The 2022 monkeypox outbreak in nonendemic countries: a review for the emergency department clinician
Article information
Abstract
Since May 2022, monkeypox (MPX) cases have been reported from several European countries, and this outbreak rapidly spread globally. Although MPX is not a new disease, most clinicians in nonendemic countries are unfamiliar with it. In addition, this current outbreak, unlike previous outbreaks in Africa, shows unique features in terms of epidemiology, transmission routes, and clinical manifestation. Most cases were men who have sex with men, had no travel history to an MPX endemic area, and presented with anogenital lesions, suggesting human-to-human transmission via close contact during sexual activity. In the emergency department setting, rapid identification of suspected cases and implementation of effective infection control and preventive measures are critical for preventing further transmission to healthcare workers and other patients. Emergency department clinicians should be aware of the clinical presentations of MPX and be alert to patients presenting with fever and vesicular rash or sexually transmitted disease-associated rash, especially among those with travel history to countries reporting an MPX outbreak. This brief review provides current information of MPX to help emergency department clinicians understand the epidemiology, transmission, clinical manifestation, diagnosis, treatment, and infection prevention and control of MPX.
INTRODUCTION
Monkeypox (MPX) is a zoonotic viral disease caused by the Monkeypox virus (MPXV). Since the first human case of MPX from the Democratic Republic of Congo in 1970, most human cases have been reported in West and Central Africa [1]. Outside of Africa, MPX caused an outbreak in 2003 in the United States, linked to importation of infected rodents from Ghana, and a few sporadic travel-related cases in the United States, United Kingdom, Israel, and Singapore [2]. In May 2022, several European countries and the United States reported atypical cases of MPX, which rapidly spread globally. Most cases were men who have sex with men without any documented history of travel to an MPX endemic area. Between January 1 and August 22, 2022, there were 41,664 confirmed cases of MPX, and 12 deaths reported from 96 countries, with approximately 99% of cases reported outside of Africa [3]. This unprecedented outbreak shows different features in terms of epidemiology and clinical manifestations compared to previous reported MPX in endemic areas [3-6].
Emergency department clinicians should be aware of the current epidemiology and clinical symptoms and signs of MPX for rapid identification of suspected cases. This brief review aims to provide current information on MPX to help emergency department clinicians understand the epidemiology, transmission, clinical manifestations, diagnosis, treatment, and infection prevention and control of MPX. An overview of MPX is presented in Table 1.
EPIDEMIOLOGY OF THE 2022 MPX OUTBREAK
A World Health Organization report published August 24, 2022 shows an overwhelming predominance of affected men (98.2%) with a median age of 36 years (interquartile range, 30–43 years). Among cases with known data on sexual orientation, 95.8% were identified as men who have sex with men. A sexual encounter was the most common type of transmission (82.1%), and the majority of cases (60.6%) were likely exposed in a party setting via sexual contact. Of those cases with known HIV status, 45% were HIV positive. Although a small proportion of cases has been reported among health workers (n=256), most were infected in the community [3]. To date, all cases identified in nonendemic countries whose samples were confirmed by polymerase chain reaction have been identified as being infected with the West African clade [3], which is often associated with milder disease than the Congo basin clade [7]. Some outbreak clade mutations have been identified in proteins involved in virus transmission and virulence [8].
TRANSMISSION AND VIRAL SHEDDING
Before the current outbreak, virus transmission through direct or indirect contact with live or dead animals was assumed to be the main factor for human MPX infections. Human-to-human transmission occurs primarily through direct contact with infected lesions or body fluids, respiratory droplets during close and prolonged face-to-face contact, or contact with contaminated objects such as clothing or linens [7]. However, in the 2017–2018 MPX outbreak in Nigeria, several unique findings were identified compared to previous MPX outbreaks in the African region [9,10]. Most of the infected cases were young men without exposure to infected animals and presented with genital ulcers, similar to cases in the current outbreak in nonendemic countries. In a study published in 2019, Nigerian researchers suggested the possibility of sexual transmission, but this hypothesis has not received considerable attention [10]. In the 2022 outbreaks, human-to-human transmission is occurring at an unprecedented and large scale, and the primary mode of transmission is direct and prolonged skin-to-skin contact during sexual activity [3,4]. In a large case study series, MPXV DNA was found in the semen of 29 of 32 people [4]. Another study reported frequent MPXV DNA in clinical samples including saliva, semen, rectal swab, urine, and feces from infected patients [11]. However, the infectious potential of these bodily fluids and their potential role in disease transmission are uncertain. In the pandemic of COVID-19, there are growing concerns about MPX potentially being transmitted through aerosols. A previous study of an MPX case in the UK healthcare workers (HCWs) in 2018 suggested that MPX can become aerosolized, particularly during certain activities like changing contaminated bedding [12]. However, in existing epidemiological investigations, no cases of long-range airborne transmission have been reported. A person is considered infectious from symptom onset until all skin lesions have crusted, those crusts have separated, and a fresh layer of healthy skin has formed underneath [7]. Although a recent study in France has suggested that asymptomatic MPX spread is contributing to the global outbreak, the infectiousness of asymptomatic individuals is uncertain [13].
