Comparison of emergency department workloads before and during the COVID-19 pandemic as assessed using relative value units
Article information
Abstract
Objective
This study aimed to assess and compare emergency department (ED) workloads by using relative value units (RVUs) before and during the COVID-19 pandemic.
Methods
This retrospective observational study investigated the RVUs of a single ED from 2019 to 2021. We calculated the mean number of patients per day (PPD) for each year and selected the days when the number of patients was equal to the yearly mean PPD for each of the three years. We calculated the total RVUs per day and RVUs per patient and compared them.
Results
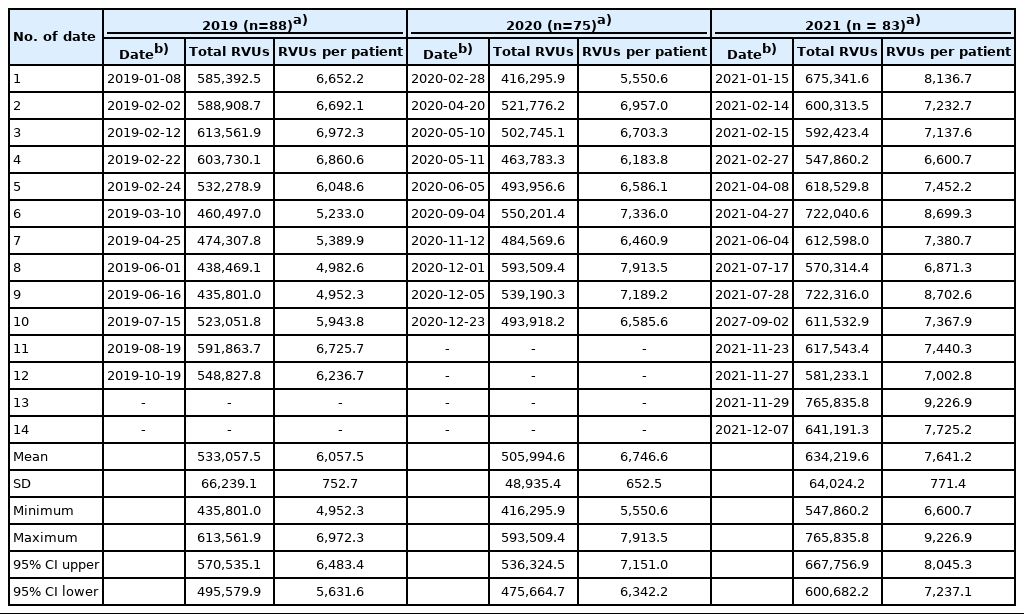
We analyzed the RVUs of 12 days in 2019 (mean PPD, 88), 10 days in 2020 (mean PPD, 75), and 14 days in 2021 (mean PPD, 83). The mean of the total RVUs per day were as follows: 533,057.5±66,239.1 in 2019, 505,994.6±48,935.4 in 2020, and 634,219.6±64,024.2 in 2021 (P<0.001). The RVUs per patient in the three year-groups were significantly different (6,057.5± 752.7 in 2019, 6,746.6±652.5 in 2020, and 7,641.2±771.4 in 2021; P<0.001). Post hoc analyses indicated that the total RVUs per day and the RVUs per patient in 2021 were significantly higher than in 2019 or 2020, although the mean PPD in 2019 was the highest.
Conclusion
Since the onset of the COVID-19 pandemic, the mean RVUs per patient have increased, suggesting that the workload per patient may also have increased in the regional emergency medical center.
INTRODUCTION
It is essential to accurately assess the workload of emergency departments (EDs). Measuring the workload properly can facilitate appropriate resource allocation to provide quality emergency medical care. However, the ED is an environment where many patients with various medical complaints and needs are seen every day. The workload varies depending on the patient [1,2]. Thus, the actual workload performed by an emergency physician (EP) may not match the number of patients they see.
Several studies have been conducted to measure the workload of EDs. A study conducted in Australia attempted to measure ED workload using newly developed emergency care workload units composed of measurements of patient capacity, disposition, numbers of patients, and the individual cost of each presentation [3]. In a British study, there was an attempt to directly observe and record EP activities of each moment (e.g., history taking, physical examination, clinical skills, etc.) to estimate the amount of EP time required [4]. However, each of the existing models of ED workloads has significant limitations [5].
