Efficiency, limitations, and familiarization of a novel negative pressure aerosol box for intubation: a simulation-based randomized crossover study
Article information
Abstract
Objective
This study aimed to introduce a novel negative pressure aerosol box (Carrycure Isolator) and to test its efficiency and limitations, with the hope of suggesting improvements and further directions.
Methods
A novel aerosol box (Carrycure Isolator) was invented. A single-center, randomized, crossover simulation study of 28 emergency medicine physicians was designed. Three trials of each participant using an intubation manikin were conducted, including intubation without the aerosol box (trial A), intubation with the aerosol box (trial B), and intubation with the aerosol box after familiarization (trial C). The primary endpoint was the time to intubation. The secondary endpoints were first-attempt success, number of attempts, percentage of glottic opening score, and Cormack-Lehane view. Collected data were statistically analyzed for their significance.
Results
The median times to intubation of trials A, B, and C were 30.5 (interquartile range [IQR], 28.0–40.0 seconds), 59.0 (IQR, 50.0–75.5 seconds), and 34.0 seconds (IQR, 30.5–47.0 seconds), respectively. Post hoc analysis showed that the time to intubation in trial B was significantly longer than that in trial A (P<0.05), while that the time to intubation in trial C was significantly shorter than that in trial B (P<0.05). Results concerning secondary endpoints showed similar patterns. Participants reported performing intubation with Carrycure Isolator to be relatively difficult, necessitating significant arm movement and view restrictions while increasing their time to intubation.
Conclusion
Physicians took a longer time to intubate a manikin using the Carrycure Isolator, a novel negative pressure aerosol box. However, the time was improved after a period of familiarization.
INTRODUCTION
The steep increase in confirmed COVID-19 cases with severe illness requiring hospitalization has led to a worldwide shortage of personal protective equipment and airborne infection isolation rooms [1]. To overcome the shortage of airborne infection isolation rooms, efforts have been made globally to develop isolation chambers or barriers known as “aerosol boxes” [2–10]. Despite their novelty, previous inventions have shown limitations. Some did not include a negative pressure device [3,5,6,10], others were simple barriers with open sides [10], and most did not have a slanted side, which can limit patient visualization [2,5,6,10]. Since severe COVID-19 cases often require aerosol-generating medical procedures (AGMPs), such as endotracheal intubation [11], having closed sides and maintaining negative pressure may mimic the effect of airborne infection isolation rooms and protect medical practitioners from pathogenic aerosols. Furthermore, a slanted viewing window enables the practitioner to approach the patient more closely and may provide a better view of the patient’s airway while performing AGMPs. Because of the limitations of previously introduced aerosol boxes, our team recently developed a novel negative pressure aerosol box called the Carrycure Isolator (Severance Hosptial) with closed sides, a negative pressure function, and a slanted viewing window. Our previous study of the Carrycure Isolator showed its efficacy in reducing contamination particles when performing intubation on a manikin [12]. However, its efficiency and usability have not yet been studied.
Despite the benefits of protecting medical practitioners from airborne illnesses, previous studies have shown that using an aerosol box limits the practitioner’s ability to perform AGMPs and thereby increases intubation time [13–18]. As an increased intubation time may prolong hypoxia and increase patient risk, studies have been cautious about applying these aerosol boxes in actual medical practice [5,13]. Because the Carrycure Isolator is a more advanced form of an aerosol box, it is prone to the same challenges. Hence, this study aimed to test the efficiency of the Carrycure Isolator through a simulation-based randomized crossover study. We hypothesized that, although intubation time may initially increase when using the Carrycure Isolator for the first time, it can be improved with multiple practice sessions and proper guidance.
METHODS
Ethical statements
This study was approved by the Institutional Review Board of Severance Hospital, Yonsei University Health System (No. 1-2021-0087).
