Interactive effect of multi-tier response and advanced airway management on clinical outcomes after out-of-hospital cardiac arrest: a nationwide population-based observational study
Article information
Abstract
Objective
We hypothesized that a multi-tier response (MTR) will provide high-quality cardiopulmonary resuscitation including airway management. However, the type of tier response system and airway management will have different interactive effects resulting in varying outcomes following out-of-hospital cardiac arrest (OHCA). This study aimed to determine whether the advanced airway management method has an effect on OHCA outcomes and to compare the size of the effect across MTR types.
Methods
This is a retrospective population-based observational study using the Korea OHCA Registry. Airway management methods were categorized into endotracheal intubation (ETI) and supraglottic airway (SGA) groups. The tier system was categorized into single-tier response (STR) or two types of MTR: ambulance-ambulance MTR or fire engine-ambulance MTR.
Results
In total, 45,264 patients were analyzed among the 89,087 emergency medical service assessed OHCAs. The SGA group was significantly associated with a lower prehospital return of spontaneous circulation (ROSC) rate compared to the ETI group (adjusted odds ratio [aOR], 0.79; 95% confidence interval [CI], 0.72–0.88). Both MTR with an ambulance or fire engine were significantly associated with higher prehospital ROSC rates compared to STR (STR vs. MTR with an ambulance: aOR, 1.33; 95% CI, 1.21–1.47; STR vs. MTR with a fire engine: aOR, 1.43; 95% CI, 1.20–1.71). Prehospital SGA was significantly associated with poor neurological outcomes in MTR with fire engine (aOR, 0.71; 95% CI, 0.53–0.96).
Conclusion
In this nationwide observational study, we observed that MTR was associated with higher prehospital ROSC than STR. Moreover, SGA is associated with a lower prehospital ROSC rate regardless of tier response type compared to ETI.
INTRODUCTION
Out-of-hospital cardiac arrest (OHCA) is a major public health burden due to its low survival rate and severe neurological disability [1]. The rate of survival to hospital discharge after OHCA was 10.4% in the US and 0.5% to 8.5% in the Pan-Asian population [1,2]. Primary compositions of high-quality cardiopulmonary resuscitation (CPR) including early defibrillation, uninterrupted chest compression, and optimal airway management are associated with the return of spontaneous circulation (ROSC) and prevention of neurological impairment [3].
The selection of prehospital optimal airway management is inconclusive. Bag-valve mask (BVM) ventilation is commonly used until advanced airway management such as endotracheal intubation (ETI) or supraglottic airways (SGAs) insertion can be applied. In general, ETI was regarded as the standard airway management during OHCA to provide controlled oxygenation and to protect the lungs from vomitus [4-6]. However, prehospital ETI is a complex task and requires the coordination of multiple actions. Therefore, international recommendations suggest that ETI should be performed by operators with adequate experience and skills [3,7]. Prehospital ETI may worsen patient outcome when associated with delays in basic life support (BLS) procedures, interruptions in chest compressions, or unrecognized esophageal intubation [8,9].
A recent multicenter trial by Wang et al. [10] showed that initial laryngeal tube insertion was associated with a greater survival rate in OHCA patients compared to initial ETI. However, the AIRWAYS-2 randomized clinical trial, which compared ETI and SGA, reported that SGA did not show favorable functional outcomes [11]. Hence, there is no consensus on the optimal method of initial airway management during OHCA.
A nationwide dispatcher-assisted CPR program and multi-tier response (MTR) service have been implemented in Korea since 2015. Prehospital advanced airway management was more widely applied after the implementation of the MTR system [12]. However, it is uncertain whether the type of tier response and advanced airway method is associated with better outcomes.
We hypothesized that the MTR would provide a higher quality of CPR and airway management. However, the combination of the tier response system and airway management may have different interactive effects resulting in varying outcomes after OHCA. This study aimed to determine whether the airway management method has an effect on outcomes after OHCA and to compare the size of the effect across the types of MTR.
METHODS
Ethics statement
This study was approved by the Institutional Review Board of Seoul National University Hospital (No. 1103-153-357). Informed consent was waived, and patient information was anonymized before analysis. The Korea Centers for Disease Control and Prevention (KCDC) released the national OHCA registry data for public health [13].
