Contemporary approaches to pulmonary embolism diagnosis: a clinical review
Article information
Abstract
The optimal diagnosis strategy for pulmonary embolism (PE) in the emergency department (ED) remains complex. This review summarizes PE diagnosis with clinical presentation, decision rules and investigations for acute PE. This review was performed using studies published between January 1, 2010, and September 1, 2023. PE should be considered in ED in patients with chest pain, shortness of breath, syncope or signs of deep veinous thrombosis. Definitive diagnosis of PE relies on thoracic imaging, with the use of chest tomographic pulmonary angiogram or ventilation-perfusion lung scintigraphy. To limit the continuous increased use of chest imaging, the clinical probability should be the first step for PE workup. The pulmonary embolism rule-out criteria (PERC) can rule out PE at this stage. If not, for low or intermediate probability, several clinical decision rules have been validated, either by ruling out PE on clinical signs, or by raising D-dimer thresholds (YEARS or PEGeD [Pulmonary Embolism Graduated D-Dimer] criteria) or by combination of these different rules. It is recommended that patients with a high clinical probability of PE should undergo chest imaging without the need for D-dimer testing. The PE diagnostic approach can be tailored in specific populations such as pregnant, younger, COVID-19, or cancer patients. PE diagnosis worup illustrates the complexity of modern probabilistic-based approaches of decision-making in medicine. It is recommended to use a Bayesian approach with the evaluation of clinical probability, then order D-dimer if the PERC rule is positive, then adapt the D-dimer threshold for ordering chest imaging using clinical decision rules.
INTRODUCTION
Pulmonary embolism (PE) is a severe condition defined as a clot in a systemic blood vessel, usually a deep vein of the lower limb, migrating to the pulmonary circulation, causing obstruction by preventing the circulation of distal blood flow. It is the major complication of thromboembolic disease. In the general population, the incidence of PE is estimated approximately from 39 to 115 per 100,000 population per year in the United States [1]. The annual incidence of acute PE has increased during the past decade from 45 to 83 per 100,000 adults with a significant decrease in both short- and long-term mortalities [2]. Age is a key risk factor for PE, with a reported sevenfold increased incidence in patients aged >75 years compared to those <50 years [3].
This is particularly relevant for emergency physicians who are treating a growing number of older patients in whom the cause of chief complaints may be complex to diagnose [4]. These numbers are derived from studies in different settings, with biases inherent to the methodology, and vary between countries, studies, and methodology. Some reports suggested that this could be underestimated. Therefore, until no studies can assess the incidence of PE, the real incidence of PE remains unknown, and is greatly influenced by age and other contributing factors. Historic series and studies reported that the in-hospital mortality was of 14% and a 90-day mortality of 20% [2,5–7]. Furthermore, it is reported that in the United States, PE mortality is approximately 60 to 100,000 each year [8,9]. However, this number may not include only patients that died because of a PE. Therefore, the reported death toll of PE may have been overestimated. Approximately one-third of the patients with PE will have a recurrence within 10 years [9]. If untreated, acute PE is associated with a significant mortality rate (as high as 30%), whereas the death rate of diagnosed and treated PE is 8% [10]. In children, the approximatively annual incidence of PE ranges reportedly between one and five per 100,000 in the general population [11].
The diagnosis of PE remains a great challenge for every clinician. PE symptoms are nonspecific and very diverse, justifying consideration of this hypothesis in a wide range of clinical situations including chest pain, syncope, shortness of breath, hemoptysis, and tachycardia. In some cases, PE may be asymptomatic or discovered incidentally during diagnostic workup for another disease. This review summarizes PE diagnosis with clinical presentation, decision rules and investigations for acute PE in the emergency department (ED).
METHODS
This review was performed using PubMed for English-language studies published between January 1, 2010, and September 1, 2023, with the key terms that examined the epidemiology, and diagnosis of PE. Articles were screened using the MeSH (Medical Subject Headings) term “pulmonary embolism” associated with diagnosis, epidemiology, and pathophysiology. Included articles were limited to international guidelines, reviews, and systematic reviews. Of the 344 articles identified, 39 were included. Relevant references were added by authors from selected articles. This review does not require ethical approval or informed consent because there was no direct contact with individual patients.
