Large observational study on risks predicting emergency department return visits and associated disposition deviations
Article information
Abstract
Objective
A common emergency department (ED) patient care outcome metric is 72-hour ED return visits (EDRVs). Risks predictive of EDRV vary in different studies. However, risk differences associated with related versus unrelated EDRV and subsequent EDRV disposition deviations (EDRVDD) are rarely addressed. We aim to compare the potential risk patterns predictive of related and unrelated EDRV and further determine those potential risks predictive of EDRVDD.
Methods
We conducted a large retrospective observational study from September 1, 2015 through June 30, 2016. ED Patient demographic characteristics and clinical metrics were compared among patients of 1) related; 2) unrelated; and 3) no EDRVs. EDRVDD was defined as obvious disposition differences between initial ED visit and return visits. A multivariate multinomial logistic regression was performed to determine the independent risks predictive of EDRV and EDRVDD after adjusting for all confounders.
Results
A total of 63,990 patients were enrolled; 4.65% were considered related EDRV, and 1.80% were unrelated. The top risks predictive of EDRV were homeless, patient left without being seen, eloped, or left against medical advice. The top risks predictive of EDRVDD were geriatric and whether patients had primary care physicians regardless as to whether patient returns were related or unrelated to their initial ED visits.
Conclusion
Over 6% of patients experienced ED return visits within 72 hours. Though risks predicting such revisits were multifactorial, similar risks were identified not only for ED return visits, but also for return ED visit disposition deviations.
INTRODUCTION
Emergency department return visits (EDRV) are considered a measure of patient safety. Higher EDRV rates indicate negative patient care outcomes [1-3]. Some studies focused on EDRV within 72 hours report increased morbidity and hospital readmission among the revisit group [4,5] while others reported similar disease patterns and hospital admissions in comparison to patients with no 72 hours EDRV [6,7].
To better understand patients experiencing emergency department (ED) returns, potential risks predictive of such returns have been extensively studied [8-10]. Of note, a variety of potential risks were identified among the different studies. Three common risk categories identified in these studies are illness, patient, and provider/system related factors [11]. Illness-related risks focus on different diseases or complaints posing higher risk of EDRV. Examples are abdominal pain, cancer, alcohol/drug abuse, psychiatric/chronic disease conditions, etc [9,10,12]. These high-risk potential EDRV are typically thought to be related to initial ED visits. However, direct supporting evidence is generally lacking. Patient-related risks mainly address patient specific characteristics (age, sex, insurance type, etc.) [13-16] and provider/system-related risks identify healthcare systems issues (provider characteristics, completion of discharge instructions, ED crowding, etc.) [17-19]. Previous studies focusing on the latter two types of risks neither differentiate whether EDRV are related to the initial ED visits nor do they specifically identify risks predictive of a relationship between EDRV and the initial visit. Uncertainty remains as to whether EDRV truly alters patient disposition and potential risks predictive of such disposition deviations from initial ED visits.
Simply determining risks predictive of EDRV without knowing whether these visits are related to the initial visit is insufficient in terms of establishing the predictive value of future interventions unless these risks are identical. Additionally, interventions might not be sufficient without knowing any potential significant disposition deviations that occur among ED return visits. Therefore, we aim to determine 1) the potential risks predictive of 72 hours related EDRV among all discharged ED patients and 2) the potential risks predictive of ED disposition deviations among all EDRV patients.
METHODS
Study design and setting
This is a retrospective, observational, single-center study. All data were retrieved from electronic health records visits covering the period September 1, 2015 through June 30, 2016. The study setting is an urban ED with annual patient visits >120,000. The institutional review board of John Peter Smith Health Network approved this study (010713.004ex). Due to retrospective chart review with no more than minimal risk to the subjects and the research could not practicably be done without a waiver of consent, this study was approved with the waiver of the written informed consent.
Participants
We included all patients presenting to the study hospital ED that 1) were discharged, 2) left without being seen (LWBS), 3) left against medical advice (AMA), and 4) eloped during the initial ED visits. Patients who visited the ED multiple times during the study period were considered as different patient encounters. We excluded 1) patients that expired at the initial ED visits, 2) patients admitted to hospital during the initial ED visits, 3) patients transferred to other facilities during initial ED visits, and 4) prisoners.
Variables
Patients who visited the study ED within 72 hours from the index ED visits were considered EDRV. Those who did not visit the study ED within 72 hours from the index visits were considered the no-return group. Two individual ED physicians, blinded to the study’s purpose, reviewed enrolled patient charts to determine whether EDRV were related or unrelated to the initial ED visits. To resolve discrepancies, a second round of reviews were rendered at least 30 days apart from the previous review. Repeated reviews occurred until a strong level of interrater agreement was reached.