Study design, setting, and data sources
This retrospective study is a population-based observational study using the Korea OHCA Registry (KOHCAR). The KOHCAR has been operated by the KCDC in collaboration with the central fire services since 2006. The Korean emergency medical services (EMSs) system is a government-operated, two-tiered, and dual dispatch system that offers basic to intermediate levels of life support ambulance services from fire stations. According to regional resources, the first response service plus intermediate life service (ILS) or ILS plus ILS models were widely accepted for the MTR (Fig. 1). The fire engine service provides BLS only and the ambulance with a level-1 emergency medical technician (EMT) provides advanced cardiovascular life support. For on-scene CPR protocol, at least 5 minutes of full resuscitative efforts delivered by an EMT is recommended before patient transportation. Prehospital ETI or SGA can be performed only by a level-1 EMT under direct or indirect medical oversight during OHCA. There is no specific protocol for the selection of the advanced airway method or cooperation between the two groups of the MTR. Moreover, EMTs are unable to terminate resuscitation attempts in the field unless the OHCA patient shows obvious signs of death such as decapitation, decomposition, or rigor mortis. Thus, nearly all EMS-assessed OHCA patients in Korea are transported to the closest emergency departments (EDs) regardless of prehospital ROSC status.
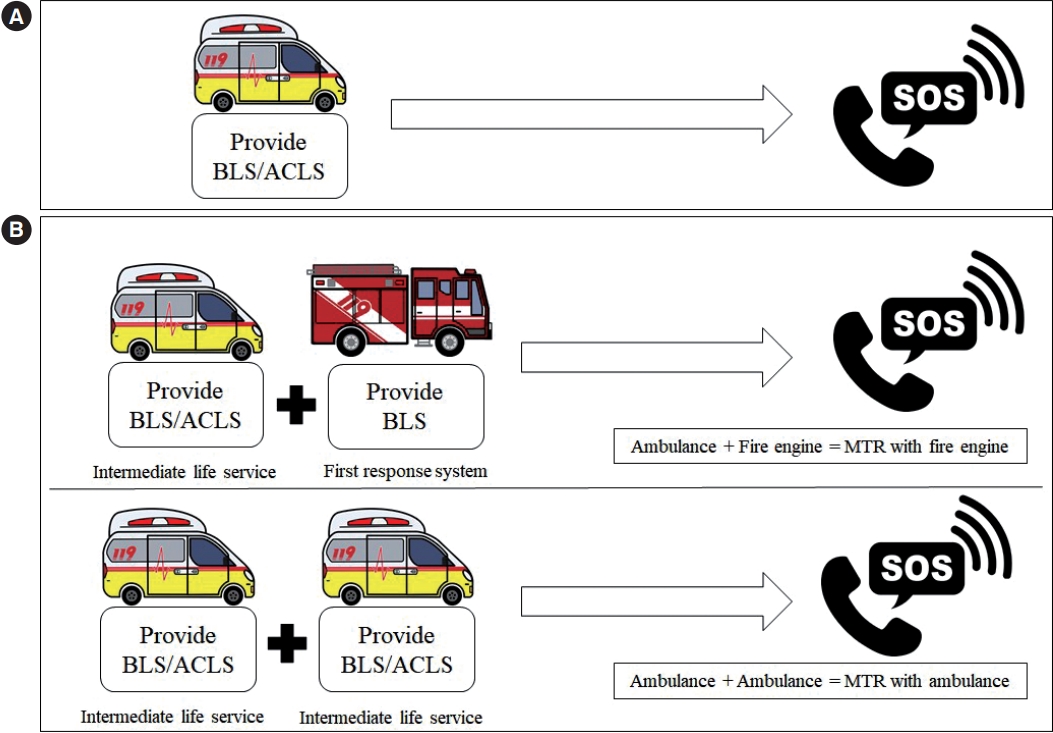
Tiered emergency medical services response system in Korea. (A) Single-tier response and (B) multi-tier response system (MTR) in Korea. BLS, basic life support; ACLS, advanced cardiovascular life support.
The dataset was integrated from the following four sources: EMS run sheets for basic ambulance operation information, EMS cardiac arrest registry, dispatcher CPR registry for the Utstein factors, and the national OHCA registry for hospital care and outcomes. The EMS providers recorded the EMS run sheets and cardiac arrest registry for all EMS-assessed OHCA. Medical record reviewers from the KCDC retrieve the recorded clinical information from approximately 700 hospitals [14,15].