In other hospital areas or functions, attempts have been made to measure workload using relative value units (RVUs) [6]. In brief, RVUs are a measure of value used in the typical formula to calculate compensation for physician services, which vary from country to country. An RVU is designed to value physicians’ service and serve as a guide for reimbursement, and can be applied to assess the productivity, cost, and benchmarking of medical services [7]. The advantage of using RVUs to measure workload is that it is possible to directly assign a numerical value to the procedures performed on the patients. For example, the RVU for central venous catheterization in Korea is 1,124.7, and the value is identical in all hospitals. However, in the compensation claim, this value is multiplied by a predetermined ratio that varies according to the level of hospital (third hospital vs. private clinic), the situation (day vs. night), and the patients treated (adult vs. pediatrics). We postulated that there have been changes in the workload performed per patient visiting the ED after the onset of the COVID-19 pandemic. However, to date, no studies have used RVUs to assess and report the workload of EDs in Korea. Therefore, this study aimed to use RVUs to evaluate and compare the identify workload of an ED in an academic hospital. Specifically, the purpose of this study was to calculate the difference between RVUs per patient and compare the total RVUs per day before and during the COVID-19 period for days on which the mean number of patients visiting the ED was equal to annual mean number of patients seen per day.
METHODS
Ethics statement
The study was approved by the Institutional Review Board of Dong-A University Hospital (No. DAUHIRB-EXP-22-03). Informed consent was waived due to the anonymous nature of the data.
Study design and setting
This retrospective observational study investigated and compared the RVUs in a single ED from 2019 to 2021. We calculated the mean number of patients per day (PPD) for each year and selected the days when the number of patients was equal to the yearly mean PPD for each of the three years. We calculated the total RVUs and RVUs per patient on those days and compared them (Fig. 1). We postulated that the ED would experience average working patterns on the selected days when an average number of patients visited the ED.

Flow chart of the study design. PPD, patients per day; RVU, relative value unit; SD, standard deviation.
This research was performed at an urban academic medical center with an 830-bed hospital. There were six members of the teaching staff and four emergency medicine residents. In 2017, this ED was designated as a regional emergency medical center. Approximately 32,000 patients visit the ED annually. The 3-year average percentage of cases that scored 3 or higher on the Korean triage and acuity scale (KTAS) was approximately 59.3%. The hospitalization rates in the ward and intensive care unit were about 35.5% and 9.5%, respectively.
Study outcomes
The primary objective was to compare the difference between the RVUs per patient in the year prior to and during the first two years of the COVID-19 pandemic on days when the mean number of PPD was equal to the annualized mean for each of the three years. The secondary objective was to compare total RVUs on days with the same mean number of PPD for each year.
Data source and collection
The RVUs are calculated automatically by the program when a physician inserts a prescription into the electronic medical record program. The data were collected through the hospital insurance department and subsequently downloaded to Microsoft Excel (Microsoft Corp., Redmond, WA, USA).
Statistical analysis
Descriptive statistics for the RVU data for those days with the same PPD as the mean PPD per year were compiled, including the mean, standard deviation, maximum, and minimum. The comparison of the daily RVUs per patient each year was conducted using a one-way analysis of variance. Post hoc analyses were conducted using the Tukey test. All the tests were two-tailed, and P-values less than 0.05 were considered statistically significant. All statistical analyses were performed using Microsoft Excel and R ver. 4.1.2 (R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
Comparison of total RVUs for the selected days when the number of patients seen was equal to the annualized mean number of PPD
During the study period, the mean PPD was 88 in 2019, 75 in 2020, and 83 in 2021. There were 12 days in 2019 when 88 patients visited the ED, 10 days in 2020 when 75 patients visited, and 14 days in 2021 when 83 patients visited. The mean PPD in three year-groups was significantly different (P<0.001). Post hoc analysis was for 2019 and 2020 (P<0.001), 2020 and 2021 (P=0.026), and 2019 and 2021 (P=0.116). The mean of the total RVUs for the selected days with the same PPD as the yearly mean PPD were as follows: 533,057.5±66,239.1 in 2019, 505,994.6±48,935.4 in 2020, and 634,219.6±64,024.2 in 2021 (Table 1). The means of the total RVUs in the three year-groups were significantly different (P<0.001). Post hoc analyses for 2019 and 2020 (P=0.034), 2019 and 2021 (P<0.001), and 2020 and 2021 (P=0.007) were significantly different. The mean PPD was higher in 2019 than in 2021 (88 PPD vs. 83 PPD, P=0.116), but the mean total RVUs was higher in 2021 than in 2019 (P<0.001).