Trial design, participant selection, and randomization
According to Begley et al. [13], the average time to intubation with and without the latest form of an aerosol box was 42.5 and 52.5 seconds, respectively, with a mean±standard deviation differential of 10.0±7.5. Using G*Power ver. 3.1 (Heinrich Heine University Düsseldorf) with a 95% confidence interval and alpha value of 0.025, the minimum sample size was 10. After measuring the time to intubation by the instructor and assuming that the possibility that the mean of the difference would be reduced to 5, the minimum sample size was 26. Hence, we chose a sample size of 28 and designed a single-center, randomized, crossover simulation study of emergency medicine physicians at Severance Hospital. This study was conducted between February 13, 2022 and February 20, 2022, at Severance Hospital. Physicians with >20 experiences of wearing personal protective equipment who were comfortable with endotracheal intubation with direct laryngoscopy were included, while those with physical disabilities or who were not willing to participate were excluded. A total of 30 emergency medicine physicians (both specialists and residents) who volunteered to participate in this study were deemed eligible, but two were excluded due to personal schedules. The remaining 28 participants completed consent forms and were block-randomized using a random number generator and allocated into either group A or B. All participants were instructed to perform three intubations on a manikin to simulate AGMPs. To minimize learning bias, group A participants started with the control trial without the Carrycure Isolator, whereas group B participants started with the experimental trial with the Carrycure Isolator. Moreover, all participants were blinded to their group assignment. After both control and experimental trials, all participants went through a familiarization period for 10 minutes, where they were instructed to practice freely with the Carrycure Isolator and the manikin. No specific set of instructions was given to each participant, although the experimenter provided each participant with a tip during that period: “When preparing endotracheal intubation, placing the endotracheal tube on the right side and the laryngoscope on the left side will prevent crossing over of your hands and may reduce intubation time.” After familiarization, each participant performed the third trial. All participants were instructed to complete a survey questionnaire after completing the trials (Fig. 1).
Invention of Carrycure Isolator
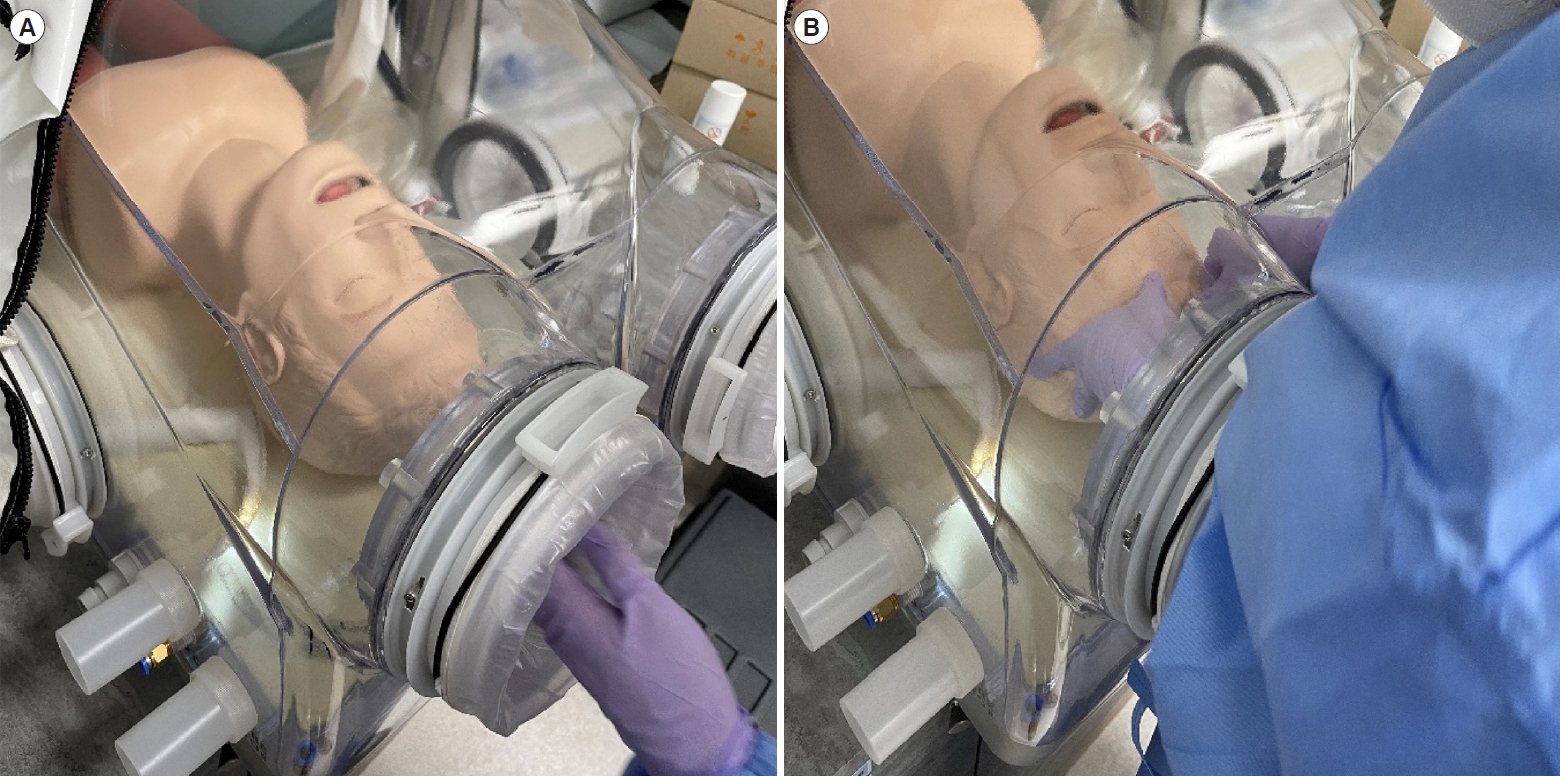
