Neurologic outcomes of prehospital mechanical chest compression device use during transportation of out-of-hospital cardiac arrest patients: a multicenter observational study
Article information
Abstract
Objective
High-quality cardiopulmonary resuscitation with chest compression is important for good neurologic outcomes during out-of-hospital cardiac arrest (OHCA). Several types of mechanical chest compression devices have recently been implemented in Korean emergency medical services. This study aimed to identify the effect of prehospital mechanical chest compression device use on the outcomes of OHCA patients.
Methods
We retrospectively analyzed data drawn from the regional cardiac arrest registry in Daegu, Korea. This registry prospectively collected data from January 2017 to December 2020. Patients aged 18 years or older who experienced cardiac arrest presumed to have a medical etiology were included. The exposure variable was the use of a prehospital mechanical device during transportation by emergency medical technicians. The outcomes measured were neurologic outcomes and survival to discharge. Logistic regression analysis was used.
Results
Among 3,230 OHCA patients, 1,111 (34.4%) and 2,119 (65.6%) were managed with manual chest compression and with a mechanical chest compression device, respectively. The mechanical chest compression group showed poorer neurologic outcomes than the manual chest compression group (adjusted odds ratio, 0.12; 95% confidence interval, 0.04–0.33) and decreased survival to discharge (adjusted odds ratio, 0.39; 95% confidence interval, 0.19–0.82) after adjustment for confounding variables.
Conclusion
Prehospital mechanical chest compression device use in OHCA was associated with poorer neurologic outcomes and survival to discharge compared to manual chest compression.
INTRODUCTION
Out-of-hospital cardiac arrest (OHCA) is a global health issue; approximately 347,000 adult OHCA patients are assessed by emergency medical services (EMSs) each year in the United States, and approximately 30,000 cases of OHCA occur annually in Korea [1-3]. High-quality cardiopulmonary resuscitation (CPR) (i.e., chest compression with adequate depth, rate, chest recoil, and minimal hands-off time) is an important factor for return of spontaneous circulation and favorable neurologic outcomes [4-7]. In previous randomized controlled trials or meta-analysis studies, the use of mechanical chest compression was not shown to improve neurologic outcomes compared to manual chest compression in OHCA [8-11].
Although prehospital use of mechanical chest compression devices has no benefit in the outcomes of OHCA patients, their use can be considered in special situations, such as in an ambulance, during coronary angiography, during extracorporeal CPR, or when there is a risk of exposure to an infectious disease such as COVID-19 [12,13]. In addition, rescuer fatigue might lead to inadequate chest compression rates and depth [14,15]. Thus, mechanical chest compression devices can have the advantage of providing continuous, high-quality chest compression during transportation, characterized by minimal compression hands-off time and constant depth of compression and relaxation. This has led to introduction of these devices to prehospital EMS in Korea. Several types of mechanical chest compression devices have been introduced to prehospital EMS, but only a limited number of studies has assessed their effectiveness.
In this study, we aimed to identify trends in the frequency of use and outcomes of mechanical chest compression devices in EMS and to compare the outcomes of OHCA patients managed with prehospital mechanical chest compression devices to those managed with manual chest compression.
METHODS
Study design and participants
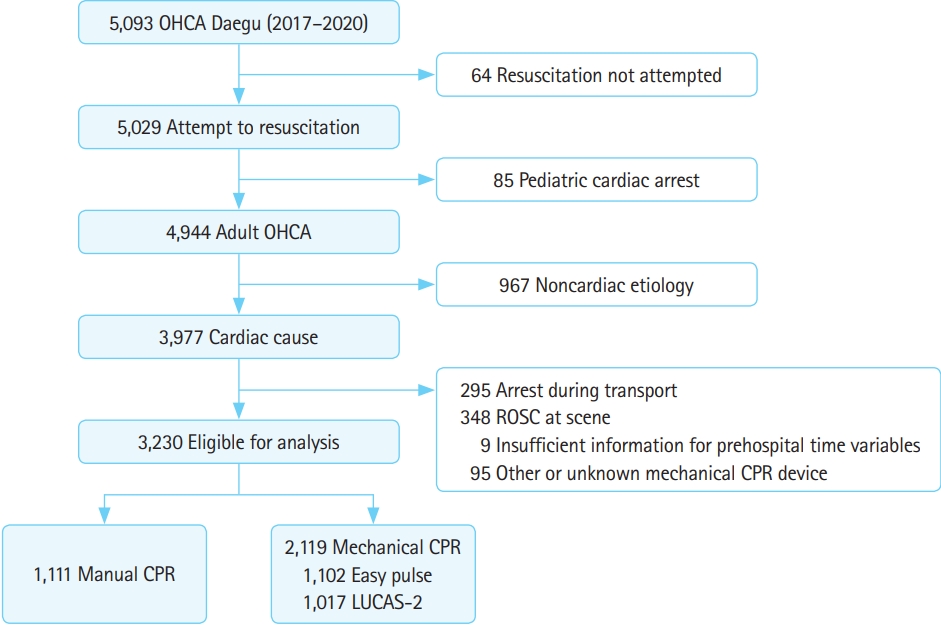
This is a retrospective observational study that used data from the regional cardiac arrest registry in Daegu. We included patients aged 18 years or older who experienced cardiac arrest that was presumed to have a medical etiology in Daegu from January 2017 to December 2020. The exclusion criteria used for patients further screened were no attempt at resuscitation (n=64), younger than 18 years (n=85), the arrest had a noncardiac etiology (n=967), OHCA occurred in the ambulance during transport (n=295), prehospital return of spontaneous circulation occurred at the scene (n=348), insufficient information of prehospital variables was available (n=9), mechanical compression devices of unknown origin were used (n=84), and other devices were used (n=11) (Fig. 1). This study was approved by the Institutional Review Board of Kyungpook National University Hospital (No.2016-03-027). The Institutional Review Board waived the need for written informed consent.