CLINICAL PRESENTATION OF MPX IN THE CURRENT OUTBREAK
The incubation period ranges from 5 to 21 days but is typically 6 to 13 days following exposure [1,7]. Historically, patients with MPX have typically presented with prodromal symptoms, including fever, headaches, chills, malaise, and lymphadenopathy, followed by development of a macular rash starting from the face and spreading across the entire body [1,7]. Involvement of the genital area was reported in an old study in less than 30% of affected patients [14]. The skin lesion of MPX usually progresses through macules, papules, vesicles, pustules, and scabs. Unlike chickenpox, the lesions typically present at the same stage. The number of skin lesions exceeds 100 in 49% to 66% of patients, with more than 1,000 lesions in 17.5% of cases [14,15]. Complications in endemic countries include encephalitis, secondary skin bacterial infections, dehydration, conjunctivitis, keratitis, and pneumonia [1,7].
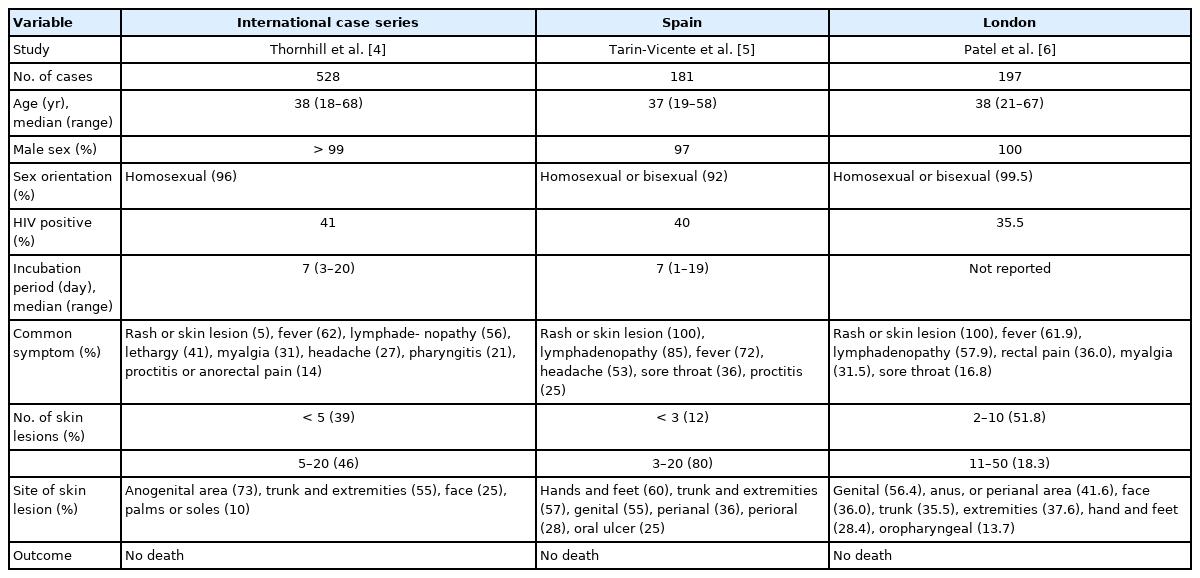
In the current 2022 outbreak, the majority of cases show atypical presentations, with rash in fewer regions of the body, in particular the genital and perianal areas, without spread to other body regions and with a relative mildness or absence of prodromal symptoms [3-6]. In the observational study of 528 MPX cases from 16 countries, 95% presented with a rash and 73% had anogenital lesions [4]. Most of the patients (64%) had 10 or fewer lesions, with 10% having a single genital lesion. Although there were no fatalities within the cohort, 13% were hospitalized for management of anorectal pain or bacterial superinfection. Additionally, two types of serious complications including epiglottitis and myocarditis were reported. The case fatality ratio of monkeypox has historically ranged from 1% to 11% in the general population and has been higher among young children [1,7]. In this outbreak, as of August 10, 2022, four deaths related to MPX have been reported outside the African region (two in Spain, one in Brazil, and one in India). In two cases, deaths have been linked to viral encephalitis, and some patients had underlying immune compromising conditions [16]. Table 2 summarizes data on the demographic and clinical characteristics of patients with MPX infection in the 2022 outbreak [4-6].
