Association between the number of prehospital defibrillation attempts and neurologic outcomes in out-of-hospital cardiac arrest patients without on-scene return of spontaneous circulation
Article information
Abstract
Objective
Delivery of prehospital defibrillation for shockable rhythms by emergency medical service providers is crucial for successful resuscitation in out-of-hospital cardiac arrest (OHCA) patients. The optimal range of prehospital defibrillation attempts for refractory shockable rhythms is unknown. This study evaluated the association between the number of prehospital defibrillation attempts and neurologic outcomes in OHCA patients.
Methods
A retrospective observational study was conducted using the nationwide OHCA registry. Adult OHCA patients who were treated by emergency medical service providers due to presumed cardiac origin with initial shockable rhythm were enrolled from 2013 to 2016. The final analysis was performed on patients without on-scene return of spontaneous circulation. The number of prehospital defibrillation attempts was categorized as follows: 2–3, 4–5, and ≥6 attempts. The primary outcome was a good neurologic recovery at hospital discharge. Multivariate logistic regression analysis was performed to evaluate the association between neurologic outcomes and the number of prehospital defibrillation attempts.
Results
A total of 4,513 patients were included in the final analysis. The numbers of patients for whom 2–3, 4–5, and ≥6 defibrillation attempts were made were 2,720 (60.3%), 1,090 (24.2%), and 703 (15.5%), respectively. Poorer outcomes were associated with ≥6 defibrillation attempts: survival to hospital discharge (adjusted odds ratio, 0.38; 95% confidence interval, 0.21–0.65) and good neurologic recovery (adjusted odds ratio, 0.42; 95% confidence interval, 0.21–0.84).
Conclusion
Six or more prehospital defibrillation attempts were associated with poorer neurologic outcomes in OHCA patients with an initial shockable rhythm who were unresponsive to on-scene defibrillation and resuscitation.
INTRODUCTION
High quality on-scene resuscitation by emergency medical service (EMS) providers is a key factor in improving the outcome of out-of-hospital cardiac arrest (OHCA) patients [1,2]. Prompt defibrillation is important for better survival and neurologic outcomes, especially in patients with an initial shockable rhythm (ventricular fibrillation [VF]/pulseless ventricular tachycardia [pVT]). Various EMS strategies have attempted to improve the provision of defibrillation in the prehospital setting [3-5]. However, not all patients with an initial shockable rhythm respond to defibrillation, even after several attempts.
Previous studies of refractory VF/pVT have shown that the success rate of defibrillation is generally poor and 30-day survival rates decrease as the number of defibrillation attempts increases [6,7]. In the case of refractory VF/pVT, the secondary rescue therapy, such as administration of amiodarone and application of extracorporeal cardiopulmonary resuscitation (E-CPR), should be considered [8-10]. In many communities, especially in Asia, E-CPR and some intravenous antiarrhythmic medications are not usually provided in the prehospital setting [11-13]. Therefore, if patients do not achieve a return of spontaneous circulation (ROSC) after a certain number of defibrillation attempts in the field, EMS providers must transport patients with ongoing cardiopulmonary resuscitation (CPR) in the ambulance. Determining the optimal range of defibrillation attempts before hospital transport is difficult. More defibrillation attempts on-scene may delay the secondary rescue therapy that can only be administered in the hospital. However, fewer defibrillation attempts before hospital transport risk bypassing the narrow time window in which defibrillation is highly effective because rhythm analysis and defibrillation delivery are difficult in the moving ambulance during transport to the hospital [14-16].
Most EMS and CPR practice guidelines emphasize the importance of prompt rhythm analysis and on-scene delivery of defibrillation by EMS providers. However, there are no clear guidelines regarding the optimal range of prehospital defibrillation attempts. In this study, we evaluated the association between the number of prehospital defibrillation attempts and neurologic outcomes in OHCA patients with an initial shockable rhythm. We hypothesized that an optimal range of prehospital defibrillation attempts would be associated with good neurologic recovery in OHCA patients.