A two-step management of data quality was performed to ensure the quality of the medical record review process. First, the EMTs were educated with EMS data recording through the data dictionary of EMS record variables and education program. Moreover, the EMTs were supervised for each case by EMS medical directors during education. Second, the hospital medical record reviewers were trained on the use of the data dictionary and case review protocols and were dispatched to all hospitals to gather information on hospital care and outcomes. The two-step quality management was supported by the committee members, which consisted of EMS physicians, epidemiology and statistical experts, cardiologists, and medical record review experts. The data quality management reviewed almost all collected data and gave monthly feedback [16].
Study population
This study included adult EMS-assessed OHCA patients with presumed cardiac etiology, who were not witnessed by EMS providers and/or were defibrillated by a bystander or automated external defibrillation. The study period was from January 2017 to December 2019. Exclusion criteria were age under 18 years, a noncardiac origin of arrest, resuscitation not attempted in ED, witnessed by EMT, and a BVM or unknown airway management method.
Variables
Airway management methods were categorized into the following two groups: ETI and SGA. The tier system was divided into single-tier response (STR) and two types of MTR: ambulance-ambulance MTR and fire engine-ambulance MTR [17].
The main exposure was the airway management method and co-exposure was the tier response type. We analyzed the impact of the airway management method and tiered response type on clinical outcomes.
We assessed all potential confounders including age, sex, residential area, bystander CPR, location of arrest, initial electrocardiogram (ventricular fibrillation, pulseless ventricular tachycardia, pulseless electrical activity, and asystole), place of cardiac arrest, witness status, bystander defibrillation, dispatcher assistance CPR, response time interval, scene time interval, transport time interval, EMS defibrillation attempt, mechanical CPR device, prehospital drugs (epinephrine, amiodarone), level of ED, past medical history, targeted temperature management, reperfusion therapy, and extracorporeal membrane oxygenation.
The primary outcome was the prehospital ROSC rate. The secondary outcomes were survival to discharge and a favorable neurological outcome. Neurological outcome was evaluated according to the cerebral performance categories (CPC) scale of 1 to 5: 1, good cerebral performance (conscious, alert, able to work, and lead a normal life); 2, moderate cerebral disability (conscious and sufficient cerebral function for independent activities of daily life); 3, severe cerebral disability (conscious, dependent on others for daily support); 4, coma or vegetative state; and 5, brain death [18]. CPC 1 and 2 were classified as favorable neurological outcomes and CPC 3, 4, and 5 were categorized as unfavorable outcomes.
Statistical analysis
Categorical variables were analyzed using the chi-square test and continuous variables were analyzed using the Wilcoxon rank-sum test. Continuous variables are presented as median and 25% to 75% interquartile range. The temporal trends by study period interval on the method of airway management and tier type were evaluated by the Cochran-Armitage test.
The unadjusted odds ratio (OR) with 95% confidence interval (CI) were calculated to show the unadjusted association between airway management/tier type and OHCA outcomes. The adjusted OR (aOR) with 95% CI were calculated via multivariable logistic regression analysis to assess the effects of airway management, tier type, and potential confounders such as age, sex, residential area, location of arrest, initial electrocardiogram, place of cardiac arrest, witness status, bystander CPR, bystander defibrillation, dispatcher assistance CPR, response time interval, scene time interval, transport time interval, EMS defibrillation attempt, mechanical CPR device, prehospital epinephrine, level of ED, and past medical history. The aOR with 95% CI were also calculated via multivariable logistic regression analysis to assess the interactive effects of airway management method and tier type. Statistical significance was defined as a P-value less than 0.05. All statistical analyses were performed using the SAS ver. 9.4 (SAS Institute Inc., Cary, NC, USA).