Our team recently invented the Carrycure Isolator, which is made of a 1-cm-thick acrylic material with five closed sides. It has a 44.3×44.3-cm base and a maximum height of 44.3 cm at the patient entrance side so that it can fit into a computed tomography scanner. There are two connecting ports on both lateral sides for a negative pressure generating device. Four patient access orifices are also located on three sides, each with an outer iris diaphragm and an inner silicone slit. The outer iris diaphragm can be completely closed when not in use. Two of these orifices are on the practitioner’s side, whereas the other two are placed on the right and left sides of the chamber, respectively. Previously invented “box-shaped” aerosol boxes are mostly cubic, which can prevent the practitioner from approaching the patient inside the box. Endotracheal intubation using a direct laryngoscope often requires approaching the patient to visualize their airway and vocal cords. The Carrycure Isolator has a slanted viewing window that enables the practitioner to freely approach the patient and easily visualize their airway [12].
Materials
One Carrycure Isolator, bag valve mask (Ambu SPUR II Adult, Ambu A/S), airway manikin (Laerdal Airway Management Trainer, Laerdal Medical), 7-mm endotracheal tube with a stylet, direct laryngoscope with Mac 4 blade, and 10-cc syringe were used for this study. The manikin was placed on a flat surface, and its height was adjusted by each participant to their most comfortable position to simulate the height-adjustable nature of the stretcher. Each participant was provided with new personal protective equipment (surgical gowns, nitrile gloves, masks, surgical caps, and protective goggles) for each trial (Fig. 2).
Endpoints and data collection
The primary endpoint of this study was time to intubation, which was defined as the time from the end of preoxygenation to the first ventilation after successful endotracheal intubation, as visualized by the inflation of both lungs on the manikin. Since Begley et al. [13] in their previous study used 180 seconds as a cutoff value for successful intubation in an aerosol box, when the participant required >180 seconds to intubate, the trial was considered a failure, and they were instructed to restart the procedure. Then, only the time to intubation during a successful trial was collected. The secondary endpoints were first-attempt success, number of attempts, percentage of glottic opening (POGO) score, and Cormack-Lehane view. A single attempt was defined as the single entrance of the direct laryngoscope into the oral cavity of the manikin. The time to intubation, first-attempt success, and number of attempts were measured and observed by the experimenter and recorded on the datasheet during the trial. The POGO score, Cormack-Lehane view, relative difficulty, relative arm restriction, relative viewing restriction, and subjective increase in intubation time were reported by each participant after the trial during a survey questionnaire, together with personal information such as age, sex, and length of experience in the emergency department. The POGO score was established on a 4-point scale as follows: 1 point, 0% to 25%; 2 points, 25% to 50%; 3 points, 50% to 75%; and 4 points, 75% to 100%. Relative measures were reported on a 5-point scale where 1 point represents “not at all” and 5 points represents “significantly increased.”