METHODS
Study design
A retrospective observational study was conducted using the nationwide OHCA registry. In South Korea, a public, fire-based EMS system responds to all ambulance calls. It provides a basic to intermediate level of ambulance services, including the use of manual or automated external defibrillators and advanced airway management (e.g., endotracheal intubation and supraglottic airway insertion), under the medical direction of EMS. EMS providers are trained to check pulse and analyze rhythms using manual or automated external defibrillators after 2-minute intervals of CPR. Once defibrillation for shockable rhythms has been performed, EMS providers are trained to immediately resume chest compressions without additional pulse checks or rhythm analysis. The on-scene administration of intravenous medications by EMS providers, such as epinephrine and amiodarone, is not permitted, except in extraordinary circumstances and under direct medical supervision. The EMS protocol encourages ≥5 minutes of resuscitation before transport to the hospital. There are no recommendations regarding the maximum length of resuscitation time or the maximum number of on-scene defibrillation attempts when ROSC is not achieved.
The nationwide OHCA registry has been operational since 2006. It is based on a collaboration between the Korea Centers for Disease Control and Prevention and the Korean National Fire Department. The database consists of prehospital EMS records and hospital medical records. EMS run sheets were completed by on-scene prehospital EMS providers and stored in the Fire Department’s central server. Prehospital EMS variables (ambulance call, dispatch, and arrival times; departure to hospitals; location of OHCA; medical procedures performed by emergency medical teams; and destination hospitals) and details of the EMS run sheets were reviewed by the EMS medical director responsible for each local EMS agency. Data from hospital medical records, including Utstein variables for reporting OHCA and clinical outcomes, were reviewed and extracted by certified medical reviewers from the Korea Centers for Disease Control and Prevention. Details of the data collection and handling processes of the nationwide OHCA registry have been reported previously [13,17,18].
This study was approved by the relevant institutional review board (1103-153-357), which waived the requirement for informed consent.
Study setting and population
OHCA patients of presumed cardiac origin who were treated by adult EMS providers (≥18 years of age) between January 2013 and December 2016 were initially enrolled. For the final analysis, we selected patients with an initial shockable rhythm (VF/pVT), without on-scene ROSC, who were defibrillated by EMS providers at least twice. Patients with OHCA witnessed by EMS providers and patients defibrillated by bystanders before the arrival of EMS providers were excluded. Patients with missing data regarding the number of prehospital defibrillation attempts, on-scene ROSC status, and hospital outcomes were also excluded.
Study protocol
The main exposure variable was the number of prehospital defibrillation attempts by EMS providers on-scene, categorized into three groups as follows: 2–3, 4–5, and ≥6 attempts. The following prehospital EMS and hospital variables were also included in the analysis: patient age, sex, location of OHCA (private or public), bystander CPR, bystander witness status, EMS advanced airway management, EMS response time interval, EMS scene time interval, emergency department level, and provision of post resuscitation care (targeted temperature management and cardiac reperfusion therapy). Metropolitan variables included enacted metropolitan cities (Seoul, Sejong, Incheon, Ulsan, Daegu, Daejeon, Busan, and Gwangju) vs. the remaining areas of South Korea.
Key outcome measures
The primary outcome was a good neurologic recovery at hospital discharge, defined as a cerebral performance category of (1) good performance (might have mild neurologic or psychologic deficits; able to work) or (2) moderate disability (sufficient cerebral function for independent activities of daily life; able to work in a sheltered environment). The other cerebral performance categories are (3) severe disability (dependent on others for daily support because of impaired brain function, ranging from ambulatory to severe dementia/paralysis), (4) coma or vegetative state, and (5) brain death [19]. The secondary outcome was survival to hospital discharge.
Data analysis
Multivariate logistic regression analysis was performed to evaluate the association between neurologic outcomes and the number of prehospital defibrillation attempts. Adjustments were made for potential confounders, including age, sex, underlying medical conditions (hypertension and cardiovascular disease), location of OHCA, bystander CPR, bystander witness status, EMS response time interval, EMS advanced airway management, and EMS intravenous line insertion.
To examine differences in the effect of the number of prehospital defibrillation attempts according to the level of urbanization, interaction analysis was performed using the final multivariate logistic regression model. In South Korea, the population density is concentrated in large cities, and there are significant differences in EMS protocols between regions. We hypothesized that there would be interregional differences in hospital arrival times for OHCA patients. Therefore, we conducted an interaction analysis between metropolitan and rural areas.
Adjusted odds ratios (aORs) and 95% confidence intervals (CIs) were estimated for survival to hospital discharge and good neurologic recovery. Statistical analyses were performed using the SAS ver. 9.4 (SAS Institute Inc., Cary, NC, USA) and Stata ver. 13.1 (Stata Corp., College Station, TX, USA).
