Study on the effect of a cold environment on the quality of three video laryngoscopes: McGrath MAC, GlideScope Ranger, and Pentax Airway Scope
Article information
Abstract
Objective
Several environmental factors influence the prehospital use of video laryngoscopes (VLs). For example, fogging of the VL lens can occur in cold environments, and the low temperature can cause the VLs to malfunction. As relevant research on the effect of environment on VLs is lacking, we aimed to study the effect of a cold environment on three commonly used VLs.
Methods
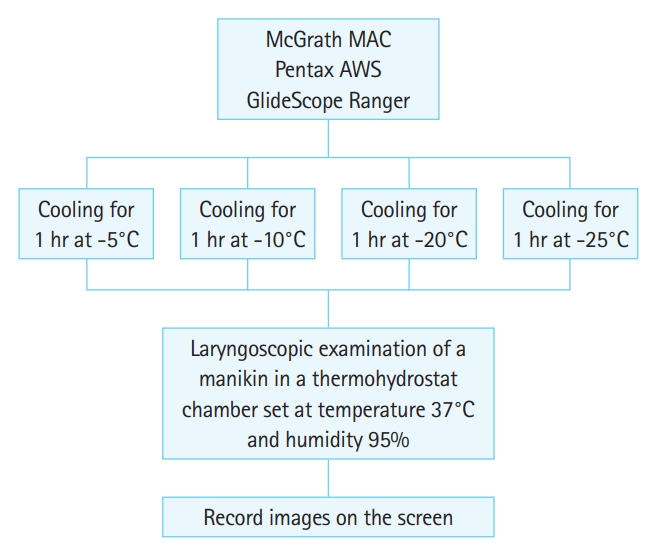
McGrath MAC, Pentax Airway Scope (AWS), and GlideScope Ranger were exposed to temperatures of -5°C, -10°C, -20°C, and -25°C for 1 hour each and then applied to a manikin in a thermohydrostat room 5 times. Immediately after turning on the power and inserting the blade, the time until an appropriate glottic image appeared on the screen was measured.
Results
McGrath MAC was able to accomplish immediate intubation regardless of the temperature drop. However, GlideScope Ranger required an average of 4.9 seconds (-5°C to -20°C) and 10.1 seconds (-25°C) until appropriate images were obtained for intubation. AWS showed adequate image acquisition immediately after blade insertion despite slight fogging at -20°C, but at -25°C, images suitable for intubation did not appear on the screen for an average of 4.7 minutes.
Conclusion
All three devices appear to be usable without any limitations up to -20°C. However, GlideScope Ranger and AWS may not produce images immediately at temperatures below -25°C. Thus, medical practitioners performing VL in a cold environment should be aware of the characteristics of the VL devices in advance.
INTRODUCTION
Several attempts have been made to evaluate the usefulness of video laryngoscopes (VLs) in the prehospital setting; however, disappointingly, VLs did not show superiority to direct laryngoscopes in the prehospital setting [1-5]. The main reason for this is that prehospital intubators lack experience with VLs; the results might have been different if there had been much more experience and knowledge on prehospital VL use [4,6]. Therefore, continuous research is needed to identify and overcome various constraints with regard to the use of VLs in prehospital settings [7]. Environmental challenges can affect the intubation ability of intubators [3,4]. Until now, there has been one study on the effect of light reflection by sunlight on screen visibility; however, there is little information on how cold temperatures affect the screen visibility of VLs [8]. At low temperatures, there is a high risk of fogging of the lens and transparent blades because of condensation. Moreover, the lower the temperature, the worse the fogging becomes and the longer it lasts. In addition, at cold temperatures, the device may malfunction. The purpose of this study was to investigate the effects of cold temperatures on the operation and fogging of three commonly used VLs.
METHODS
This study is a prospective, simulated manikin study. An Ambu Airway Management Trainer (Ambu Corp., Copenhagen, Denmark) was placed in a thermohydrostat room set at a temperature of 37°C and 95% humidity, similar to the conditions of the human throat. We selected three devices commonly used in prehospital environments for our experiments: McGrath MAC (Aircraft Medical, Edinburgh, UK), GlideScope Ranger (Verathon, Bothell, WA, USA), and Pentax Airway Scope (AWS) (Pentax Corporation, Tokyo, Japan). We exposed all 3 VLs to temperatures of -5°C, -10°C, -20°C, and -25°C for one hour at each temperature by placing them in a refrigerator (Fig. 1). Then, the VLs were taken out of the refrigerator and immediately powered on, following which they were inserted into the airway management model in the thermohydrostat room and images on the screens of the VLs were recorded. The images from the three VLs were then compared by two emergency physicians. The images appearing on the screen were recorded for at least 30 seconds and were further recorded if necessary to ensure appropriate glottic view for intubation. The same experiment was repeated 5 times to check whether the image on the screen was the same among the experiments.
We investigated whether fogging occurred on the screen and measured the time from when the VLs were switched on until one emergency specialist determined that the glottis structure was identifiable enough to allow intubation. Before the experiments, anticondensation solution was applied onto the liquid crystal display (LCD) surface of the VLs.
This study was approved by the institutional review board of Hanyang University Guri Hospital (2017-05-21).
