Predictive values of the Pediatric Penetrating Ocular Trauma Score and the Toddler/Infant Ocular Trauma Score in Brazilian children with open globe injury
Article information
Abstract
Objective
This study compared the prognostic value of the Pediatric Penetrating Ocular Trauma Score (POTS) with the Toddler/Infant Ocular Trauma Score (TOTS) in a cohort of Brazilian children with open-globe injuries.
Methods
This retrospective, observational case series included consecutive children with open-globe injuries seen at the Santa Casa de Sao Paulo Eye Emergency Service. The medical records of all patients were reviewed for data analysis, including the circumstance and time of injury, type of penetrating injury, initial and final visual acuity (VA), time of surgery, and associated eye diseases. The test characteristics of POTS and TOTS for VA were calculated and compared by the McNemar test.
Results
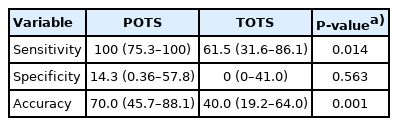
Thirty patients were included. The mean age was 3.9 ± 1.6 years; 20 were male patients and 10 were female patients. Most wounds were limited to the anterior segment (93.3%). The sensitivity for the POTS was higher than that of the TOTS (100%; 95% confidence interval [CI], 75.3–100 vs. 61.5%; 95% CI, 31.6–86.1; P = 0.014). The specificity was not significantly different (14.3%; 95% CI, 0.4–57.8 vs. 0%; 95% CI, 0–41.0; P = 0.563). The accuracy for the POTS was higher than the TOTS (70.0%; 95% CI, 45.7–88.1 vs. 40.0%; 95% CI, 19.1–63.9; P = 0.001).
Conclusion
In this cohort of Brazilian children with open-globe injuries, the POTS had better accuracy than did the TOTS in predicting VA after treatment.
INTRODUCTION
Ocular trauma in children can cause life-long visual disability and poses a burden to the healthcare system and society [1]. Most pediatric cases of open globe injury—the most devastating type of eye trauma—occur at home and are the result of sharp object penetration [2]. Proper care of these children requires careful evaluation and timely treatment in order to optimize outcomes. A major challenge in the care of eye trauma in children is a precise visual prognostication. Parents often ask physicians if their child is going blind or if it is going to be able to see again. This is an issue of major concern and, in order to help healthcare providers to predict appropriate final visual outcomes, different ocular trauma scoring systems have been developed. The Ocular Trauma Score was the first generic instrument; the predicted visual acuity (VA) is estimated by subtracting raw points for five diagnostic findings from the initial VA [3]. However, its use in children proved to be less precise, probably due to the inability to obtain an accurate VA, and prompted authors to develop instruments specifically for pediatric patients [4-8]. The Pediatric Penetrating Ocular Trauma Score (POTS) downplayed the initial VA, added age and wound location as two new variables, and removed the afferent pupillary defect as a prognostic factor. 8 The POTS proved to be a viable tool for predicting visual outcomes of pediatric ocular trauma with traumatic cataracts [9]. Nevertheless, the POTS has received criticism [10-14].
More recently, the Toddler/Infant Ocular Trauma Score (TOTS) was developed specifically for children under 6 years of age with traumatic open globe injuries. Similar to the POTS, it is not reliant on the presenting VA and has proven to be useful in predicting prognosis in very young children in the United States [15]. The TOTS has not been evaluated in children living in a developing country where socioeconomic and healthcare conditions differ from those in industrialized countries. Therefore, this study aimed to evaluate the clinical features of traumatic open globe injuries in a cohort of young Brazilian pediatric patients and to compare the prognostic accuracy between the TOTS and POTS.
METHODS
Ethics statement
This retorspective study was conducted with the approval of the Human Subjects Research Committee at Irmandade da Santa Casa de Misericórdia de Sao Paulo (No. 082/11). All procedures followed the tenets of the Declaration of Helsinki, its late amendments, and Resolution 466/2012 (National Heath Council, Ministry of Health, Brazil). Informed consent was exempted due to the type of research.