Comparison of RVUs per patient on the days with the same mean number of PPD
The daily RVUs per patient are presented in Table 1 and Figs. 2 and 3. Since the onset of the COVID-19 pandemic, the RVUs per patient has increased. The RVUs per patient in the three year-groups were significantly different (6,057.5±752.7 in 2019, 6,746.6±652.5 in 2020, and 7,641.2±771.4 in 2021; P<0.001). Post hoc analyses of the RVUs for 2019 and 2021 (P<0.001) and 2020 and 2021 (P<0.001) were significantly different, but the RVUs for 2019 and 2020 (P=0.560) were not significantly different.
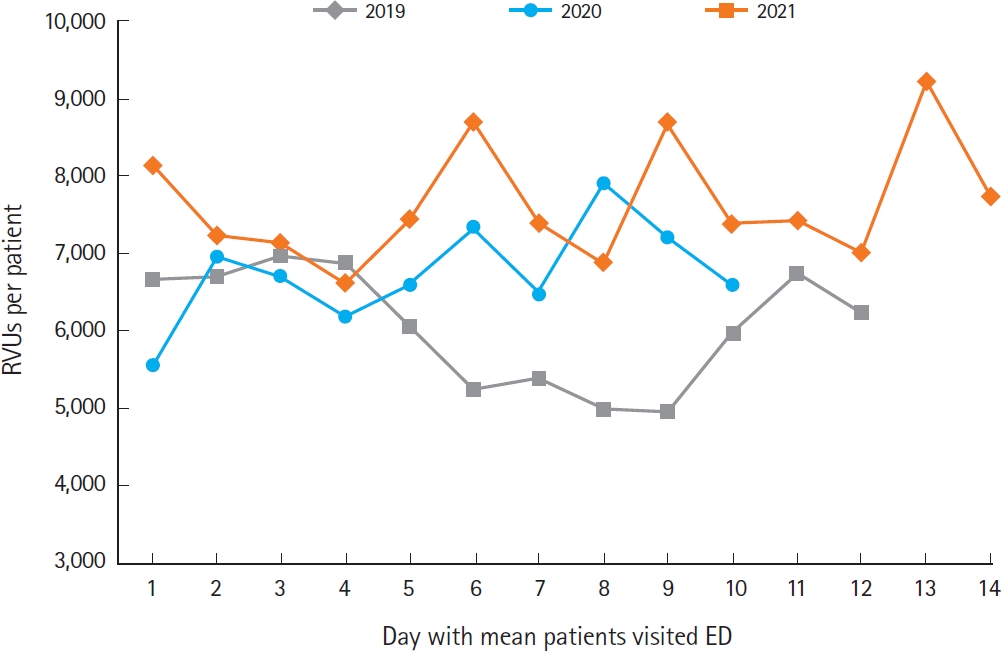
Comparison of relative value units (RVUs) per patient on days with the same number of patients as the mean patients per day for each year. The X-axis indicates the day when the mean number of patients per year visited the emergency department (ED), and the Y-axis indicates the RVUs per patient for that day.