RESULTS
With both McGrath MAC and GlideScope Ranger, lens fogging occurred at all temperatures, beginning just after the insertion of the laryngoscope blade. The degree of fogging with McGrath MAC was mild enough to identify the anatomical structure of the glottis, and the same level of fogging was maintained for over 30 seconds (Fig. 2). On the other hand, lens fogging on using GlideScope Ranger was so heavy just after insertion of the blade that the anatomical structure of the glottis could not be identified at all (Fig. 3). The mean time required for the visual field of GlideScope Ranger to improve enough to identify the anatomical structure was 4.9 seconds (standard deviation [SD]±0.08 seconds) at -5°C, -10°C, -20°C, respectively, and 10.1 seconds (SD±0.05 seconds) at -25°C. The mean time taken for fogging to completely disappear from the GiideScope Ranger screen was 9.8 seconds (SD±0.07 seconds) at -5°C to -20°C and 4.7 minutes (SD±0.13 minutes) at -25°C. With Pentax AWS lens fogging hardly occurred at -5°C to -20°C. However, at -25°C, Pentax AWS did not show any image on the screen for an average of 4.7 minutes (SD±0.04 minutes); the first recorded glottic image was sufficient for intubation, although there was some fogging (Fig. 4). For all VLs, as condensation occurred only slightly on the LCD surface, it did not affect the visual field.

Images from McGrath MAC, immediately after blade insertion (A) and 30 seconds after blade insertion (B) in cold temperatures (-5°C to -25°C).

Images from GlideScope Ranger in cold environments. Image changes after blade insertion (A,B) at -5°C, -10°C and -20°C and image changes at -25°C (C,D).
DISCUSSION
VLs use a lens to provide a good glottic view; however, when the lens is dirty or clouded, vision through the lens is obstructed. Lens fogging is also a phenomenon that can interfere with glottis observation. When equipment mounted with lenses that have been used in cold environments are exposed abruptly to warm environments, condensation of moisture on the surface of the lens occurs because of the temperature differences between the environments. Therefore, it can be assumed that the fogging rate, severity, and duration will increase as the temperature difference increases. Fogging can be a major obstacle when intubation is needed in a cold outdoor environment. Although there have been few studies on lens fogging at room temperature, there have been no studies in low-temperature environments, and the manufacturers of the VLs do not provide data regarding the phenomenon of fogging. One study using GlideScope Ranger in an indoor setting reported that lens fogging occurred in 59.5% of intubations with disposable blades and 33.3% of intubations with conventional blades; however, the severity was low [9].
In addition to lens fogging, cold temperatures can interfere with equipment operation. The manufacturers of GlideScope Ranger and McGrath MAC provide information regarding the optimal operating temperature of the devices. According to the manufacture’s information, GlideScope Ranger can operate at temperatures of up to -20°C. In this study, GlideScope Ranger was found to be operational at temperatures as low as -20°C. However, it was difficult to identify the glottic opening for approximately 5 seconds after turning on the power because of lens fogging. The antifogging mechanism of GlideScope Ranger involves heating of the lens, and the 5-second delay is because of the time it takes for the lens to heat properly [10]. Interestingly, from -5°C to -20°C, the lens took approximately 5 seconds to reach a proper viewpoint, compared with approximately 10 seconds at -25°C. However, even in environments that were 5°C below the operating temperature limit provided by the manufacturer, GlideScope Ranger operated normally after 10 seconds. Therefore, when attempting to intubate with GlideScope Ranger in a cold environment, it may be helpful to turn the power on for more than 10 seconds before inserting the blade. According to the manufacturer’s information, McGrath MAC can operate at 10°C to 40°C. In this study, however, the McGrath MAC operated normally at -25°C, and although there was significant fogging on the transparent blade, we could still identify the glottis structures. Therefore, we think that, among the three devices, McGrath MAC was the most reliable device for use in cold environments. The disposable blade of McGrath MAC is made of polycarbonate, which is resistant to fogging, but the lens has no separate antifogging mechanism. However, as the lens is not directly exposed to air, it is estimated that it is less likely to fog than the lens of GlideScope Ranger on exposure to air. In addition, the plastic housing of the device is presumed to better protect the internal components from degradation owing to temperature compared to that in other equipment. The manufacturer of Pentax AWS did not disclose any special operating conditions, and this VL showed slight fogging, allowing intubation as soon as the power was turned on up to -20°C. When the power was turned on at -25°C, the screen did not turn on; however, after approximately 5 minutes, it worked normally. Therefore, we believe that Pentax AWS is very reliable in cold environments up to -20°C, but at temperatures lower than this, it is necessary to check the operation before use.
There are some limitations to our study. First, there is a possibility of selection bias, as the three VLs were randomly assigned to four temperature environments. Second, the time to determine the glottis structure on the screen was assessed by one experienced researcher. Therefore, if the practitioner had less experience, the time required for intubation could be extended beyond the values reported in this study.
In this study, we tried to set the temperature and humidity of the manikin as close to that in humans as possible. In real intubation situations, only the lens and blade would be inserted into the warm and humid body; however, in this study, the entire device, including the LCD screen, was exposed to the warm and humid environment. Fogging can also occur on the LCD screen, possibly interfering with vision. However, in this study, an antifogging agent was applied to the LCD screen to minimize this effect.
In summary, in cold environments, fogging occurred in all three laryngoscopes but not enough to disturb intubation, and all devices worked well beyond the operating limits provided by the manufacturer. However, GlideScope Ranger required several seconds for the lens to heat up, and Pentax AWS did not work below the critical temperature. A practitioner who needs to use a VL in a cold environment should be aware of the characteristics of the device in advance.
Notes
No potential conflict of interest relevant to this article was reported.
References
Article information Continued
Notes
Capsule Summary
What is already known
There have been attempts to use video laryngoscopes in prehospital settings, but the results have not been satisfactory. A video laryngoscope with a lens can experience fogging in cold environments, and the electronics may not work properly due to the cold.
What is new in the current study
All three devices tested appear to be usable without any limits up to -20°C. However, the GlideScope Ranger and Pentax Airway Scope may not be immediately available at temperatures below -25°C.