RESULTS
Clinical presentation
According to several studies in different countries and settings, PE is confirmed in less than 10% of patients in whom the diagnosis was initially suspected, which suggests excessive use of additional tests, side effects from irradiation and contrast injections, as well as consuming material resources and increasing the length of stay in the ED [12]. In the ED, diagnosing PE can be a real challenge for physicians because clinical symptoms are both common and nonspecific to the pathology (namely chest pain, shortness of breath, and syncope). Other more specific symptoms of PE include clinical signs of deep venous thrombosis (DVT), which may be present in about 20% of the patients with PE [13,14]. In some cases, PE may be asymptomatic and incidentally diagnosed during workup for another indication. Hemodynamic instability is a rare but important form of clinical presentation, as it indicates central or massive PE that has severely reduced hemodynamic reserve. Approximately 5% to 10% of patients presenting to the ED report chest pain and dyspnea as their primary symptom [15]. Chest pain is a frequent symptom of PE and is probably caused by pleural irritation due to distal embolism causing pulmonary infarction [13]. A retrospective study reported that in the ED that 30% of patients with chest pain were investigated for PE with 2.6% of PE diagnosed [16]. Dyspnea may be acute and severe in central PE; in small peripheral PE, it is often mild and may be transient. In patients with preexisting heart failure or pulmonary disease, worsening dyspnea may be the only symptom indicative of PE [17]. Although dyspnea is usually of abrupt or rapid onset, in some patients it may progress over several days or even weeks [18]. In a meta-analysis, among the included 397 patients with free-floating right-heart thrombus and PE, dyspnea was the main presenting symptom [17].
Last, a syncope (i.e. transient loss of consciousness) can be the chief complaint for PE suspicion. Despites recent controversies, it is estimated that PE should be considered in patients with a syncope even in the absence of chest pain or dyspnea (with a reported prevalence of 2.2%) [19]. Another clinical sign that can increase awareness for physicians is tachycardia, which is present in about 45% of patients [20], and hemoptysis has been also associated with a higher risk of PE [17,19,21,22]. However, other atypical presentations have been described such as abdominal pain [23].
The notion of overtesting
Since the introduction of chest tomographic pulmonary angiogram (CTPA) in the early 2000s, the possibility of assessing patients for PE with a noninvasive study has exponentially increased the number of procedures performed to rule out PE. This rise in the use of chest imaging was described in 2011, with a twofold increase in the CTPA use, without any improvement in overall PE prognostic ation [24]. This led to the notion of overtesting and overdiagnosing. In addition to excessive resource use, this may lead to the avoidable initiation of anticoagulant drugs, with subsequent risk of adverse events [25]. In order to reduce this, several clinical decision rules (CDR) have been derived and validated. However, despite these, a recent large retrospective time series analysis confirmed the continuous rise in the use of CTPA [26]. Overall, despite controversies on the real prevalence of PE in the ED, less than 10% of patients that are investigated in the ED are ultimately diagnosed with a PE [27–30].
Diagnosis strategies
Definitive diagnosis of PE relies on thoracic imaging, mainly with CTPA or ventilation-perfusion (V/Q) lung scintigraphy. CTPA is often preferred over V/Q scan because of its better sensitivity (94% vs 56%–98%), its ability to identify differential diagnoses and its better availability [17,31,32]. Pulmonary angiography, the former gold standard for PE diagnosis, has no place in the diagnostic strategy, as its performance is equivalent to CTPA and requires more resource use.
The diagnostic approach to PE can be differentiated based on the hemodynamic status of the patient, which can be categorized into hemodynamically unstable and stable states. In hemodynamically unstable patients, the diagnostic process needs to be swift and may often involve the use of bedside echocardiography or CTPA, if the patient's condition allows and to initiate life-saving treatment [33].
As the spectrum of symptoms of PE is wide, and the morbidity/mortality associated with undiagnosed PE is substantial, clinicians must maintain a low suspicion threshold for deciding to start a PE diagnosis workup. Several diagnostic algorithms have been developed over the past decades in order to refine the indication of chest imaging studies in a Bayesian approach, i.e. the result of a test (posterior probability) is interpreted using prior information (pretest probability).
