evaluated both medial and lateral meniscus in acute and chronic injuries, their results are consistent with the results of the present study.
Although POCUS is safe, noninvasive, cost-effective, easily available, and can be quickly used for real-time diagnosis, its accuracy in diagnosing meniscal injuries remains controversial [1,3,4]. Azzoni and Cabitza [18] and Bruce et al. [19], in two retrospective studies, reported that US was neither sensitive nor specific in diagnosing meniscal tears. However, promising results have been reported in more recent studies [8,12]. Previous studies have reported wide ranges of sensitivity (75.9%–97.2%) and specificity (83%–100%) [12,13,20]. The results of the present study are also in this range. Several factors may lead to a wide range of results. First, the US resolution has improved in recent years. Second, the linear array probe resolution used in recent years is higher than the convex array probe resolution [1,2]. Choosing the suitable probe increases the accuracy of the US examination, which is especially important in examination of the anterior horns of the meniscus [21]. Third, musculoskeletal US is becoming more common and the technique is more common and known [1,13,15]. Fourth, the technology and training of operators have improved. With new high-quality US devices available in laptops and handheld versions, damage can be detected with greater quality and accuracy [1,2,13,21]. As a result, more patients with meniscal tears have been recently diagnosed.
The diagnostic accuracy of the US for evaluating the medial and lateral meniscus differs, with the US exhibiting higher sensitivity for diagnosing medial meniscus tears compared to lateral meniscus tears [15,20]. In addition, the sensitivity and specificity of US examinations for chronic knee injuries were higher than for acute knee injuries of the medial meniscus of the knee [15,17].
POCUS has several advantages over MRI. First, POCUS can be performed more frequently and without delay compared to MRI. Second, in addition to meniscal tears, POCUS can detect other musculoskeletal diseases in patients with knee trauma. Third, functional (dynamic) POCUS can also be performed like conventional (static) US [1,12,22].
The present study has several limitations. A potential limitation of the present study is that only patients scheduled for knee arthroscopy were included, which could have excluded many patients with meniscal injuries. This was a single-center study, which limits generalizability. The mean age of the patients is very young, limiting generalizability of the POCUS results to elderly patients. Only the medial meniscus was examined. In order to determine simultaneous rupture of the medial collateral ligament, it would be better to evaluate the medial compartment of the knee. POCUS being operator-dependent is the next limitation. Finally, the results of our study cannot be generalized to patients with penetrating injuries, multiple traumas, or injuries older than 5 days or in pediatric patients.
In conclusion, the present study demonstrated that POCUS is an accurate and reliable diagnostic tool alternative to MRI in detecting medial meniscal tears. POCUS exhibited acceptable sensitivity, specificity, and accuracy in detecting meniscal injuries. Therefore, POCUS could be performed as an effective immediate investigation to guide further modalities, such as MRI, in patients with acute knee trauma.
Notes
Author contributions
Conceptualization: all authors; Data curation: all authors; Formal analysis: FH, OA; Funding acquisition: all authors; Investigation: all authors; Methodology: OA, FH, SH, AAM; Writing–original draft: all authors; Writing–review & editing: all authors. All authors read and approved the final manuscript.
Conflicts of interest
The authors have no conflicts of interest to declare.
Funding
This study was supported by Isfahan University of Medical Sciences (Isfahan, Iran).
Data availability
Data analyzed in this study are available from the corresponding author upon reasonable request.
Acknowledgements
The authors thank the cooperation of Isfahan University of Medical Sciences (Isfahan, Iran) and the staff of the emergency department of Kashani Hospital (Isfahan, Iran).
References
Article information Continued
Notes
Capsule Summary
What is already known
Magnetic resonance imaging (MRI) is considered the best and most noninvasive diagnostic imaging for diagnosing knee meniscal injuries. Recently, ultrasound has been used to diagnose meniscal injuries. In previous studies, ultrasound is usually compared with MRI.
What is new in the current study
Considering that knee injuries are common in patients referred to the emergency department and with the presence of controversial findings in previous studies, the purpose of this study was to compare the accuracy of point-of-care ultrasonography and MRI to detect medial meniscus tear in patients with an acute knee injury, with arthroscopy considered the reference (gold standard).