Effect of percutaneous coronary intervention team prenotification based on real time electrocardiogram transmission in interhospital transfer of ST elevation myocardial infarction patients: pilot trial of Preparing Revascularization Effort before Patients’ Arrival via Regionalization Engagement protocol
Article information
Abstract
Objective
Prompt reperfusion is important for patients with ST elevation myocardial infarction (STEMI). However, patients often require interhospital transfer for percutaneous coronary intervention (PCI) because not all hospitals can provide. The purpose of this study is to reduce the PCI delay using a regionalization protocol in patients with STEMI following transfer from another hospital lacking PCI facility.
Methods
We established a revascularization protocol designated as Preparing Revascularization Effort before Patients’ Arrival via Regionalization Engagement (PREPARE) for the STEMI patients transferred from an outside regional hospital. The protocol included immediate referral acceptance by an emergency physician, real-time electrocardiogram sharing via mobile phone and early activation of the PCI team. We analyzed the differences between the PREPARE and the non-PREPARE groups.
Results
In the PREPARE group, the median time from the first hospital visit to the ballooning procedure via PCI at the receiving facility (D1-to-B time) was 111.0 (interquartile range 97.0– 130.0) minutes, which was significantly shorter than in the non-PREPARE group 134.0 (interquartile range 115.0–182.0) minutes. The proportion of D1-to-B time within 120 minutes was 30.4% in the group and 60.0% in the PREPARE group, which represents a significant difference (P=0.004). Multivariate logistic regression analysis revealed that patient transfer via PREPARE protocol (odds ratio, 3.399; 95% confidence interval, 1.150–10.050, P=0.027) was related to adequate D1-to-B time. No statistically significant differences were found in the hospital length of stay or major adverse cardiac events within 4 weeks.
Conclusion
The PREPARE protocol is an effective strategy to reduce the time to revascularization of the transferred STEMI patients.
INTRODUCTION
Acute myocardial infarction is one of the most common causes of death in adults globally, and accounts for approximately 5% of all deaths in South Korea [1,2]. Revascularization of coronary arteries is important to increase the survival rate of patients with myocardial infarction. Especially, in patients with ST elevation myocardial infarction (STEMI), the shorter the time to reperfusion, the higher is the patient’s survival [3]. The American College of Cardiology and the American Heart Association (AHA) guidelines recommend rapid percutaneous coronary intervention (PCI) of all STEMI patients. In PCI-capable hospitals, the recommended door-to-balloon time is less than 90 minutes, and in a non-PCI-capable hospital, the recommended time for the first door-to-balloon (D1-to-B) time starting from the visit at the initial referral hospital to reperfusion is less than 120 minutes [4].
The expansion of PCI facilities by the Korean government and related institutions has decreased the time required for coronary reperfusion therapy [5-9].
As a result, 95.7% of STEMI patients admitted to regional cardiovascular centers during 2011 achieved PCI within 90 minutes [10]. However, more than half of STEMI patients are referred to PCI after visiting the emergency department of a non-PCI capable hospital first [11]. According to Kim et al. [12] and Park et al. [13], 60.9% of STEMI patients visit non-PCI capable hospitals initially and are subsequently transferred to hospitals with a PCI facility, and the D1-to-B time of 120 minutes was observed only in 29.3% of such STEMI cases.
Due to growing awareness of the need to reduce the D1-to-B time of the referred STEMI patients significantly, efforts to further shorten the revascularization time of acute myocardial infarction patients are ongoing. The delay in D1-to-B time in South Korea is primarily attributed to geographical factors and the procedures for acceptance and admission to PCI-capable hospitals [14,15]. To the best of the authors’ knowledge, no domestic localization strategies or effects have been reported to overcome these limitations. Therefore, the authors designed a strategy known as Preparing Revascularization Effort before Patients’ Arrival via Regionalization Engagement (PREPARE) to reduce the reperfusion time for the transfer of STEMI patients from non-PCI capable hospitals. This study is a pilot trial to reveal the effectiveness of reducing the D1-to-B time and outcomes via PREPARE protocols.
METHODS
Study design and hospital setting
This single center retrospective observational study was conducted with STEMI patients who were referred for PCI between March 2011 and February 2016. Patients were excluded if they had two or more interhospital transfers or were transferred more than 15 km away from the hospital or used a private vehicle for transport or refused PCI.