Potential independent risks predictive of ED returns were divided into three categories: patient-related risks, system/provider-related risks, and illness-related risks. Potential patient-related risks included age, sex, race/ethnicity, mode of arrival, insurance type, and homeless status. Mode of arrival was divided into three categories: 1) healthcare assisted transportation (ambulance ground transportation, flight, and hospital assisted transportation); 2) private transportation (private car or taxi); and 3) public/other transportation (public vehicle, ambulatory, and wheelchair). Insurance type was divided into three categories: 1) government/charity (Medicaid, Medicare, and other national/local charity insurance plans); 2) private commercial insurance; and 3) no insurance. Potential system/provider-related risks included initial total ED length of stay, initial ED disposition, and whether patients had their primary care physician assigned upon initial ED visit. Initial ED dispositions were further divided into two categories, including discharge and disposition with uncertainty, a combination of eloped, AMA, and LWBS either before or after triage completion. Potential illness-related risks included level of acuity as determined by the 5-point Emergency Severity Index, history of alcohol or substance abuse, psychiatric conditions, acute injury, and whether patients had discharge medications prescribed during the initial ED visits. Psychiatric conditions included patients with history of depression, anxiety, mania, schizophrenia, schizoaffective disorder, and bipolar disorder. Acute injury was defined as patients presenting to the ED with acute traumatic injury including, but not limited to, any type of trauma, stab wound, gunshot wound, laceration, and fracture/dislocation.
Outcome measurements
EDRV was categorized as related or unrelated EDRV. The primary outcome was to determine the risks predictive of related 72-hour EDRVs. The secondary outcome was to identify significant EDRV disposition deviation (EDRVDD) and further determine risks predictive of EDRVDD. Significant EDRVDD was defined as an obvious disposition difference between initial ED visit and return visit. Such disposition deviations included hospital admissions, hospital observation, patient expiration during EDRV, or operation room admission. Non-significant ED disposition deviation was defined as patients discharged during return visits. Uncertain ED disposition deviation included patients that eloped, left AMA, LWBS, and those transferred to other services or facilities during EDRV.
Data sources
All data, except for related versus unrelated EDRV determination, were retrieved by persons from the hospital’s information technology department who were blinded to the study’s outcomes. To assess internal validation, twenty random samples were selected at three separate phases. As this is an epidemiological observational study, sample size estimation is not considered necessary per study design.
Study protocol
After individual physicians rendered intensive chart reviews, interrater variability was tested to determine consistency with respect to determination of 72 hours EDRV. Patients were initially divided into three groups: 1) patients with no EDRV, 2) patients with 72 hours related EDRV, and 3) patients with 72 hours unrelated EDRV. Potential risk variables were compared among the three groups. Risks predictive of patient 72 hours EDRV (both related and unrelated) were analyzed. Additionally, among all EDRV patients, those with significant EDRVDD were analyzed separately. Risks predictive of significant EDRVDD were compared between related and unrelated EDRV patients.
Data analysis
The kappa test was used for interrater variability analysis with κ >0.8 indicating a strong level of agreement. The analysis of variance was used for continuous data comparisons among the three different groups and the Pearson chi-square test was used for categorical data comparison. We used multivariate multinomial logistic regression models to examine the relationship between the predictors and the outcomes of interest [20]. We classified our primary outcome into three categories: no return, related return, and unrelated return. Predictors included age, sex, race/ethnicity, mode of arrival, primary care provider assignment, level of acuity, insurance type, homelessness, history of alcohol abuse, history of substance abuse, history of psychiatric conditions, ED length of stay, ED medication prescription upon discharge, and whether patients had acute injuries. The secondary outcome was classified into three categories: no disposition deviation, uncertain disposition deviation, and significant disposition deviation. All predictors included in the primary outcome analysis were included in this secondary outcome model prediction with the addition of two variables (return mode of arrival and return triage level of acuity). Diagnostic tests for collinearity and potential variable interactions were performed among predictor variables. Our final model was selected based on Likelihood Ratio Tests, Akaike Information Criterion and Bayesian Information Criterion values. All analyses were performed using Stata ver. 14.2 (StataCorp., College Station, TX, USA) with P-value <0.5 considered statistically significant.