Study setting
Daegu has a population of 2.4 million and an area of 883.51 km2. The Korean prehospital EMS is operated by a single provincial fire department supported by eight local EMS agencies with 50 ambulance stations and a single unified dispatch center [16]. Mechanical chest compression devices were first introduced in November 2016, and there are currently a total of 55 devices being used in Daegu EMS: 34 from Easy Pulse (Schiller, Baar, Switzerland) and 21 from LUCAS-2 (Jolife AB, Lund, Sweden).
Each prehospital EMS team is comprised of two to three emergency medical technicians (EMTs), including a level 1 EMT (similar to intermediate level EMTs in the EMS of the United States) as the top-level ambulance crew, a level 2 EMT (similar to basic level EMTs), and a driver [16-18]. For both EMTs, the scope of practice is limited to the basic level of life support; for some EMTs who completed an advanced training course after September 2019, the scope of practice can be expanded to include intravenous epinephrine administration during CPR under medical oversight. In March 2015, the dual-dispatch system was initiated in Daegu EMS to reduce response time and increase the number of EMTs responding to OHCA cases [17]. Since March 2017, EMS medical directors have regularly facilitated team CPR training programs to enable a well-coordinated team approach with predefined roles for each EMT [16]. This team CPR program includes training with equipment to provide high-quality CPR (i.e., end-tidal CO2 equipment, CPR feedback device, video-laryngoscopy, and mechanical compression device) as well as scenario-based dual-dispatch CPR training. In the team program, CPR was practiced by applying a mechanical chest compression device before scene departure to provide high-quality CPR during transport in cases of dual dispatch. CPR was performed according to the Korean fire department EMS protocol and the team CPR protocol, and a mechanical chest compression device was applied immediately before transportation. The mechanical chest compression device was applied to the patient by EMTs according to availability of the chest compression device in the ambulance, field situation, and team CPR protocol.
Data source and variables
We used the regional OHCA registry, which includes all OHCA cases of level 1 and 2 hospitals in Daegu [16-19]. Data were retrieved from the EMS run sheets for basic ambulance operational information, the EMS CPR registry, the dispatcher CPR registry, and the hospital OHCA registry for hospital care and outcomes.
We analyzed the following data: demographic information (i.e., age, sex, and past medical history); community factors (i.e., presence of a witness, CPR by a bystander, location of the arrest, and primary electrocardiogram rhythm at the scene); EMS factors (i.e., activation of the dual-dispatch system, details of EMS resuscitation including defibrillation and epinephrine administration, and prehospital advanced airway management by EMTs); time variables (i.e., response time interval, scene time interval, transport time interval, duration between collapse and initiation of CPR, and duration between initiation of CPR and end of resuscitation efforts); and hospital treatments (i.e., target temperature management [TTM], percutaneous coronary intervention [PCI], and extracorporeal membrane oxygenation [ECMO]).
Outcome measures
The primary outcome measured was neurologic outcome. “Good” outcome was defined as cerebral performance category 1 (alert, conscious, able to work, and possibly having a mild neurologic or psychological deficit) or cerebral performance category 2 (conscious, sufficient cerebral function for independent activities of daily life, and able to work in a sheltered environment). The secondary outcome was survival to discharge. Each outcome was reviewed based on hospital records.