The authors’ hospital is a tertiary university hospital located in Goyang, northwest of Gyeonggi province, and the PCI facility was always available to the team. Five hospitals equipped with PCI facilities were located within a 15-km radius of the hospital. Such hospitals are responsible for the treatment of cardiovascular emergencies in nearly 2-million civilians of Goyang, Paju, and Gimpo. Due to the absence of PCI-capable hospitals in Paju and their location in the northern region of South Korea, most STEMI patients are transferred to the authors’ hospital. The authors implemented a PREPARE strategy to reduce the transfer time of STEMI patients in conjunction with an emergency medical center located in Paju, which was located at a distance of 10 km from the authors’ hospital. We have not informed other institutions about the PREPARE strategy and therefore, they did not use the strategy during the study period.
Regionalization protocol: PREPARE
The authors’ protocols for localization strategies in hospitals were as follows based on steps 3, 4, and 7 conforming to Bradley’s six guidelines to reduce PCI time [16].
First, the referral hospital emergency physician (EP1) confirms the results of a 12-lead electrocardiogram within 10 minutes of patient arrival. Second, if STEMI is suspected, the EP1 immediately contacts the emergency physician (EP2) in the authors’ hospital via a hot line. Third, EP1 sends electrocardiogram images to EP2 via mobile phone short message service pending transfer request. Fourth, acceptance of STEMI patients is determined by EP2 immediately. Fifth, after acceptance of transfer, EP2 shares the electrocardiogram received with the cardiologist and determines the PCI team activation. Sixth, PCI teams are fully activated following a single contact from the emergency department. Seventh, EP1, EP2, and cardiologist exchange feedback based on the treatment results available online within 48 hours.
Study variables
Clinical data obtained from electronic medical records included the following parameters: age, sex, hypertension, dyslipidemia, current smoking, familial history, previous myocardial infarction, previous stroke, height, weight, initial heart rate, initial systolic blood pressure, Killip class, time segment of door-to-balloon, and outcomes.
The time segment from the first hospital visit to the reperfusion treatment was defined as follows: Length of stay in the referring hospital (D1LOS) means patient’s stay in the first hospital. Interhospital transport (D1-to-D2) time is the time required for transport between hospitals. Door-to-balloon (D2-to-B) time indicates the time taken from arrival at the referred hospital until reperfusion. D1-to-B time means the time taken from arrival at the first referral hospital until reperfusion.
We defined on-duty time as the hours from 8 a.m. to 6 p.m. on weekdays when PCI team were on standby at the hospital. Otherwise night and holiday when PCI teams were activated within 30 minutes on-call were defined as on-call time. We defined adequate D1-to-B time if the D1-to-B time was within 120 minutes per AHA guidelines [4]. The primary outcome of our analysis was adequate D1-to-B time. The secondary outcome was length of hospital stay, intensive care unit length of stay, and incidence of major adverse cardiac events within 4 weeks, such as cardiac arrest, recurrent myocardial infarction, or death.
The patients were divided into two groups. The PREPARE group included patients who were transferred via PREPARE protocol and the non-PREPARE group included patients who were transferred via conventional methods.
Statistical analysis
We compared the study variables of the PREPARE and the non-PREPARE groups. Continuous variables were presented as median values (interquartile range) and compared by Mann-Whitney test. Nominal data were calculated as percentages based on the frequency of occurrence and compared using chi-square or Fisher exact test, as appropriate. Multivariate logistic regression was used to correlate single variables with adequate D1-to-B time. The resulting odds ratios (ORs) were presented with 95% confidence intervals (CIs). A two-sided P-value less than 0.05 was considered statistically significant. Analysis was performed using IBM SPSS Statistic ver. 24.0 (IBM Corp., Armonk, NY, USA).
Ethics statement
This study was approved by the institutional review board of Dongguk University Ilsan Hospital, Dongguk University (DUIH2017-11-007). Informed consent was waived by the board.
RESULTS
Patient demographics
During the study period, 107 STEMI patients were transferred to our institution for PCI from other non-capable PCI hospitals. Among them, six patients were excluded due to interhospital transport across distances greater than 15 km, two patients were excluded due to two or more interhospital transfers, two patients were excluded due to the use of private vehicles and not an ambulance for transport, and one patient was excluded because they declined PCI. Finally, 96 patients were enrolled in the study (Fig. 1). Fifty (52.1%) and 46 (47.9%) patients were enrolled in PREPARE and non-PREPARE groups, respectively. The PREPARE group was younger (58 years [49–71] vs. 73 years [56–80], P=0.029), comprised a higher percentage of male patients (80% vs. 56.5%, 0.016), and were taller (166.0 cm [161.0–171.0] vs. 163.0 cm [153.0–169.0], P=0.032) than those in the non-PREPARE group. There were no other significant differences in general characteristics between the two groups (Table 1).