The performance of a diagnostic strategy is defined in terms of safety (number of patients in whom PE has been initially ruled out with no subsequent diagnosis of thromboembolic event) and efficiency (number of patients in whom the need for a chest imaging was reduced). The International Society on Thrombosis and Hemostasis (ISTH) [34] suggested to consider a strategy as safe if its failure rate is between 1.85% to 2% (depending on the overall prevalence of PE). This threshold for confirming the safety of a diagnostic approach is however subject to controversies. The definition of the “failure rate” is not consistent between studies and should be especially evaluated within the subpopulation of patients that underwent a change of management under the tested rule. A summary of the diagnostic strategy for PE in the ED is reported in Fig. 1.
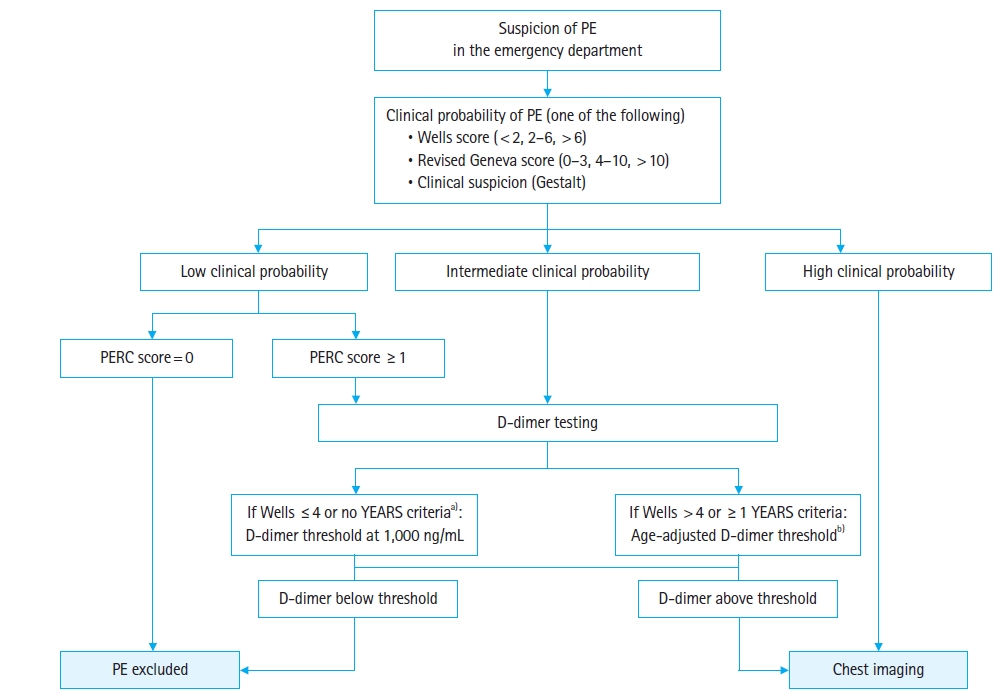
Diagnostic strategy for pulmonary embolism (PE) in the emergency department. Clinical probability of PE can be made upon structured choice (Wells score or revised Geneva score) or unstructured gestalt evaluation according to the practitioner’s choice. PERC, pulmonary embolism rule-out criteria. a)YEARS criteria: hemoptysis, clinical sign of deep venous thrombosis, opinion from the clinician that PE is the most likely diagnosis. b)Age-adjusted D-dimer threshold: ×10 ng/mL if age ≥50 years (for patients <50 years, D-dimer threshold is 500 ng/mL).
D-dimer assay
D-dimer is a biological marker, elevating in the presence of endogenous fibrinolysis, occurring during endovascular thrombosis as well as other inflammatory conditions (infection, cancer, etc.). D-dimer assay is therefore used to identify patients with a low probability of PE, among which PE can be ruled out without further exploration: at 500 ng/mL threshold, the sensitivity of D-dimer is estimated between 97% and 100% in the overall population suspected of PE [35,36].
However, the negative predictive value of D-dimer depends on the clinical probability, i.e., the probability of PE given clinical predictors, prior to D-dimer testing, this is due to Bayes theorem: at equivalent D-Dimer levels, the negative predictive value decreases as the pretest probability increases. Therefore, it has been suggested that in the case of a high clinical probability, D-dimer testing may not have sufficient negative predictive value to rule out PE, although this is based on very low level of evidence. The historical D-dimer threshold for ordering a chest imaging is 500 ng/mL, but it has been validated that in patients aged 50 years and older, this threshold can be raised to age×10 ng/mL [37].