RESULTS
A total of 10,762 adult EMS-treated OHCA patients of presumed cardiac origin with an initial shockable electrocardiographic rhythm, who were defibrillated at least twice, were initially enrolled in this study. Patients who met the following criteria: (1) OHCA witnessed by EMS providers during transport (n=557), (2) defibrillated by bystanders (n=226), (3) defibrillated only once (n=3,558), (4) unknown number of defibrillation attempts (n=166), and (5) missing outcome data (n=2) were serially excluded. Of the remaining 6,253 patients, 4,513 (72.2%) left the scene without ROSC after ≥2 defibrillation attempts for shockable cardiac rhythms (Fig. 1). Patient distribution and survival outcomes are shown in Fig. 2 according to the number of prehospital defibrillation attempts by EMS providers.
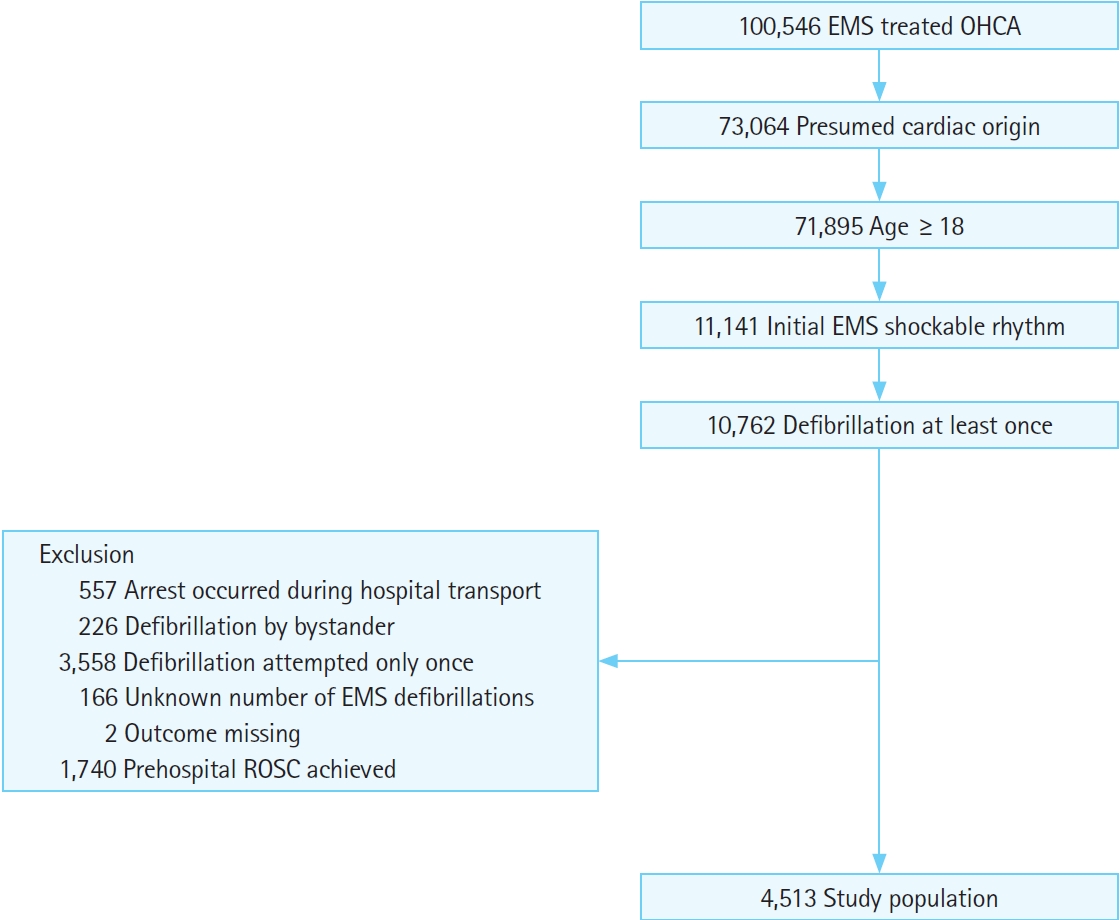
Patient enrollment flowchart. EMS, emergency medical service; OHCA, out-of-hospital cardiac arrest; ROSC, return of spontaneous circulation.