Flow chart of the patient enrollment. STEMI, ST elevation myocardial infarction; PCI, percutaneous coronary intervention; PREPARE, Preparing Revascularization Effort before Patients’ Arrival via Regionalization Engagement.
Time segment required for coronary reperfusion
In the time segment required for revasculization, the D1LOS (20.0 [12.0–30.0] vs. 36.0 [23.0–52.0], P=0.001) and D1-to-B (111.0 [97.0–130.0] vs. 134.0 [115.0–182.0], P<0.001), were shorter in the PREPARE group than in the non-PREPARE groups. Adequate D1-to-B time (60.0% vs. 30.4%, P=0.004) was higher in the PREPARE group than in the non-PREPARE group (Table 2).
Multivariate logistic regression analysis revealed that on-call time (OR, 0.287; 95% CI, 0.102–0.805; P=0.018) was negatively correlated with adequate D1-to-B time, and transfer via PREPARE protocol (OR, 3.399; 95% CI, 1.150–10.050; P=0.027) was related to adequate D1-to-B time (Table 3).
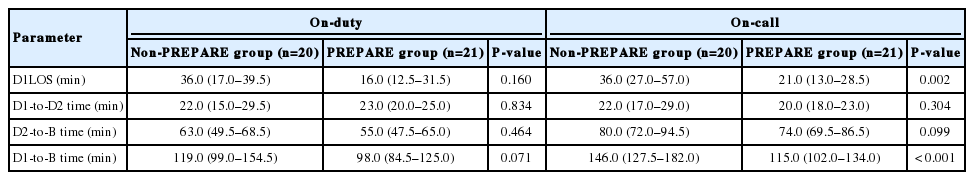
Comparison of time segment between on-duty time and on-call time
Compared with on-call time, D1LOS (21.0 [13.0–28.5] vs. 36.0 [27.0–57.0], P=0.002) and D1-to-B times (115.0 [102.0–134.0] vs. 146.0 [127.5–182.0], P<0.001) were shorter in the PREPARE group than in the non-PREPARE group. No significant difference was detected in the time to revascularization between the two groups with on-duty time (Table 4).
DISCUSSION
In STEMI patients, the hospital mortality rate was 3.0% following reperfusion within 90 minutes of hospital visit; However, the mortality rate increased to 4.2% and 7.4% whenever the revascularization time was delayed from 91 to 150 minutes and 150 minutes, respectively [17]. Another study found that every 30 minutes of PCI delay from the onset of the symptoms increased the risk of one-year mortality by 7.5% [18]. On the basis of these reports, many health organizations and societies have recommended rapid reperfusion therapy for STEMI patients, which have greatly affected the ability of hospitals to meet the rapid reperfusion treatment requirement [19-21].
According to the current treatment data available for STEMI patients in South Korea, the D2-to-B times less than 90 minutes at the regional PCI center were 85.9% in 2008, and 95.7% in 2011 [10]. Similarly, a remarkable shortening in time to reperfusion therapy in STEMI was observed in patients in South Korea over the years.
In the case of a transferred STEMI patient, however, the results have not been not satisfactory. According to Korea Acute Myocardial Infarction Registry (KAMIR) statistics, 60.9% of STEMI patients first visit hospitals where PCI is not available [12]. A similar trend has been detected internationally, and in general, about half of STEMI patients visit hospitals initially where PCI is not available [22,23].
The AHA recommends a D1-to-B time of less than 120 minutes from the initial visit to a non-PCI facility to a PCI after transfer.4 Vora et al. [24] analyzed the Acute Coronary Treatment and Intervention Outcomes Network Registry-Get With the Guidelines database containing 22,481 registered cases obtained from 1,771 STEMI reference centers between 2008 and 2012, and reported that the D1-to-B time within 120 minutes of the transfer in patients who had primary PCI was 42.6%.
Unfortunately, according to Park et al. [13], the D1-to-B time within 120 minutes was only 29.3% among locally transferred STEMI patients between 2007 and 2012 in South Korea. Sim et al. [25] analyzed the 2005-2011 KAMIR data and reported that the median D2-to-B time of the transferred STEMI patients in South Korea was 78 minutes at STEMI-receiving hospitals, whereas the D1-to-B time within 120 minutes was only 26.1%.
Similar distributions were identified in this study; the D1-to-B time within 120 minutes was only achieved by 30.4% in the non-PREPARE group, which was not exposed to the regionalization strategy. In a report analyzing KAMIR data of 8,040 domestic patients undergoing primary PCI from 2008 to 2011, Kim et al. argued that in order to reduce the total ischemic time, in addition to shortening the D2-to-B time at the hospital providing the treatment, new strategies are needed at the pre-hospital stage [26].