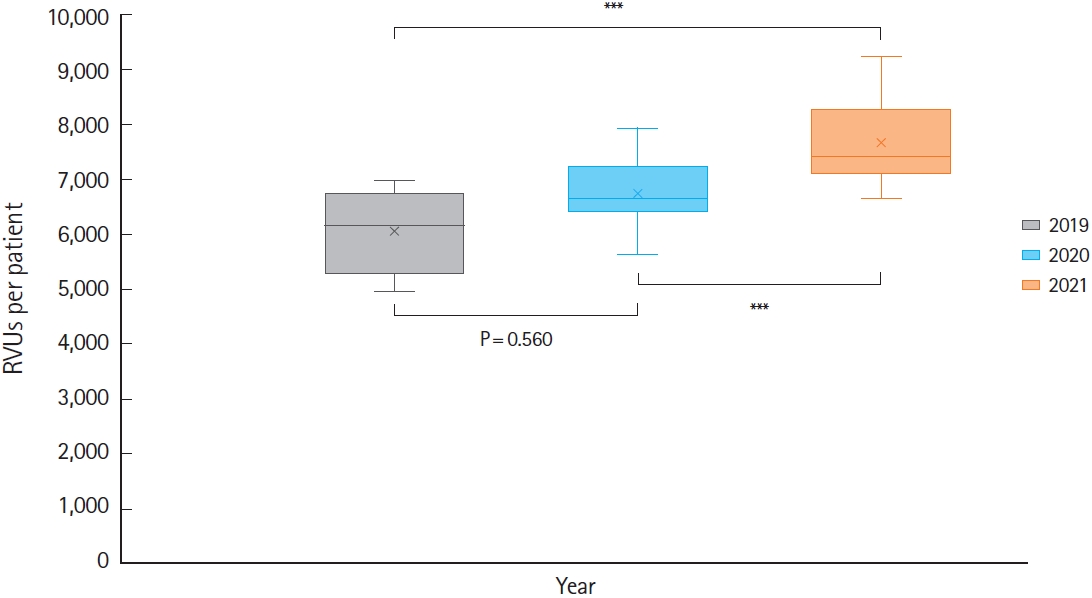
Comparison of relative value units (RVUs) per patient on days with the same number of patients as the mean patients per day for each year with boxplots. The boxplot shows the maximum, third quartile, median, first quartile, and minimum from the upper line to the lower line, and the X mark indicates the mean. ***P<0.001.
DISCUSSION
The goals of this study were to estimate the total workload using RVUs and examine changes in the RVUs per patient since the COVID-19 pandemic began. The mean PPD was higher in 2019 than in 2021 (88 PPD vs. 83 PPD), but the mean total RVUs was higher in 2021 than in 2019. The RVUs per patient have been steadily increasing during the COVID-19 pandemic.
There has been some controversy regarding the use of RVUs in the measurement of physician performance or workloads. The use of RVUs was initially designed to provide relative economic values of healthcare services based on the cost of delivering services, including costs attributed to physician’s work, medical expenses, and professional liability [8]. It should be noted that RVUs were not originally intended to function as the primary measure of a physician’s performance. Thus, assessing physician performance by RVUs monetizes the patient-physician relationship and incentivizes more, although not necessarily better, care [9]. The use of RVUs also indirectly discourages clinicians from focusing on essential behaviors to improve outcomes and reduce costs [10]. In addition, RVU assignments correlate poorly with specific metrics of surgical work [11]. High productivity does not always reflect the intensity of work. Nevertheless, the practice of using RVUs to measure workload or productivity is widespread, as RVUs are used globally as a standardized metric to describe medical services [12]. If RVUs are used as a tool of reward to physicians, physicians may prefer skills or treatment with high RVUs. However, emergency care in the ED is not performed for compensation, and EPs in Korea are also not compensated based on the RVUs. Thus, it is thought that there will be no exaggeration in estimating the workloads with RVUs.
Few studies in Korea have used RVUs to estimate workload or productivity. Most studies have investigated whether the RVU of a specific procedure or surgery is adequately valued or reimbursed. One study that analyzed changes in spinal surgery and intervention reported that RVUs for more complex spinal and brain neurosurgery procedures increased by 125.3% and 133%, respectively, during the same period [13]. Another study examined associated physician fees and used RVUs to compare the mean proportion of the total medical cost represented by physician labor costs: the resulting value of 0.19 was significantly lower than that for corresponding procedures in the United States based on RVUs (mean, 0.48) [14]. One reason RVUs have not been used to estimate workload or productivity in Korea may be because this system is not directly linked to physician wages.
Studies comparing workload using RVUs are relatively common in the United States. This is because RVUs were developed to reimburse physicians based on their workload. A study in the United States reported that an approximately 60% reduction in workloads in the radiology department after COVID-19 was reported when using RVUs, and this information was used for staff redeployment [15]. Another study described the financial impact of COVID-19 on an academic neurosurgery department using daily RVUs and found that the mean reduction was 51.4% compared with the pre-COVID period [16]. However, we could not find any studies from Korea that reported changes in RVUs before and after the onset of the COVID-19 pandemic.