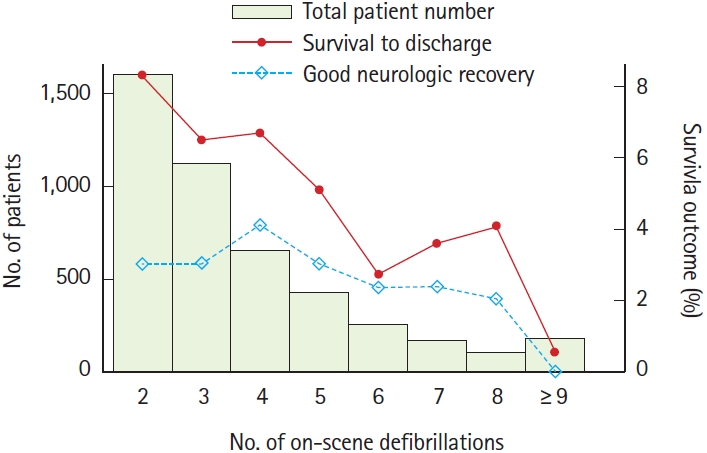
Patient distribution and survival outcomes according to the number of prehospital defibrillation attempts by emergency medical service personnel in the study population.
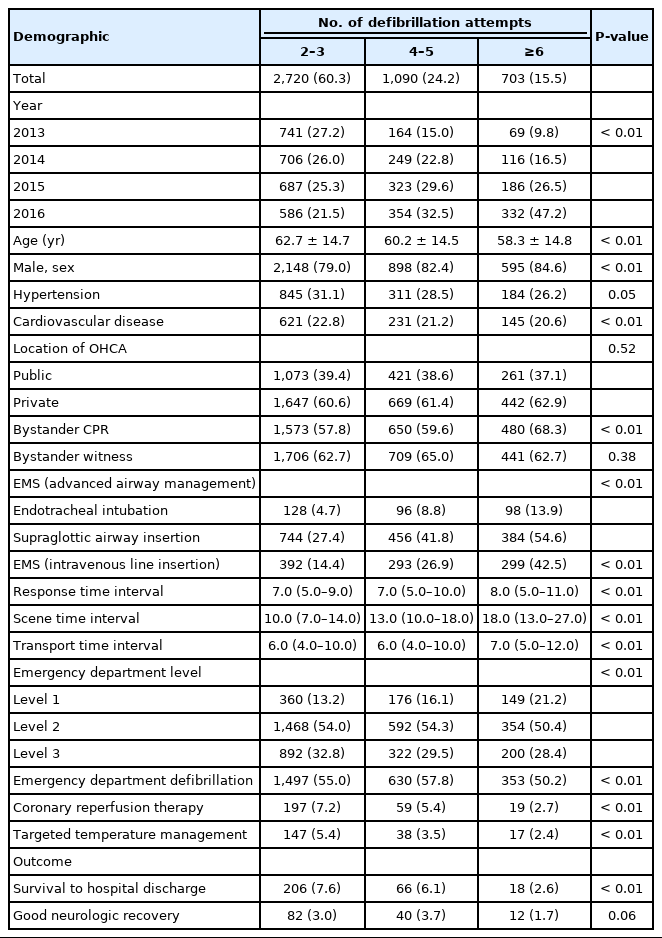
The demographics of the study population according to the number of defibrillation attempts are shown in Table 1. Although good neurologic recovery was most frequently achieved in the group with 4–5 defibrillation attempts, the difference was not significant (2–3, 4–5, and ≥6 defibrillation attempts: 3.0%, 3.7%, and 1.7%, respectively; P=0.06).
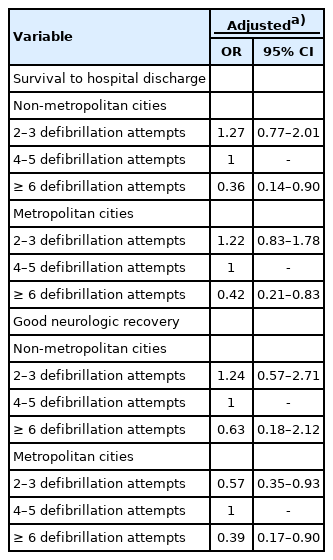
The results of the univariate and multivariate logistic regression analyses are shown in Table 2. Prehospital defibrillation attempts of ≥6 were associated with poorer outcomes, both in terms of survival to hospital discharge (aOR, 0.38; 95% CI, 0.21–0.65) and good neurologic recovery (aOR, 0.42; 95% CI, 0.21–0.84).