Statistical analysis
Demographics and outcomes of the study population were compared. These were also analyzed among subgroups of types of mechanical chest compression devices used. Descriptive statistics are presented as medians with interquartile ranges (25th and 75th percentiles), while categorical variables are presented as counts and percentages. The significance of the differences between the two groups was analyzed using the Mann-Whitney U-test for continuous variables and the chi-square test for categorical variables. All trends were tested by the Cochran-Armitage test.
Associations between the study groups and outcomes were assessed using logistic regression analysis. We included potential confounding variables of demographic factors (i.e., sex, age, and presence of comorbidities); arrest characteristics (i.e., witness status, primary electrocardiogram rhythm, and location of arrest); prehospital time variables (i.e., response time interval, scene time interval, and transport time interval); EMS resuscitation procedures (i.e., prehospital airway management, prehospital epinephrine administration, and dual dispatch); and postresuscitation hospital management (i.e., PCI, TTM, and ECMO). Logistic regression analysis was performed to analyze associations between study groups and outcomes according to initial electrocardiogram rhythm, as shown in Supplementary Table 1. The results are expressed as adjusted odds ratios (AORs) and 95% confidence intervals (CIs). All statistical analyses were performed with SAS ver. 9.4 (SAS Institute Inc., Cary, NC, USA). Based on a two-sided test, P<0.05 was considered statistically significant.
RESULTS
Demographic analysis
Among 3,230 patients eligible for analysis, 1,111 and 2,119 were managed with manual compression and mechanical compression, respectively (Fig. 1 and Table 1). The demographic analyses of each study group are shown in Table 1. The mechanical compression group had smaller proportions of witnessed arrest and prehospital bag-valve mask ventilation but a larger proportion of dual-dispatch and prehospital epinephrine administration than did the manual compression group. Scene time interval, time from arrival to departure from the scene, was also longer in the mechanical compression group. Overall, 3.4% and 0.5% of patients in the manual compression and mechanical compression groups, respectively, had good neurologic outcomes.
Trend analysis
The rate of mechanical chest compressions during transport in OHCA patients tends to increase every year (P<0.001). Annually, the proportion of patients with good neurologic outcomes showed an increasing trend for the manual chest compression group (P=0.002), but a plateau was observed in the mechanical compression group (P=0.598) (Fig. 2A). Similarly, the rate of survival to discharge in the manual compression group showed an increasing trend over time, but no significant trend was seen in the mechanical compression group (Fig. 2B).
Subgroup analysis
The subgroup analysis according to the type of mechanical compression device used is shown in Table 2. Among 2,119 patients in the mechanical chest compression group, Easy Pulse and LUCAS-2 were used in 1,102 and 1,017 patients, respectively. The proportions of patients with good neurologic outcome in the Easy Pulse and LUCAS-2 groups were 0.5% and 0.6%, respectively (P=0.663).
Main analysis
Overall, patients treated with mechanical chest compression devices had worse neurologic outcomes (AOR, 0.12; 95% CI, 0.04–0.33) than patients with manual compressions. There was also a lower survival to discharge ratio in the mechanical chest compression group (AOR, 0.39; 95% CI, 0.19–0.82) compared to the manual chest compression group after adjusting for confounders (Table 3).
DISCUSSION
We evaluated the types and trends of mechanical chest compression device use during OHCA in patients and analyzed its association with neurologic outcomes and survival. With the introduction of mechanical chest compression devices, such as Easy Pulse and LUCAS-2, in prehospital ambulances, their use during transport has been increasing. However, use of a mechanical chest compression device during transport was associated with poorer neurological prognosis (AOR, 0.12; 95% CI, 0.04–0.33) and survival (AOR, 0.39; 95% CI, 0.19–0.82) compared to manual chest compression.
The 2020 American Heart Association CPR guidelines and the Korean CPR guidelines suggest that mechanical chest compression be considered in special situations, such as having a small number of staff who can perform CPR, being in an ambulance, during coronary angiography, during extracorporeal CPR, or when there is a risk of exposure to infectious diseases such as COVID-19 [12,13,20]. The guidelines emphasize that interruption of chest compressions could be minimized with use of a mechanical chest compression device [12]. However, few studies have analyzed neurologic and survival outcomes related to the use of a mechanical chest compression device in OHCA patients immediately prior to transfer and departure from the scene. In this study, a team CPR training program for EMTs was conducted every year on proper use of the mechanical chest compression device of the local ambulance. Based on dual-dispatch, CPR was performed at the scene according to the fire department EMS protocol of Korea and applied during the transfer process immediately prior to departure. This study was conducted based on regional cardiac arrest registry data reflecting the actual use of the EMS mechanical chest compression devices in the region. Therefore, our study is meaningful because the comparison of outcomes between mechanical chest compression devices and manual chest compressions was contextualized according to a regional prehospital protocol for OHCA patients. In addition, this study might assist in the establishment of an EMS strategy in the region.