Sample and data acquisition
All patients younger than 6 years of age who presented at the Santa Casa de Sao Paulo Ophthalmology Emergency Service with open globe trauma between July 2011 and January 2020 were searched. Patients with less than a 6-month follow-up were not included in the study. The electronic medical records were reviewed by two of the authors (GVSF and AMMK) using standardized abstraction forms to guide data collection. The retrieved data included age, gender, circumstance and time of injury, time elapsed from the traumatic event to surgery, type of penetrating injury, initial VA at presentation, final VA at the last follow up visit, and concomitant eye disease. Additional signs and ocular comorbidities that were collected and used to calculate the scores included hyphema, iris organic/unclean injury, prolapse, traumatic cataract, retinal detachment, vitreous hemorrhage, delay of surgery > 48 hours, and endophthalmitis. In order to mitigate potential sources of bias, an effort was made to first establish that the minimal necessary information was available in the charts, there were enough patients to perform the analysis with adequate precision, and that the predictor and outcome variables were defined a priori.
Score calculations and statistical analysis
The POTS was calculated according to Acar et al. [8]. For each child, the initial VA at presentation was assigned as raw points, and additional points were added or subtracted for wound location, age, and any of eight concomitant eye conditions. In those patients whose initial VA was not available from the medical records, the following equation was used to determine the trauma score: [8] VA = 2 × (age+zone)-corresponding pathologies
Open globe injuries were stratified according to anatomical location into three zones: limited to the cornea and limbus (zone I); located within 5 mm posterior to the limbus (zone II); and if the wound was extended to the macula and optic nerve, posterior to zone II (zone III) [16]. The patients were stratified into five groups based on the POTS value as group 1, < 45 points; group 2, 46–64 points; group 3, 65–79 points; group 4, 80–89 points; and group 5, 90–100 points. A lower score was presumed to have a worse prognosis.
The TOTS was calculated using high-risk characteristics of injury: wound > 6 mm (1 point), hyphema (1 point), cataract/lens damage (1 point), retinal detachment (2 points), and choroidal detachment (1 point) [15]. If the TOTS was 0 or 1, then the injury was categorized as a low risk (better prognosis); if 2 or higher, as a high risk (worse prognosis) [15].
To facilitate statistical comparison of the two scoring systems, we defined a VA of 20/40 as the cut-off value for assigning POTS values into TOTS categories 1 (low risk) or 2 (high risk). Thus, the POTS categories 1 to 4 were merged into a high-risk category corresponding to the TOTS category 2 and the POTS category 5 corresponded to a low-risk TOTS [15]. To evaluate the predictive value of both scores—a patient achieving a final outcome of VA 20/40 or better—the final VA achieved for each patient was compared with the predicted VA using Fisher exact test of independence. The sensitivity, specificity, and accuracy, with 95% confidence intervals (CIs), were compared by the McNemar test. The significance level was set at P < 0.05.
RESULTS
Patients' characteristics
Thirty patients were included in the study. The mean age was 3.9 ± 1.6 years (range, 0–6 years); 20 (66.6%) were male patients and 10 (33.3%) were female patients. Sixteen patients had the right eye injured, and 14 had left eye injuries. Blunt objects accounted for 50% of all causes of injury, including infliction by wood, metal, stick, stone, lamp, nonintentional assault (kick or punch), or pliers tool. The other significant causes were glass (10.7%), sharp objects (10.7%), toys (7.1%), pencil (3.5%), knife (3.5%), and fireworks (3.5%); in seven patients, the cause of injury was not reported.
The initial VA at presentation was no light perception in two patients (6.7%), hand motion in one (3.3%), counting fingers in one (3.3%), between 20/200 and 20/40 in five (16.7%), > 20/40 in one (3.3%); in 18 (60.0%), VA could not be adequately determined or the information was not available.