D-dimer interpretation using CDR
There are three main approaches to clinical probability evaluation of PE. Clinical probability of PE can be made upon structured choice (Wells score or revised Geneva score) or unstructured gestalt evaluation according to the practitioner’s choice.
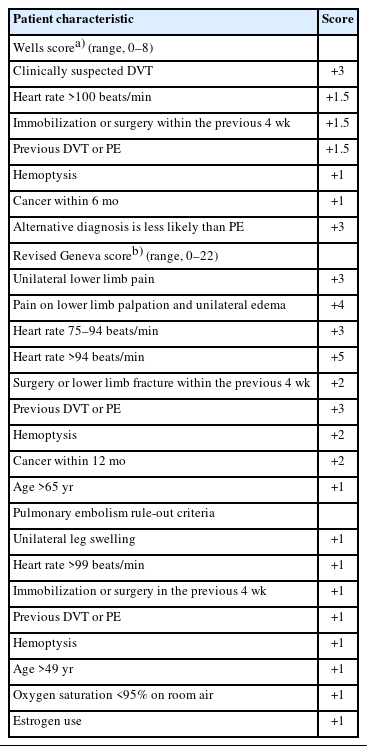
The Wells score identifies three groups of patients with low (<15% if score is <2), intermediate (15%-40% if score is 2–6), or high (>40% if score is >6) probability of PE, using clinical predictors: DVT signs, heart rate, immobilization, history of thromboembolism, hemoptysis, cancer, and presence of at least one (subjective item) more likely alternative diagnosis [28,38].
The revised Geneva score relies on only objective items: unilateral lower limb pain, presence of unilateral limb oedema, heart rate, immobilization, history of PE, hemoptysis, cancer, and age to identify the same three groups (low if score is 0–3, intermediate if 4–10, high if greater than 10) (Table 1).
Finally, an unstructured estimation of the clinical probability (clinical gestalt), i.e., an impression of whether the probability is low, moderate, or high has showed similar performance than the score-based approaches [38], although dependent on clinician’s experience [39].
Determining the optimal threshold of D-dimer
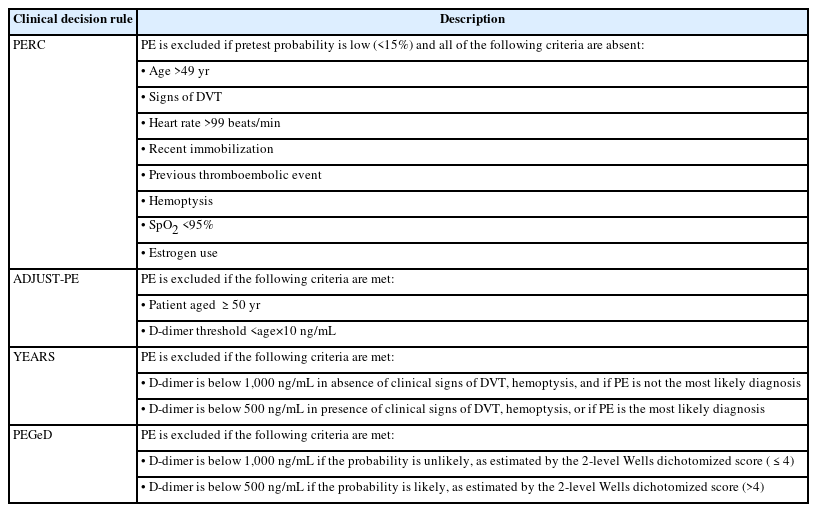
To limit the constant increase in use of chest imaging, several CDR have been validated to alleviate the need for imaging, either by ruling out PE on clinical signs, or by raising D-dimer thresholds for the lowest prior probabilities. A summary of the validated CDR is reported in Table 2.
As it is the case for early exclusion of acute coronary syndrome suspicion, a clinical decision rule can also identify patients with a very low probability of PE in whom PE can be safely excluded without the need for further investigation [40]. The pulmonary embolism rule-out criteria (PERC) include age of 50 years or greater, heart rate over 100 beats/min, pulse oximetry below 95%, unilateral leg swelling, hemoptysis, recent surgery or trauma, prior PE or DVT, and hormone use (Table 1) [28,41]. The absence of all of these criteria allows to safely rule out PE, without the need of further testing [29].