In our study, the mean PPD in the ED decreased after the COVID-19 pandemic began, but RVUs per patient increased. These findings are consistent with a study by Pines et al. [17], wherein the authors found that following the onset of the COVID-19 pandemic, geriatric, adult, and pediatric visits declined by 43%, 40%, and 73%, respectively, compared to 2019. However, RVUs per visit rose by 8%, 9%, and 18%, respectively. This finding may be partly attributed to the use of additional diagnostic procedures, such as chest computed tomography or COVID-19 polymerase chain reaction (PCR) tests, to screen patients for COVID-19. The COVID-19 PCR test in Korea is assigned 1,630.6 RVUs. It can be estimated that 24% of RVUs per patient in 2020 and 21% of RVUs per patient in 2021 were associated with COVID-19-related work in this study. Alternatively, the influence of COVID-19 on RVUs may be due to an increased proportion of more severely or acutely ill patients presenting to the regional emergency medical center requiring more complex procedures [18]. In the ED where this study was conducted, the proportion of emergency patients with KTAS scale of 3 or higher increased from 57.7% in 2019, to 58.3% in 2020, and 61.8% in 2021 during the study period, although it should be noted that the KTAS does not directly reflect the patient’s severity or resource requirements.
The current standard staffing requirement for EDs in Korea is based on the number of patients visiting the ED per year. According to the criteria governing regional emergency medical centers, the rules for assigning EPs state that if the number of patients in the ED exceeds 30,000 in the previous year, a medical center will be added, and one additional EP per 10,000 patients will be secured [19]. The findings of our study confirm that when assigning ED staff, the number of patients may not sufficiently reflect the actual workload of the ED. The standards for staffing need to reflect the actual workload, and not only the number of patients, and in particular, need to consider the increase in the RVUs per patient due to COVID-19. We found the RVU reflects the ED workload better than patient numbers, but it is not sufficient. It is necessary to develop a new ED workload measurement tool, such as the emergency care workload units developed in Australia [3].
We acknowledge that there are several limitations to our study. First, this study analyzed data from a single ED. Further analyses of data from several EDs with varying patient volume and context should be conducted. In the case of regional emergency medical institutions, where the number of patients visiting the ED decreased and the proportion of severely ill patients also decreased during the COVID-19 pandemic, the RVUs per patient would have been reduced as well. However, caution should be taken in using these results as a criterion for staff reduction. This is because emergency medical services serve as social safety nets. Second, features of medical services that could not be measured by RVUs, such as multitasking in the ED—treating multiple patients simultaneously—were not assessed in this study. Third, the RVUs of each procedure performed in the ED were not evaluated in depth. We did not evaluate whether the difference in RVUs between a surgeon suturing a patient’s wound during the day and an EP suturing at midnight was appropriate. Productivity as evaluated by RVUs can change depending on the physician and patient, even for patients with similar complaints. In addition, if a specialist and a resident work together, it is not always easy to attribute the result to one or the other. Fourth, this study focused on the workload of an ED, and not on the workload of individual EPs; in a study by Park et al. [20] that evaluated the nonclinical work of EPs who worked in a training hospital, administrative and educational work was found to be a considerable burden over and above clinical work. Further research is required on this topic.
In conclusion, we provided an estimate of ED workload based on the number of patients treated. However, this study showed that there was a gap between the actual workload in the ED and the number of patients. Moreover, since the COVID-19 pandemic began, the mean RVUs per patient has increased, suggesting that the workload per patient may also increase in a regional emergency medical center. Estimating the ED workload is the basis for calculating staffing requirement and preparing adequate resources. When staff are assigned appropriately, safe and quality emergency medical services can be provided. It is time to consider measuring ED workload based on the actual amount of work performed and not only on the number of patients visiting the ED.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
FUNDING
This work was supported by a Dong-A University Research Fund (No. 20220124).
References
Article information Continued
Notes
Capsule Summary
What is already known
It is essential to accurately assess the workload of emergency departments (EDs). Measuring the workload can facilitate appropriate resource allocation to provide quality emergency medical care. There were studies to measure workload using relative value units (RVUs) in other non-ED areas of hospitals outside of Korea.
What is new in the current study
This study showed that since the COVID-19 pandemic, the mean RVU per patient has increased, suggesting that the workload per patient may also have increased in the regional emergency medical center. Moreover, there were considerable differences between the actual workload that estimated using RVUs and the number of patients in the ED.