In the interaction analysis, 2–3 defibrillation attempts (aOR, 0.57; 95% CI, 0.35–0.93) and ≥6 defibrillation attempts (aOR, 0.39; 95% CI, 0.17–0.90) were associated with significantly poorer neurologic outcomes than 4–5 defibrillation attempts in metropolitan cities (Table 3). In both metropolitan and non-metropolitan cities, survival to hospital discharge decreased as the number of prehospital defibrillation attempts increased. In non-metropolitan cities, there were no significant associations between neurologic outcomes and the number of prehospital defibrillation attempts.
DISCUSSION
We analyzed clinical outcomes according to the number of prehospital defibrillation attempts in OHCA patients with refractory shockable rhythms without on-scene ROSC. The associations between clinical outcomes and the number of prehospital defibrillation attempts were insignificant for 2–3 and 4–5 defibrillation attempts. However, ≥6 defibrillation attempts were associated with poorer survival to hospital discharge and poorer neurologic outcomes. In the interaction analysis, an intermediate number of defibrillation attempts (i.e., 4–5) was associated with better neurologic outcomes.
Our findings suggest that an excessive number of defibrillation attempts is not beneficial and may actually be harmful to patients without ROSC following serial defibrillation attempts on-scene. We believe that because of the uniqueness of our EMS system, in which intravenous medications, such as epinephrine and amiodarone, cannot be administered in the prehospital setting, delayed time to advanced cardiac life support may be one of the reasons for these findings.
In this study, patients who achieved prehospital ROSC were excluded. Patients receiving more defibrillation shocks in the field who achieved ROSC as a result of subsequent defibrillation attempts were also excluded from the final analysis. We initially expected that the outcomes of the group with 2–3 defibrillation attempts might be superior to the groups with a greater number of defibrillation attempts. However, there was no significant difference in the aOR between 2–3 and 4–5 defibrillation attempts in the total population. In the interaction analysis, 4–5 defibrillation attempts were associated with a better neurologic outcome than 2–3 defibrillation attempts in metropolitan cities. There may be several possible explanations for this. One explanation is that the number of defibrillation attempts may act as a surrogate marker of sufficient on-scene resuscitation before hospital transport. During hospital transport, high-quality CPR and rhythm analysis are difficult to perform in a moving stretcher and ambulance, even for trained EMS providers [14-16]. Therefore, sufficient time and effort should be given to on-scene evaluation and resuscitation before transport to the hospital. We also analyzed the association between the number of prehospital defibrillation attempts (as a continuous variable) and survival by including cubic spline. However, stratifying the number of prehospital defibrillation attempts into groups proved to be more desirable for both EMS providers and emergency room physicians.
In addition to antiarrhythmic drugs, there are other forms of management for refractory cardiac arrest that can only be provided in the hospital. One of these is the initiation of cardiopulmonary bypass during resuscitation, known as E-CPR. This involves urgent cannulation of large vessels and initiation of venoarterial extracorporeal circulation and oxygenation with an extracorporeal membrane oxygenator. Several observational studies have suggested that in conventional CPR, extracorporeal membrane oxygenation is associated with favorable outcomes in cardiac arrest patients <75 years of age. The International Liaison Committee on Resuscitation Advanced Life Support Task Force conducted a systemic review in 2015 [20]. A prospective propensity-matched observational study reported that there was a greater tendency for ROSC, as well as improved survival to hospital discharge, 30-day follow-up, and 1-year follow-up (except for neurologic outcomes), in the E-CPR group than in the conventional CPR group [21]. A retrospective observational study showed that E-CPR was associated with survival and neurologic benefits at hospital discharge and 6-month follow-up [22]. However, a retrospective propensitymatched observational study suggested that E-CPR was not associated with survival or neurologic benefits at hospital discharge, 30-day follow-up, or 1-year follow-up [23]. A prospective observational cohort study and post hoc propensity-matched analysis showed that E-CPR was associated with better neurologic outcomes at 3-month follow-up [24]. Another prospective observational study reported improved neurologic outcomes in E-CPR patients at 1- and 6-month follow-up [25]. In conclusion, there is insufficient evidence to recommend the routine use of extracorporeal membrane oxygenation, which may be considered for patients with refractory cardiac arrest with shockable rhythms, in selected inclusion criteria.