The YEARS algorithm may allow elevating the D-dimer to 1,000 ng/mL threshold in absence of hemoptysis, signs of DVT, and if at least another diagnosis is more likely; and 500 ng/mL if one of these criteria is absent, with a failure rate of 0.5% [42,43].
The PEGeD (Pulmonary Embolism Graduated D-Dimer) algorithm uses the two-level dichotomized Wells score to define a D-dimer threshold of 1,000 ng/mL [37,44]. PE is excluded if D-dimer is below 1,000 ng/mL if the clinical probability is unlikely (two-level Wells score ≤4). D-dimer is below 500 ng/mL if the clinical probability is likely, as estimated by the two-level Wells score (>4).
Clinical application and combination of rules
Whether these different CDR can be combined remains controversial, although a large randomized controlled trial confirmed that YEARS can be safely combined with PERC and age-adjusted D-dimer threshold [30]. Furthermore, a post hoc analysis of two European cohort studies confirmed the safety of these, with acceptable failure rates of PERC+YEARS and PERC+PEGeD algorithms of 0.75% (95% confidence interval [CI], 0.51%–1.10%) and 0.87% (95% CI, 0.61%–1.25%), respectively [45].
As an alternative to rule combination, a global algorithm has been published by Roy et al. [46], using a one-step clinical decision rule and determining four levels of clinical probability. The very low level identifies patients in whom PE can be ruled from clinical predictors only, allowing patient discharge without D-dimer assay. The low and intermediate levels require a D-dimer value below 1,000 and 500 ng/mL, respectively, to allow discharge without imaging. The highest level requires imaging without a D-dimer assay. In the validation cohort, the reported failure rate was 0.8% (95% CI, 0.5%–1.2%), with a reduction of the number of imaging between 19% and 22% [47].
Although safe and efficient these CDR may have a limited applicability in routine practice by emergency physicians, who might be reluctant to use several score with numbers of items. Therefore, a simplified strategy has been introduced that allow to raise the D-dimer threshold in all patients in whom the treating emergency physician consider that “PE is not the most likely diagnosis.” Two retrospective studies have suggested that this strategy may be safe [43,48]. The simplicity of such approach could enhance physicians’ adherence.
Specific populations
Several patients’ profiles require particular consideration for the diagnosis of PE. This may result from their exclusion from studies that have derived and validated current tools, sometimes involving the design of specific tools, or from pathophysiological hypotheses that may justify adapting the weighting of scores or D-dimer thresholds, or taking into account other specific risk factors.
Pregnant patients
It has been reported that pregnancy is a prothrombotic state that increases the risk of thromboembolic events. It is the leading cause of maternal mortality in the United Kingdom, with an estimated rate of between 0.71 and 1.59 per 100,000 between 2010 and 2012 [49,50]. Most clinical signs can be partly caused by the physiological course of pregnancy (dyspnea, tachycardia, pain). Furthermore, the interpretation of D-dimer levels is more difficult because they are physiologically elevated in pregnant patients. Therefore, the threshold for imaging test may need to be tailored.
Most CDR have excluded pregnant or postpartum women from study populations. An adapted version of the YEARS algorithm was studied in pregnant patients [51]. In this study, performance of YEARS for pregnant women showed a failure rate of 0% (95% CI, 0%-2%), with CTPA avoided in 65% (95% CI, 54%–75%) among women in the first trimester of pregnancy, and 46% (95% CI, 39%–53%) in the second trimester. Of note, there is no indication to perform lower leg compression ultrasonography in the absence of clinical signs of DVT.
Younger patients
The incidence of PE decreases with age. Therefore, there may be a lower rate of positive chest imaging studies [52]. Furthermore, tachycardia does not appear to be a predictor in this population, while hyperthermia is reportedly associated with increased risk of PE. It therefore seems reasonable to adapt diagnostic tools to take account of this a priori lower probability on the one hand, and of these specific predictors on the other. Mongan et al. [52] have thus proposed adapting the PERC criteria to this subpopulation, by integrating temperature and removing tachycardia. This “PERC-35” rule has been validated in two retrospective cohort studies [52,53].