RESULTS
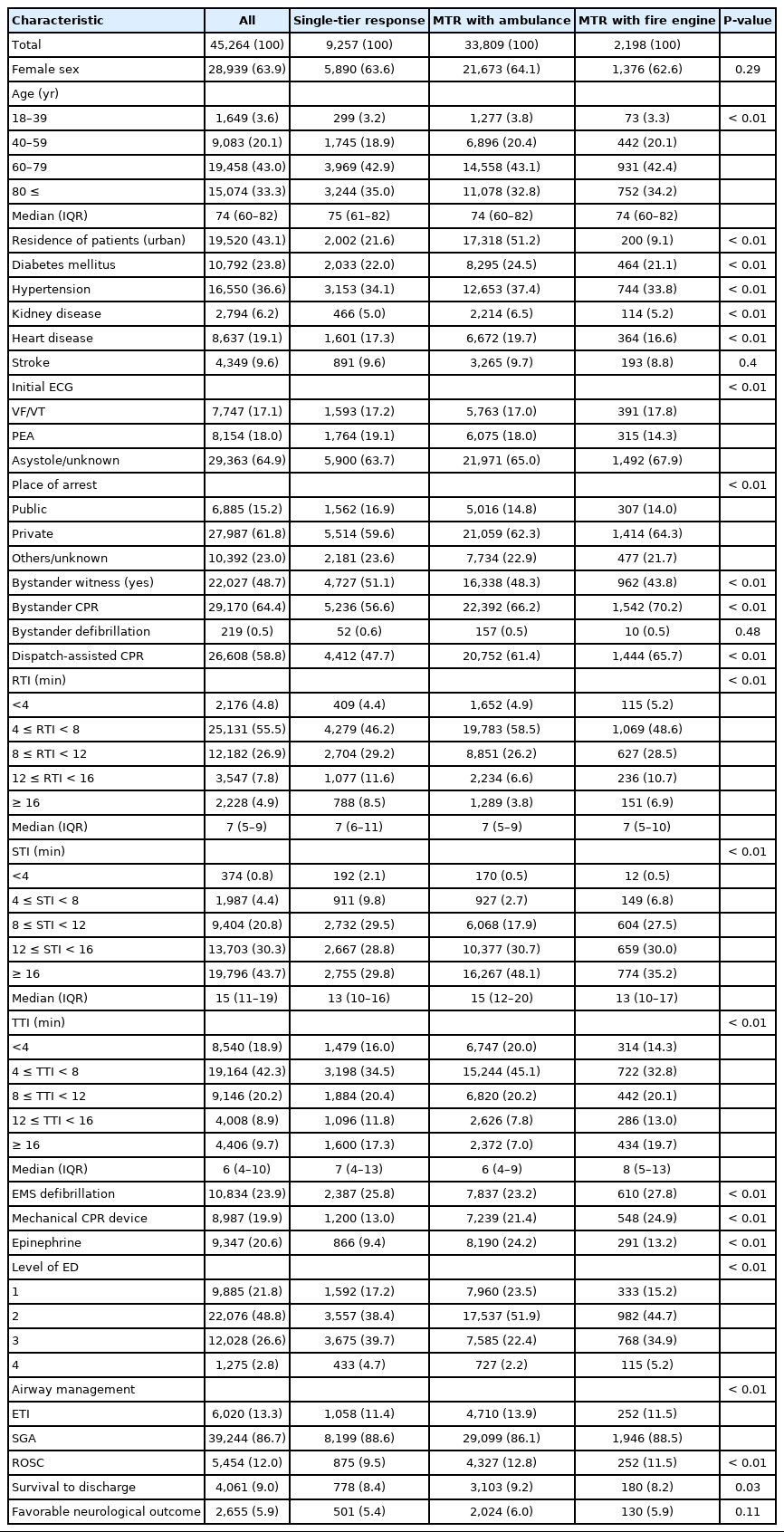
Among the 89,087 EMS-assessed OHCAs during the study period, 45,264 patients were analyzed (Fig. 2). The characteristics of OHCA patients by airway management and tier response type are shown in Tables 1 and 2. Of the airway management methods performed, SGA was more preferred than ETI (86.7% vs. 13.3%, P<0.01). In tier type, MTR with an ambulance was more prevalent than the STR (74.7% vs. 20.5%, P<0.01) or MTR with a fire engine (74.7% vs. 4.9%, P<0.01).
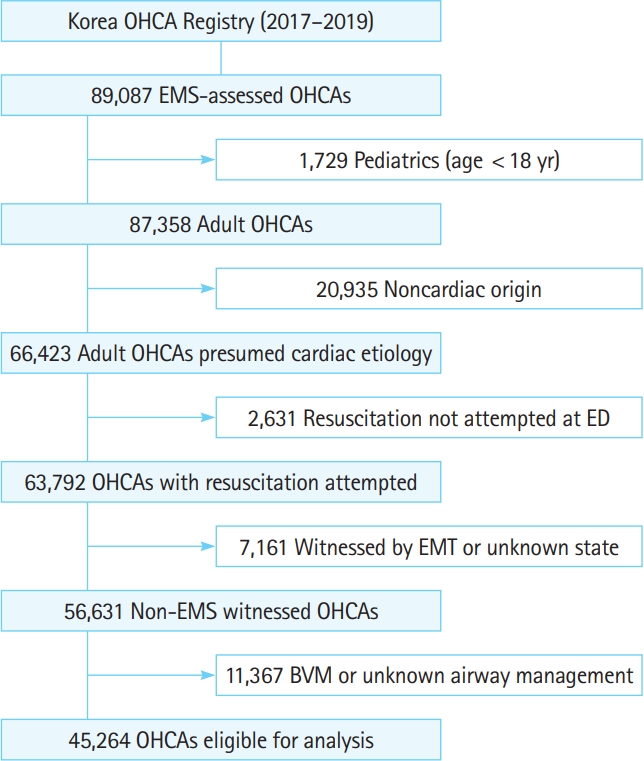
Study flow chart. OHCA, out-of-hospital cardiac arrest; EMS, emergency medical service; ED, emergency department; EMT, emergency medical technician; BVM, bag-valve mask.
