Macklin effect in acute asthma exacerbation
Article information
A 25-year-old male patient presented with persistent cough and deteriorating dyspnea. He regularly used short-acting beta2-agonist inhalers for asthma. Arterial blood gas analysis revealed hypoxemia (PaO2 62 mmHg). Spirometry showed that the forced expiratory volume in 1 second (FEV1) was 30%, the forced vital capacity (FVC) was 60%, and the FEV1 to FVC ratio was 55% of predicted values. Chest computed tomography demonstrated a small pneumomediastinum (Fig. 1). He received nebulized long-acting beta2-agonists, muscarinic antagonists, corticosteroids, and oxygen therapy. He was discharged 3 days later. Repeat imaging revealed no evidence of pneumomediastinum, and spirometry values were unremarkable. Written informed consent for publication of the research details and clinical images was obtained from the patient.
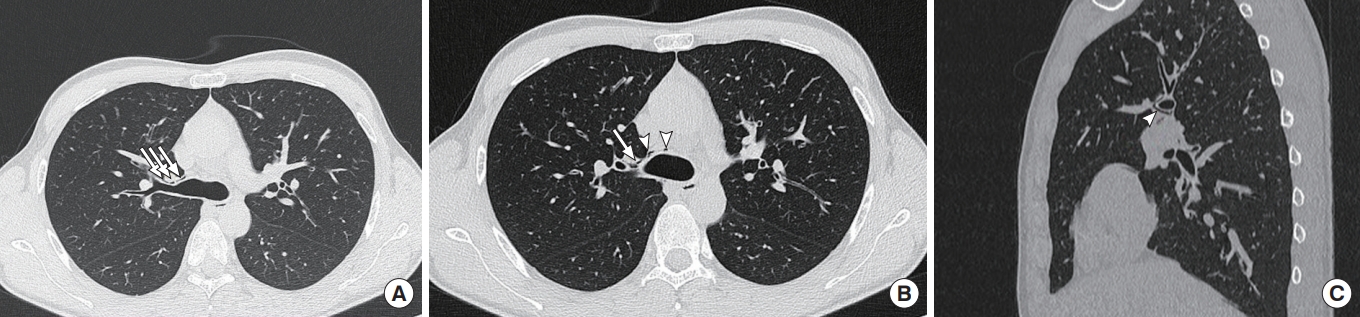
Axial chest computed tomography image (lung window) showing (A) linear collection of air (arrows) adjacent to the bronchovascular sheath (Macklin effect) and (B) centripetal spread of air along the bronchovascular sheath to the right hilum (arrow) and to the mediastinum (arrowheads). (C) Sagittal chest computed tomography image (lung window) showing the presence of air around the right main bronchus (arrowheads).
Macklin [1] first described the “Macklin effect” in 1939; this explains the pathophysiology of spontaneous pneumomediastinum, which occurs when air leaks through small alveolar ruptures to the surrounding bronchovascular sheaths and spreads into the mediastinum. Spontaneous pneumomediastinum happens in 1 in 8,000 to 1 in 42,000 of emergency admissions, with common triggers including acute asthma exacerbation, respiratory tract infection, strenuous physical activity, coughing, and vomiting [2,3]. The presence of air in the pulmonary interstitium and adjacent to the bronchovascular sheaths strongly suggests the Macklin effect and obviates the need for further diagnostic investigations.
To avoid unnecessary hospitalization of patients with spontaneous pneumomediastinum, Okada et al. [4] have proposed a five-question guide. Patients without temperature >38°C, oxygen saturation <96%, progressive symptoms, vomiting at the onset, and anxiety are eligible for ambulatory care. The present case illustrates the self-limited nature of spontaneous pneumomediastinum by demonstrating rapid and complete resolution with conservative management. Follow-up imaging may not be needed in selected patients.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
FUNDING
None.
References
Article information Continued
Notes
Capsule Summary
What is already known
The Macklin effect explains the pathophysiology of spontaneous pneumomediastinum, which can be observed in acute asthma exacerbation.
What is new in the current study
Spontaneous pneumomediastinum is usually self-limited.