RESULTS
General information
A total of 63,990 patient encounters were enrolled in this study comprising 43,809 unique patients. A detailed interpretation of patient information is provided in Table 1. Two rounds of provider reviews were performed to determine whether EDRV were related to initial ED visits. Interrater agreement was 0.74 (first round, P<0.05) and 0.93 (second round, P<0.05), indicating a strong level of agreement between providers. Additional electronic health record reviews were stopped after the second round of reviews. Among all enrolled patient encounters, 6.45% (4,130) were 72 hours EDRV; 4.65% (2,976) were determined related EDRV and 1.80% (1,154) were considered unrelated. Briefly, return patient characteristics consisted primarily of male, geriatric, homeless patient populations with government/charity funded insurance. These patient encounters also had a higher incidence of history of alcohol or drug abuse and psychiatric conditions. Subsequently, all EDRV patients were included in a subgroup study. Analysis of this subgroup found 21% (873) of patients had significant EDRVDD while 71% (2,944) had no disposition deviations (Table 1).
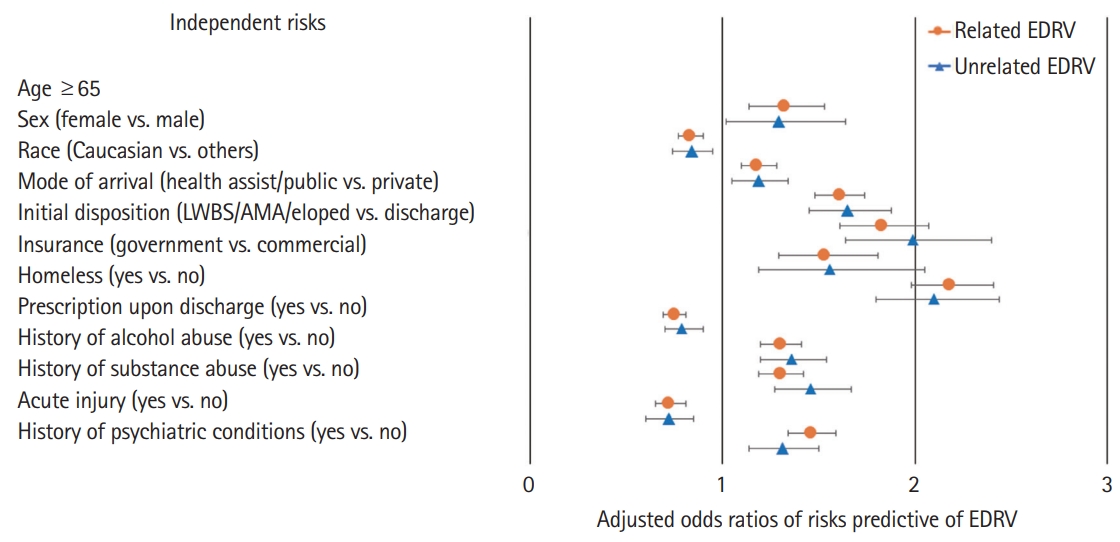
Risks predictive of ED returns
After adjusting for all potential risks, it was found that there were nine independent risks favoring EDRV: geriatrics; non-Caucasian races; homelessness; initial ED visit LWBS/AMA/eloped; history of alcohol or substance abuse; psychiatric conditions; patients with government/charity insurances; and mode of arrival to the ED other than private car or taxi (e.g., healthcare assisted or public transportation). Female patients with acute injuries and medications prescribed upon ED discharge were considered having relatively less risks for ED returns (Fig. 1 and Supplementary Table 1). More importantly, risks predictive of related and unrelated EDRV were very similar (Fig. 1).
Risks predictive of significant ED return disposition deviations
After adjusting for all potential confounders, the three independent risks that predicted more significant EDRVDD were: geriatric age, patients with primary care physician assigned, and longer ED length of stay during EDRV as compared to initial visit. Three risks predicted less significant deviations: mode of arrival to the ED (public or other transportation); homelessness; and patient triaged with lower level of acuity (Fig. 2 and Supplementary Table 2). Overall, these independent risks predicted significant EDRVDD regardless of its relation (related vs. unrelated) to the initial ED visits.
DISCUSSION
It is well known that risks predictive of EDRV are multifactorial and may vary among different patient populations [21,22]. Our findings showed similar risks predictive of EDRV despite association (related versus unrelated) with the initial ED visits. This relationship factor has not been previously reported in the literature [14,21,23]. Additionally, this study further emphasizes disposition deviations among EDRV patients and identifies different risk prediction models which are infrequently found in previous studies. More importantly, similar risk patterns are again revealed regarding the ED disposition deviation predictive model despite its link to initial ED visits. Based on our predictive models, though EDRV patients are a different patient population in comparison to patients with no returns, related and unrelated EDRV patients can be categorized into one group for future quality improvement interventions. Since all EDRV patients might be affected by the same risk patterns, we suggest that further differentiating EDRV patients with respect to related versus unrelated return visits might not be necessary.