The initial diagnosis at the first visit were iris prolapse in 10 patients (33.3%), traumatic cataract in 10 (33.3%), hyphema in eight (26.7%), vitreous hemorrhage in three (10.0%), open globe injury > 6 mm in three (10.0%), and retinal detachment in one patient (3.3%). No patient presented with endophthalmitis or choroidal detachment. There were 28 wounds (93.3%) located in zone I, two (6.6%) in zone II, and none in zone III.
All patients underwent primary surgery for reconstitution of globe integrity and repositioning of the ocular tissues whenever possible, at the surgeon’s discretion. The time between the initial evaluation and surgery was < 48 hours in 27 patients (90%) and was delayed for more than 48 hours in three (10%). The mean follow-up period was 7.9 ± 1.8 months (range, 6.0–12.1 months).
Score results
Table 1 depicts the final achieved VA according to each TOTS category. Only seven patients in the low-risk category achieved VA 20/40 or better. Conversely, in the high-risk category, three achieved no light perception and two light perception/hand motion/count fingers. Table 2 shows the comparison between the final achieved VA and the predictive VA according to the POTS. For the POTS category 1 (worse prognosis), six patients remained at no light perception; three achieved better VA, and one patient achieved 20/40 or better. All four patients in category 3 achieved 20/40 or better VA, as initially predicted.
Table 3 depicts the comparison of the POTS and TOTS predictive values for 20 patients whose final VA was available from the medical records. The comparison did not show a statistically significant association between the predictive POTS VA and achieved VA (P = 0.350), or between the predictive TOTS VA and achieved VA (P = 0.083). The sensitivity for the POTS was higher than that of the TOTS (100%; 95% confidence interval [CI], 75.3–100 vs. 61.5%; 95% CI, 31.6–86.1; P = 0.014) (Table 4). The specificity was not significantly different (14.3%; 95% CI, 0.4–57.8 vs. 0%; 95% CI, 0–41.0; P = 0.563). The accuracy for the POTS was higher than the TOTS (70.0%; 95% CI, 45.7–88.1 vs. 40.0%; 95% CI, 19.1–63.9; P = 0.001).
DISCUSSION
The majority of patients with eye trauma were boys, concurring with previously reported data in most studies [1,4-8,11-15]. This might be due to the play behavior of boys. As to the causative object, most patients were injured by blunt objects. In most studies, however, sharp objects are the most frequent cause of open globe injuries. The mechanisms of injury have geographic characteristics involving both cultural and socioeconomic aspects. The Santa Casa de Sao Paulo is a charity hospital to which highly complex cases of trauma are referred. It is located at a densely populated urban area; the majority of patients are uninsured and from low-income families. Most parents cannot afford regular toys; children play with whatever they find available, and they could be injured by accidental physical confrontation when playing with each other. These might explain the mechanism of injury findings in the study.
Open globe wounds are probably the most severe eye injuries. In this sample, however, most wounds were located in the cornea and limbus (zone I) accompanied by iris prolapse, cataracts, and hyphema. Few patients had vitreous hemorrhage and retinal detachment, and none presented with choroidal hemorrhage that would be expected in posterior open globe injuries (zones II and III). Moreover, no patient developed endophthalmitis; this might be attributable to early intervention, since the majority of patients received surgery less than 48 hours from injury.
In this study the TOTS had limited value as predictors of VA in children younger than 6 years with open globe injury. The POTS was more accurate as compared to the TOTS. The POTS had a tendency to be more sensitive than the TOTS in predicting the final VA after treatment.
Both the POTS and TOTS are prognostic models for predicting the possibility of a patient with open globe injury to attain a specific VA after treatment. They do not rely on VA at presentation, which is virtually impossible in preverbal children and difficult in older children; anxiety due to the circumstances in the emergency room cause VA information to be imprecise [6,13]. The POTS includes 10 variables to assess visual prognosis: age, wound location, and 8 different concomitant eye conditions. According to the score, patients are grouped into five categories, where higher points are presumed to predict a better prognosis [8]. In comparison, the TOTS is calculated using 5 high-risk characteristics of the injury: a wound larger than 6 mm, hyphema, lens damage, choroidal, and retinal detachment. The injury is categorized as a high risk if the score is ≥ 2 or a low risk if it is 0 or 1; in the latter case, the patient has a greater chance to attain a VA of 20/40 or better. The TOTS uses fewer variables than the POTS; however, the score included only those variables found to have the largest odds ratio in the study [14]. Previous studies have determined additional risk factors for poor visual prognosis, including blunt injury, posterior zone of injury, vitreous hemorrhage, and injury to the posterior segment [11,12]. We cannot assert that the inclusion of other prognostic factors of poor outcomes would change the predictive performance of the TOTS, but that is a real possibility.