Another management strategy to support patients with refractory cardiac arrest is the administration of intravenous medications, such as epinephrine and amiodarone. Vasopressors, such as epinephrine, improve blood pressure and flow to the coronary and cerebral circulation to enhance perfusion, while antiarrhythmic drugs, such as amiodarone, facilitate the restoration and maintenance of a spontaneous perfusion rhythm in combination with the termination of VF. Several large observational studies have reported that the early use of epinephrine is associated with improved outcomes in OHCA patients [9,26]. Several randomized controlled trials have also shown that patients who were administered epinephrine exhibited a higher rate of ROSC and better 30-day survival than those who were administered placebo, consistent with findings from previous observational studies and a randomized controlled trial [27]. Different observations have been reported regarding the use of epinephrine in patients with different electrocardiographic rhythms. Epinephrine improved the 30-day survival rate of patients with non-shockable rhythms, but no clear benefits were observed in patients with shockable rhythms [28,29]. In patients with refractory shockable rhythms, antiarrhythmic drugs can help achieve successful defibrillation and reduce the risk of recurrent VF/pVT. In blinded randomized controlled trials of adult OHCA patients with refractory VF/pVT, paramedic-administered amiodarone in polysorbate (300 mg or 5 mg/kg) improved survival to hospital admission [29,30]. However, it did not affect survival to hospital discharge or neurologic outcomes. Therefore, the effectiveness of intravenous medications for patients with refractory cardiac arrest with shockable rhythms may need to be considered.
If all of the advanced cardiac and extracorporeal life support that can only be provided in the hospital could be provided on-scene, then discussion regarding the optimal range of prehospital defibrillation attempts would be meaningless. However, in all EMS systems, hospital transport should be considered for patients with refractory shockable rhythms, even if the patient does not achieve ROSC. To our knowledge, there are no universal resuscitation guidelines or consensus regarding the number of prehospital defibrillations that should be attempted in patients with refractory arrhythmia before leaving the scene. We believe that the results of this study may be beneficial to EMS directors and providers who must make decisions every day between more defibrillation attempts in the field and hospital transport for OHCA patients with refractory shockable rhythms without on-scene ROSC.
There are several limitations of this study. First, the type of initial EMS electrocardiographic rhythm in the nationwide OHCA registry was recorded by emergency medical technicians. There is potential for these electrocardiographic diagnoses to be less accurate than those of medical doctors. In our medical oversight system, EMS medical directors reviewed all OHCA registries with scanned copies of electrocardiographic rhythm strips attached that were completed by EMS providers. Although the rate of electrocardiographic misdiagnosis has not been previously reported, the rate of confusion between shockable and non-shockable rhythms is usually very low. Second, in our nationwide OHCA registry, we did not collect the final on-scene electrocardiographic results before hospital transport. Although the enrolled patients did not achieve on-scene ROSC, it is unclear whether patients still had shockable rhythms at the commencement of hospital transport. Third, our study did not include an analysis of defibrillation times in the prehospital setting or the number of defibrillation attempts and defibrillation times after visiting the emergency room. Finally, with the exception of hospital factors, it is factors affecting ROSC in OHCA patients that are very diverse: patient age, past medical history, bystander-administered CPR and use of automated external defibrillators, EMS response time interval, EMS advanced airway management (whether successful or not), and so forth. More detailed analysis adjusting for these potential confounding variables is needed.
In summary, ≥6 prehospital defibrillation attempts were associated with poorer neurologic outcomes in OHCA patients with an initial shockable rhythm who did not achieve on-scene ROSC after defibrillation by EMS providers. In metropolitan cities, 4–5 prehospital defibrillation attempts were associated with a better neurologic outcome. Future prospective studies are needed to determine the optimal range of prehospital defibrillation attempts for maximizing the neurologic outcomes of OHCA patients with refractory shockable rhythms.
Notes
No potential conflict of interest relevant to this article was reported.
Acknowledgements
This study was supported by the Korea Centers for Disease Control and Prevention (E33010-00).
References
Article information Continued
Notes
Capsule Summary
What is already known
Early and timely defibrillation is important for out-of-hospital cardiac arrest with shockable rhythm.
What is new in the current study
An optimal range of defibrillation attempts might be associated with favorable neurologic outcome.