In South Korea, the effects of the localization strategy to shorten the D1-to-B time have yet to be reported. We have shown that the time to revascularization of the transferred STEMI patients was reduced using the PREPARE protocol, which significantly demonstrates the effectiveness of the localization strategy domestically, for the first time. In this study, the D1-to-B time of the transferred STEMI patients using the PREPARE protocol within 120 minutes was 60.0%, which was significantly different from the 30.4% in the non-PREPARE group. Miedema et al. [27] analyzed the factors underlying the extended D1-to-B time in the transferred patients: based on the length of stay in the referring hospital, interhospital transport time and door-to-balloon time in the referred hospital, the findings suggest that the longest and the most significant delay involved D1LOS. Usually in South Korea, in order to accept transfer of patients with STEMI, the cardiologist of the referred hospital might be contacted for confirmation, which causes delays at several stages. In particular, if a PCI-capable hospital is not available nearby, it is a time-consuming process to inquire about the transfer to multiple hospitals. In this study, emergency physicians accepted the requested patient transfer independent of cardiologist consultation in the PREPARE group. In addition, even if the initial diagnosis was ambiguous, the treatment method was decided after accepting the transfer first and sharing the electrocardiogram via short message service with the cardiologist during patient transportation. This process ensured that the transfer was not unduly delayed at the referral hospital, and significantly shortened the length of stay by obviating the need to request several hospitals for acceptance.
In this study, the D2-to-B time with on-call activation was 80 minutes for the non-PREPARE groups and 74 minutes for the PREPARE group, similar to the average time of 76 minutes required for PCI at the STEMI-receiving hospital in South Korea [6].
Wilson et al. [28] reported a 60% to 90% improvement in performance within 120 minutes of D1-to-B time following a regionalization strategy at the hospitals within a radius of 80 km of the Carolina Medical Center. In their study, the D2-to-B time target in the referred hospital was 30 minutes and the performance was increased from 72.3% to 93.4% after the protocol was applied. Holmes et al. [29] also reported that the D1-to-B time decreased from 85 to 65 minutes during on-duty time and from 98 to 74 minutes during on-call time following the regionalization protocol, when D2-to-B time was 37 minutes during on-duty time and 29 minutes during on-call time. By contrast, the average D2-to-B time was 76 minutes in the STEMI-receiving hospital in South Korea [6]. The most important factor contributing delays in D2-to-B time in South Korea is related to difficulties having PCI teams on duty 24 hours a day [30]. At nights or during holidays, most of the PCI facilities activated the PCI team on-call after patients were admitted even if the transferred STEMI patients visited the hospital. Although no significant reduction was seen in our study, the D2-to-B time, especially during on-call times, was reduced if the PCI team was pre-activated during patient transfer via the PREPARE protocol. A further study is needed to corroborate the results of the PREPARE strategy reported in this study.
This study has a few limitations. First, this study was conducted at a single institution. Therefore, the results may not represent the comprehensive characteristics of domestically transferred STEMI patients. Second, since the transfer and treatment of patients in the PREPARE group was previously requested, the Hawthorne effect may have been caused by the members of the referral hospital medical members. Third, since patients requested by a single pre-consulted hospital were included in the PREPARE group, the authors’ medical staff at the hospital emergency room distinguished patients belonging to the PREPARE and non-PREPARE groups, possibly resulting in a selection bias. Fourth, the study was limited to patients’ prognosis under the PREPARE protocol because the number of patients was not large enough to verify serious outcomes such as mortality. Finally, the study used only the time of the first hospital visit by patients as a variable because it was not easy to confirm pre-hospital factors such as onset of chest pain or the ambulance arrival time.
Application of the PREPARE protocol reduced the time required for reperfusion of STEMI patients transferred between the hospitals. Whether the standby PCI team at the hospital or on call is a factor determining adequate D1-to-B time needs further analysis.
Notes
No potential conflict of interest relevant to this article was reported.
References
Article information Continued
Notes
Capsule Summary
What is already known
Remarkable shortening in intra-hospital time to reperfusion therapy in ST elevation myocardial infarction (STEMI) was observed in patients in South Korea over the years. However, more than half of STEMI patients are referred from outside hospitals because they visited non-percutaneous coronary intervention (non-PCI) capable facility first.
What is new in the current study
An inter-hospital transfer strategy (PREPARE, Preparing Revascularization Effort before Patients’ Arrival via Regionalization Engagement) reduced the time required for reperfusion of STEMI patients transferred from non-PCI capable hospitals. It would be useful to reduce the reperfusion time in this way in facilities where the PCI team cannot be operated 24 hours a day.