Fig. 3 shows trends in the crude incidence rate of airway management method and tier type by year. From 2017 to 2019, MTR with an ambulance was significantly increased from 70.1% to 79.1% (Ptrend<0.01) and prehospital SGA was also significantly increased from 84.7% to 88.4% (Ptrend<0.01) whereas there was a significant decrease in the trend of the STR, MTR with a fire engine, and prehospital ETI (Ptrend<0.01).

Trends in the tier response type and airway management of out-of-cardiac arrest. MTR, multi-tier response; ETI, endotracheal intubation; SGA, supraglottic airway.
Results of multivariable logistic regression models for outcome by airway management method are shown in Table 3. In the case of adjusted analysis, the SGA group was significantly associated with a lower prehospital ROSC rate compared to the ETI group (aOR, 0.79; 95% CI, 0.72–0.88). Table 4 shows multivariable logistic regression analysis of tier response type and each outcome. Both MTR with an ambulance or with a fire engine were significantly associated with higher prehospital ROSC compared to the STR (STR vs. MTR with an ambulance: aOR, 1.33; 95% CI, 1.21–1.47; STR vs. MTR with a fire engine: aOR, 1.43; 95% CI, 1.20–1.71).

Multivariable logistic regression analysis for out-of-hospital cardiac arrest outcomes by airway management method
Table 5 shows interaction analysis of tier type response and airway management method on clinical outcomes. Regardless of tier type response, SGA was significantly associated with lower prehospital ROSC than ETI. In the case of MTR with a fire engine, patients who received SGA showed significantly lower favorable neurological outcomes than ETI (aOR, 0.71; 95% CI, 0.53–0.96).
DISCUSSION
In this nationwide population-based observational study, we observed that MTR was associated with higher prehospital ROSC than a STR. Prehospital SGA was associated with a lower prehospital ROSC rate compared to prehospital ETI regardless of the tier response type. In the case of MTR with a fire engine, prehospital ETI was significantly associated with a favorable neurological outcome.
During field resuscitation, an inadequate number of providers may cause low-quality CPR because simultaneous tasks including defibrillation, oxygen supply, airway management, and intravascular access should be provided. It is not easy to manage all tasks on the field with two or three EMT members. MTR is one of the most common methods of providing more manpower for field resuscitation [19-21]. In this study, we showed that the MTR could provide enough manpower to achieve a higher prehospital ROSC rate.
The pros and cons of ETI have been proposed. ETI is a definitive airway management technique that precisely controls gas exchange and protects lungs from vomitus if competency to performance is guaranteed. However, because of its difficulty and complexity, it should be performed by an experienced EMT in cooperation with organized manpower [3,7-9]. ETI showed superiority to SGA in prehospital ROSC regardless of tier type in this study. In Korea, prehospital providers are classified into level-1 EMT (EMT-intermediate in the USA) and level-2 EMT (EMT-basic in the USA). Prehospital ETI or SGA is performed only by a level-1 EMT, and the selection of the advanced airway management method is dependent on the preference of the EMT. Table 2 shows that prehospital SGA is preferred more than prehospital ETI (86.7% vs.13.3%). In this sense, we expect that ETI was done mostly by skillful and experienced EMTs, which could have affected the results.
We hypothesized that MTR could provide enough manpower. However, the type of tier response provides a different level of service, which could result in different interactive effects with the type of airway management. In the case of MTR with a fire engine, prehospital ETI was associated with favorable neurological outcomes. Table 2 shows that the MTR with a fire engine was more prevalent in rural areas. In rural areas, EMS resources might be insufficient due to a lower population rate resulting in a lack of experience, shortage of eligible hospitals, and shortage of manpower. Due to the shortage of resources, MTR with the fire engine service provides the fire engine team as the first responder, who can only provide BLS. Paradoxically, the divided scope of work between the first responder and the ambulance service may have a positive effect on the prognosis. In rural areas, a team includes a skillful EMT, who can provide advanced cardiovascular life support. Therefore, support members capable of providing BLS might be appropriate in the aspect of resource allocation. The specific protocol of the MTR and the training of the EMT in advanced resuscitation techniques could beneficially affect the clinical outcomes of OHCA patients.