Specific study methodology was used in this study. Stepwise sequential interrater agreement performed in this study, though subjective and time consuming, demonstrates less bias regarding determination of related versus unrelated EDRV, similar to the modified Delphi technique [24]. Additionally, further identifying risks predicting related versus unrelated EDRV and EDRVDD using a multivariate multinomial logistic regression model provided us an optimal analytic method to minimize confounding biases while allowing more appropriate outcome categorizations than a traditional multivariate logistic regression model with binary outcomes [20].
We identified over 6% of patients experiencing 72 hours EDRV which is similar to those previously reported [5,8,14,25]. Most EDRV predictive risks identified in this study have been reported in other studies demonstrating consistent findings [14,16,26-28]. Among all risks predictive of EDRV, homelessness and patient LWBS/AMA/eloped dispositions were among the top two contributing factors. Many previous studies identified subgroups of patient populations (e.g., patients with high psychosocial risks) that tended to have higher EDRV whose general characteristics matched well with our top risks in this study [12,26,28-30]. All potential independent risks also fit well into three major risk areas (patient, illness, and system/provider related) thus further confirming such risks being multifactorial.
Similar risk patterns were noted between related versus unrelated EDRV subgroups indicating that it is unnecessary to differentiate related and unrelated EDRV. It is well known that geriatric patients and patients with higher level acuity presentations tend to have higher frequency disposition deviations when comparing index to return visits [27]. Geriatric patients have greater potential for severe disease progression despite subtle symptoms presentation at the initial ED visit. Patients with higher level acuity presentations usually indicate more emergent/severe disease patterns requiring further evaluation [21,27]. This might explain how common ED provider behavior (e.g., universal high-risk potential consideration among all EDRV patients) influences EDRV patient dispositions although we are unable to provide direct evidence for such linkage in this study. Moreover, no significant management deviation was noted among non-geriatric, homeless patients with lower acuity level presentations.
Our findings indicate that EDRV patients are a special patient population and the risks predictive of EDRV and EDRVDD are multifactorial. Such findings provide some indirect evidence for future interventions in this special patient population such as, but not limited to, minimizing EDRV by applying out-of-hospital outreach programs or urgent primary care physician follow up for low acuity, homeless, or non-geriatric EDRV patients since their management is rarely altered. However, lacking direct evidence of such linkage, a prospective observational study with large sample size is warranted for external validation.
In summary, over 6% of patients experienced EDRV within 72 hours of initial ED visit. Though risks predicting such revisits were multifactorial, similar risks were identified for both EDRV and EDRVDD regardless of whether EDRV was related versus unrelated to initial visit. Therefore, it is reasonable to consider EDRV as a single entity in terms of patient care outcome measurements in future studies.
This is a single-center retrospective study which cannot demonstrate causality due to limited information accuracy and potential selection bias. Second, we enrolled all EDRV patients at the study ED but are unable to identify and enroll ones that might have visited other EDs within 72 hours of index visit to the study ED. Third, though high fidelity was observed between individual reviewers regarding determination of related versus unrelated EDRV, we were unable to completely rule out case-by-case inaccuracy due to lack of a gold standard. Furthermore, as risks predictive of EDRV or EDRVDD are multifactorial, we may have overlooked other potential risks not considered in this study. Fourth, homeless patients tended to have high psychosocial risks and their ED return pattern might be different than the general patient population. In this study, we did not investigate ED return and disposition deviation risks in detail among homeless patients which could generate potential patient selection bias. Finally, considering ED disposition deviations as a singular end-point may be short-sighted thereby excluding additional potential clinically relevant data that might be associated with an extended investigation incorporating in-hospital morbidity, mortality, and/or short-term progress reports following hospital admission which might be linked to EDRV. Future studies should be carried out investigating more robust network data to include large regional and/or national samples analyzing extended outcomes.
SUPPLEMENTARY MATERIAL
Supplementary Tables are available from: https://doi.org/10.15441/ceem.18.024.
Supplementary Table 1. Risk factors predictive of 72-hour emergency department return visits
Supplementary Table 2. Risk factors predictive of ED significant disposition deviations
Notes
No potential conflict of interest relevant to this article was reported.
References
Article information Continued
Notes
Capsule Summary
What is already known
Risks predictive of emergency department return visits are multifactorial.
What is new in the current study
Though risks predicting such revisits were multifactorial, similar risks were identified not only for emergency department return visits, but also for return emergency department visit disposition deviations regardless of the link between initial and return visits.