DIAGNOSIS AND TREATMENT OF MPX
It is important to be aware of the clinical presentations of MPX that have been described in the ongoing 2022 outbreak. When there is clinical suspicion for MPX, clinicians should ask about travel history and close contact with people with a similar rash or suspected or confirmed MPX infection. Particularly, clinicians should consider MPXV in differential diagnoses of sexually transmitted diseases presenting with genital lesions. Swabbing of a lesion exudate or crust specimen is considered the best sampling method to obtain a rapid and definite diagnosis of MPX. The nucleic acid of the virus could be also retrieved in blood, urine, upper respiratory tract excretions, and seminal fluid [17]. The treatment of MPX is primarily supportive with pain control, hydration, and management of complications. Antibiotics may be necessary in patients with a secondary bacterial skin infection, pneumonia, or conjunctivitis. There are no treatments specifically for MPXV infections. However, two antivirals, tecovirimat and brincidofovir, approved in the United States for treatment of smallpox, have been demonstrated to be effective against orthopoxviruses (including MPX) in animal models [18]. In Korea, tecovirimat is recommended for severe cases of MPX or immunocompromised persons. Additionally, cidofovir and vaccinia immune globulin may be considered for severe cases [18].
INFECTION PREVENTION AND CONTROL OF MPX IN HEALTHCARE SETTINGS
A combination of standard, contact, and droplet precautions should be applied in healthcare settings when caring for suspected or confirmed cases of MPX. Additionally, because of the theoretical risk of airborne transmission of MPXV, airborne precautions should be applied based on risk assessment. The patient should be required to wear a medical mask and placed in an isolated room with a dedicated toilet. No special air handling is required, but any procedures likely to spread oral secretions should be performed in an airborne infection isolation room. Skin lesions of the patients should be covered to the extent possible to minimize contact risk with others. Isolation precautions should be continued until all lesions have resolved and a fresh layer of skin has formed [19].
HCWs caring for confirmed or suspected MPX patients or handling specimens for diagnosis should use personal protective equipment, including gloves, gown, eye protection, and respirator. Dedicated footwear also can be used. For environmental infection control, standard cleaning and disinfection procedures are sufficient, but soiled laundry should be handled with gloves to avoid contact with lesion material and never be shaken or handled in a manner that may disperse infectious material [19].
The probability of exposure to MPXV for HCWs wearing appropriate personal protective equipment is considered to be very low. However, HCWs who have had an occupational exposure to an MPX case in the absence of appropriate personal protective equipment should undergo active surveillance for symptoms for 21 days. Postexposure vaccination is recommended for close contacts of cases, ideally within 4 days of first exposure (and up to 14 days in the absence of symptoms), to prevent onset or mitigate disease severity. Primary preventive (preexposure) vaccination is indicated for individuals and HCWs at high risk of exposure, clinical laboratory personnel performing diagnostic testing for MPX, and outbreak response team members (as designated by national public health authorities) [3]. Currently, the JYNNEOS vaccine, a third-generation vaccine approved for prevention of MPX by the US Food and Drug Administration, has been introduced and is available in Korea.
CONCLUSION
The 2022 MPX outbreak in nonendemic countries is a new threat during the ongoing COVID-19 pandemic. This outbreak presents unique epidemiological and clinical features from those of prior outbreaks. Emergency department clinicians should be aware of clinical manifestations, evaluation, and management of MPX. In addition, to prevent transmission in healthcare settings, clinicians should understand the basics of infection control for MPX.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
FUNDING
None.
References
Article information Continued
Notes
Capsule Summary
What is already known
Since the first human case of monkeypox (MPX) in 1970 in the Democratic Republic of Congo, sporadic outbreaks mainly in African regions and occasional cases and limited outbreaks linked to travel or importation of African animals have been reported. Since May 2022, numerous cases of MPX were reported from several nonendemic countries and this outbreak rapidly spread.
What is new in the current study
This brief review provides the current information of MPX to help emergency department clinicians understand the epidemiology, transmission, clinical manifestation, diagnosis, treatment, and infection prevention and control of MPX.