COVID-19 patients
During the first wave of COVID-19 epidemic, there were concerns on a potential increased risk of PE in patients with SARAS-CoV2 infection [54]. However, a large retrospective study reports that COVID-19 was not an independent risk factor for thromboembolic events in ED patients with suspicion of PE [55].
Cancer patients
Cancer is a known risk factor for PE but can also increase D-dimer levels despite absence of thromboembolism. Cancer patients with PE have a higher in-hospital mortality [56]. Actual CDR appear to be valid in this population, according to a recent meta-analysis of individual patient data [57]. The diagnostic workup for PE should remain unchanged in patients with cancer.
PERSPECTIVES
The definition of the acceptable failure rate is subject to debate, involving medical, social, and ethical considerations. A unique acceptable failure rate relies on equity principle but implies inequity for other factors such as years of healthy life, which would mean adjusting the acceptable false-negative threshold for age and comorbidities. Furthermore, such an approach can lead to apparently paradoxical situations, such as in younger patients, where the probability of PE could be excluded from age only, as the probability of PE is very low in this population.
Improving the accuracy of models for specific population subgroups is also necessary for the fairness of clinical rules. In particular, a diagnostic strategy may perform well and be balanced overall, although this performance may be heterogeneous, i.e., too restrictive for one subgroup, and too unreliable for another. However, recent results do not seem to show such heterogeneity [57].
It is of utmost importance that the failure rate definition should be consistent within different diagnostic studies to validate the safety of an algorithm. The most clinically relevant definition for “failure rate” would be the number of missed PE divided by the number of patients in whom PE was initially ruled out among patients in whom the strategy has been effectively applied. For example, a study evaluating the PERC rule should consider the “false-negative rate” as the number of patients with PE and PERC=0, and a study evaluating the YEARS rule should consider the “false-negative rate” as the number of PE at follow up in patients in whom PE as initially ruled out, among patients that did not undergo D-dimer testing because of the YEARS rule (i.e., patients with YEARS=0 and D-dimer >500 and <1,000 ng/mL).
CONCLUSION
PE diagnosis workup illustrates the complexity of modern probabilistic-based approaches of decision-making in medicine. A number of recent research projects have improved the performance of diagnostic tools for PE, through better integration of clinical information, improved performance of imaging tests, and more effective CDR using a rational probabilistic approach, thereby reducing the number of tests required for diagnosis while maintaining acceptable safety. It is recommended to use a Bayesian approach with the evaluation of clinical probability, then order D-dimer if the PERC rule is positive, then adapt the D-dimer threshold for ordering chest imaging using the YEARS, PEGeD, or PE likely CDR.
Despite these recent validated CDRs, reports suggest that this may not have translated in routine practice and has not resulted in the reduction of chest imaging use. There is therefore a need for a more practical approach that can have easier application for emergency physicians.
Notes
Author contributions
Conceptualization: DT, YF, PC; Investigation: all authors; Methodology: all authors; Validation: DT; Writing–original draft: all authors; Writing–review & editing: all authors. All authors read and approved the final manuscript.
Conflicts of interest
The authors have no conflicts of interest to declare.
Funding
The authors received no financial support for this study.
Data availability
Data sharing is not applicable as no new data were created or analyzed in this study.
References
Article information Continued
Notes
Capsule Summary
What is already known
The optimal diagnosis strategy for pulmonary embolism (PE) in the emergency department remains complex. Definitive diagnosis of PE relies on thoracic imaging, mainly with chest tomographic pulmonary angiogram or ventilation-perfusion lung scintigraphy. In order to reduce the exponential increase of chest tomographic pulmonary angiogram to rule out PE, several clinical decision rules have been derived.
What is new in the current study
PE symptoms are nonspecific and very diverse, justifying consideration of this hypothesis in a wide range of clinical situations including chest pain, syncope, shortness of breath, hemoptysis, and tachycardia. PE diagnosis workup illustrates the complexity of modern probabilistic-based approaches of decision-making in medicine. A number of recent research projects have improved the performance of diagnostic tools for PE, through better integration of clinical information, improved performance of imaging tests, and more effective clinical decision rules using a rational probabilistic approach, thereby reducing the number of tests required for diagnosis while maintaining acceptable safety. This review summarizes PE diagnosis with clinical presentation, new decision rules and investigations for acute PE in the general population or in specific populations (pregnant patients, younger patients, COVID-19 patients, or cancer patients) in the emergency department.