In this study, use of a mechanical chest compression device during transport of OHCA patients was associated with poor neurological prognosis. Despite differences in the type and application protocol of chest compression devices, the AutoPulse Assisted Prehospital International Resuscitation Trial reported favorable neurological prognosis at hospital discharge in 3.1% and 7.5% of patients managed with the automated load distributing band (LDB) chest compression device and manual CPR, respectively. In that study, the LDB-CPR group reported poorer neurological prognosis than manual CPR patients, similar to the results of our study [21]. Hallstrom et al. [21] reported that the poor neurological prognosis of the LDB-CPR group could be a result of the Hawthorne effect, in which the quality of manual CPR was higher than average and because the mechanical device takes longer to set up. In a video-recording and time-motion study performed during resuscitation in the emergency department, an average of 122.6 seconds was required to apply the mechanical chest compression device, and approximately 72.7% of the time elapsed was reported as no-flow time [22]. Thus, in this study, application of a mechanical chest compression device in the field was possibly associated with increased no-flow time. Considering that the median transport time interval was 6 minutes in an EMS in a large city with a relatively shorter transport time than in a rural area, application of mechanical chest compression devices during transport might not have benefited the chest compression fraction.
Another possible explanation is that the mechanical chest compression device was displaced from the proper position during transport. A randomized crossover manikin study by Blomberg et al. reported that, during CPR, the rate of compressions with sufficient depth among total chest compressions was lower with the mechanical chest compression device than with manual CPR (58% vs. 88%). It is suggested that the mechanical chest compression device may have been affected by changes from the proper position of chest compression during application [23]. Our study showed that the rates of favorable neurological prognosis and survival at discharge have been increasing yearly in the manual chest compression group, but these rates remained constant in the mechanical chest compression device group. Each year, paramedics are periodically educated regarding OHCA, proper application of mechanical chest compression devices, and team CPR; but the effectiveness of this training might not have been sufficient. The training process should further emphasize the importance of reducing no-flow time and maintaining appropriate chest compression position during application. Also, assessment and feedback regarding EMT proficiency are necessary.
This study has several limitations. First, as a retrospective observational study, selection and information biases might have occurred. Second, there might have been differences in chest compression quality and team CPR performance depending on the individual capabilities of the EMT and paramedics; additional information to evaluate the quality of CPR (e.g., chest compression fraction) was not provided. Third, although team CPR training was conducted every year, there was no assessment of EMT proficiency before and after training or annually. It also is possible that the effectiveness of the training in mechanical device use for EMTs was insufficient. Fourth, there can be differences between hospitals in quality of CPR and in postcardiac arrest treatment capacity (i.e., TTM, ECMO, and PCI). These factors can influence the patient’s neurological prognosis. Last, there are inherent differences between EMS, out-of-hospital CPR protocols, and EMTs; therefore, consideration of these is necessary before generalizing and applying these findings to other regions or countries.
In conclusion, use of mechanical chest compression devices during transport of OHCA patients was associated with poorer neurological and survival outcomes at discharge compared to manual chest compressions. When applying a mechanical chest compression device during transport, paramedics should be trained to minimize interruption of chest compressions and to maintain the device at an appropriate position.
SUPPLEMENTARY MATERIAL
Effect of mechanical cardiopulmonary resuscitation on out-of-hospital cardiac arrest outcomes according to initial electrocardiogram rhythm
Supplementary materials are available at https://doi.org/10.15441/ceem.21.142.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
FUNDING
None.
References
Article information Continued
Notes
Capsule Summary
What is already known
Although prehospital use of mechanical chest compression devices has no benefit in the survival and neurologic outcomes of out-of-hospital cardiac arrest patients, their use can be considered in special situations, such as in an ambulance, during coronary angiography, during extracorporeal cardiopulmonary resuscitation, or when there is a risk of exposure to an infectious disease.
What is new in the current study
With the introduction of mechanical chest compression devices in prehospital emergency medical services, their use during prehospital transport has increased annually in Korea. The use of mechanical compression devices during transport is associated with worse neurologic outcomes and survival to discharge than is manual compression.