The sample in this study comprised children who sustained less-severe injuries, as compared to the Read and Cavuoto study [15]. Most patients (93.3% vs. 64%) had an open globe injury located in zone I, no patient had an intraocular foreign body (vs. 11%), there were no choroidal detachments (vs. 39%), 3.3% had retinal detachment (vs. 11%), 33.3% had uveal prolapse (vs. 93%), and 33.3% had cataracts (vs. 43%). This might suggest that the accuracy of the TOTS for predicting visual outcome is inferior in a sample of children with less-severe or moderate trauma.
Among patients with final VA data, only 7 of 20 patients (35%) achieved a final VA of 20/40 or better in the study. This is somewhat low given the nature and severity of the injuries. Most patients sustained moderate trauma, and surgical intervention was performed early in most cases. One hypothesis is that many patients developed amblyopia. This is a major concern in children with eye trauma, since it can develop relatively fast. Prompt visual recovery, with prescription of adequate optical correction and patching the of fellow eye in the critical period, is necessary for visual rehabilitation and development of stereopsis [17]. In this study, the follow-up period was short, and some patients might not have had enough time to undergo specific treatment for amblyopia. Some might have had a potential for a better final VA if they had the opportunity for adequate treatment and a longer follow-up period. To some extent, this observation might have influenced the results, possibly diminishing the accuracy, sensitivity, and specificity rates of both scores.
This study has some limitations. First, this was a hospital-based retrospective cohort study. Since, retrospective observational studies use data that were originally collected for other purposes, not all the relevant information may have been available for analysis [18]. In this regard, the final VA of 10 patients was not available in the records. In addition, retrospective studies are subject to historical, statistical, and mortality threats to validity, which limit the interpretation and generalizability of the results [18]. Second, our sample size was relatively small. However, the sample was representative of the incidence of open-globe trauma in this age range, electronic hospital files before 2011 were not accessible for research at our institution, and previous studies also had fewer than 30 patients [7,14,15]. Third, the TOTS is a simplified binary system for standardized assessment with only two categories, whereas the POTS is a 1 to 5 scale score. In the study, it was decided to merge the POTS categories 1 to 4 into one single category in order to make it comparable with the TOTS, and 10 patients (five in category 2, four in category 3, and one in category 4) were downgraded to a lower category. By assigning patients with a better final VA into a lower POTS category, which should predict a lower final VA, one could mistakenly cause categories 2, 3, and 4 to underestimate the predictive VA and, therefore, decreasing the sensitivity.
In summary, both the POTS had fair accuracy as predictive instruments for estimating the final VA in Brazilian children with open globe trauma; the POTS tended to be more accurate than was the TOTS. Especially in preverbal children, or in situations where an initial VA cannot be evaluated adequately, both the POTS can be used to evaluate visual prognosis in pediatric open globe injury.
Notes
No potential conflict of interest relevant to this article was reported.
References
Article information Continued
Notes
Capsule Summary
What is already known
In clinical practice, the emergency physician is frequently inquired by parents what are the odds of their child to be able to see again. The Pediatric Penetrating Ocular Trauma Score (POTS) and Toddler/Infant Ocular Trauma Score (TOTS) are scores that guide doctors to estimate prognosis and answer the parents questions.
What is new in the current study
The POTS had fairly better accuracy as predictive instrument to estimate final visual acuity in children with open globe injury when compared to TOTS. POTS was more sensitive as compared to TOTS.