A previous study has shown that the prehospital ROSC rate was significantly associated with survival to discharge and favorable neurological outcomes [22]. In this study population, prehospital ROSC was also associated with survival to discharge (aOR, 27.03; 95% CI, 24.83–29.42) and favorable neurological outcomes (aOR, 59.41; 95% CI, 51.38–68.69). Prehospital ETI was significantly associated with prehospital ROSC. However, it was not associated with survival to discharge or favorable neurological outcomes. There may be two explanations for the study results. First, the prehospital ROSC rate was similar between the ETI and SGA groups (12.5% vs. 12.0%). However, variables related to prehospital outcomes were significantly different. The urban population was more prevalent in the ETI group (62.8% vs. 40.1%), whereas, prehospital epinephrine administration (25% vs. 20%) and mechanical CPR device (40.4% vs. 16.7%) were higher in the ETI group, which could have affected the prehospital ROSC rate more positively. Mechanical device application during ambulance transportation was recommended to provide high-quality CPR [23,24]. Moreover, there was a significant imbalance in the number of included patients between the ETI and SGA groups. We were unable to adjust the confounding conditions completely. Second, failed ETI attempts were reverted to SGA or BVM and these were profound confounding factors. We could not adjust these confounding factors due to the retrospective study design. Further studies using more appropriate statistical analysis to adjust for confounders such as propensity score matching analysis or prospective randomized control study designs are needed to verify prehospital airway management and OHCA outcomes.
This study has several limitations. First, the KOHCAR database was not planned for collecting information on airway management resulting in the lack of details on airway management such as the initial selection of the airway method, number, and duration of initial advanced airway attempts. In addition, there was a lack of information on whether advanced airway management was performed during CPR or after ROSC. We could not adjust the attempts of advanced airway trials. In the Korean EMS system, all EMTs must follow government regulations. The regulation states that one attempt should be performed within a single 30-second duration and up to two attempts of advanced airway management can be made on the scene. Therefore, we could presume that only a small number of cases were reverted to SGA or BVM after prolonged and multiple attempts. Second, this study was conducted in a two-tier, dual dispatch EMS system that provides an intermediate service level, which is different from other countries. Noteworthy differences were also found in the OHCA patient characteristics between the Korea OHCA registry and previously studied registries such as the CARES (Cardiac Arrest Registry to Enhance Survival) registry, ROC (Resuscitation Outcomes Consortium) trial, or the AIRWAYS-2 trial. Field termination of resuscitation comprised a considerable percentage in other registries. However, EMTs in Korea are unable to terminate resuscitation and declare death unless there are signs of irreversible death; therefore, most OHCA cases in Korea are transported to the closest ED. These factors could have influenced study outcomes, limiting the generalizability of the findings in this study. Third, selection bias may exist despite performing multivariable adjustments for potential confounders. We could not exclude the possibility that the preference of ETI over SGA by skillful EMTs resulted in a better patient prognosis. Prehospital ETI is relatively new in Korea. Therefore, organized training and education of airway management are expected to have positive effects on OHCA outcomes. Fourth, there was no information on CPR quality, which is a profound prognostic factor. Korean EMTs, who passed the national level certification, receive annual medical education and clinical training to maintain knowledge and skill performance. Hence, CPR quality management might be well-controlled. Fifth, this was a retrospective registry-based study; thus, there might have been potential uncontrolled biases.
In conclusion, in this nationwide population-based observational study, we observed that MTR was associated with a higher prehospital ROSC rate compared to a STR. Prehospital SGA was associated with a lower prehospital ROSC rate compared to prehospital ETI, regardless of tier response type. Prehospital ETI was significantly associated with favorable neurological outcomes in MTR with a fire engine.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
FUNDING
None.
References
Article information Continued
Notes
Capsule Summary
What is already known
Optimal prehospital airway management during cardiopulmonary resuscitation is debating.
What is new in the current study
This study shows that multi-tier response provides higher prehospital return of spontaneous circulation (ROSC) than single-tier response. Additionally, supraglottic airway management is associated with a lower prehospital ROSC rate regardless of tier response type compared to endotracheal intubation for out-of-hospital cardiac arrest patients.