Statistical analysis
As our study considered three repeated trials for each participant, we performed a parametric analysis, assuming that the data from each trial were correlated. Freidman test and the Wilcoxon signedrank test were used for continuous and ordinal dependent variables, respectively, and the Cochran’s Q test and McNemar’s test were used for binary dependent variables. As a continuous variable, time to intubation was presented with median and interquartile range (IQR) values. All tests were two-sided, with a cutoff P-value of <0.05. A post hoc analysis was performed using the Bonferroni adjustment. Because three trials were performed, P<0.017 (0.05/3) was considered to be statistically significant. All statistical analyses were performed using SAS ver. 9.4 (SAS Institute Inc).
RESULTS
A total of 84 intubations were performed by 28 participants, all of whom were emergency medicine physicians. Although most participants (85.7%) were residents, all reported that they were confident in intubating using a direct laryngoscope. The mean age of the participants was 29.8 years, and their mean length of experience in the emergency department was 3.2 years. Other demographic information is presented in Table 1.
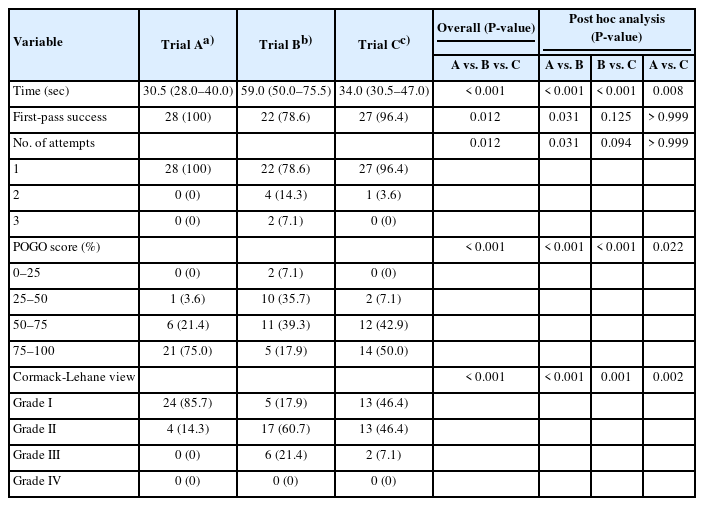
As a primary endpoint, the median times to intubation during the trials without the Carrycure Isolator (trial A), with the Carrycure Isolator (trial B), and with the Carrycure Isolator after familiarization (trial C) were 30.5 seconds (IQR, 28.0–40.0 seconds), 59.0 seconds (IQR, 50.0–75.5 seconds), and 34.0 seconds (IQR, 30.5–47.0 seconds), respectively (Fig. 3). The overall statistical analysis revealed that all three trials had significant differences in the time to intubation (P<0.001). Post hoc analysis showed that the time to intubation in trial B was significantly longer than that in trial A (P<0.017), while the time to intubation in trial C was significantly shorter than that in trial B (P<0.017). However, when comparing trials A and C, there was still a significant time increase, even after practice (P=0.008) (Table 2).
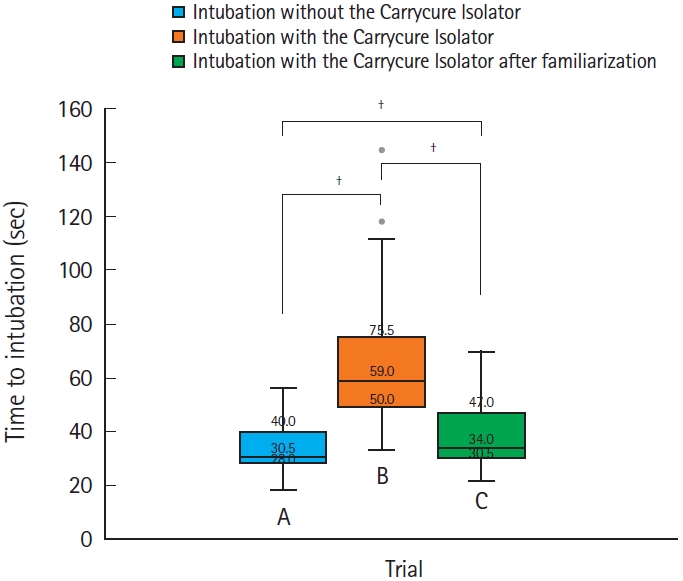
Box-and-whisker plot of the three trials. Interquartile range and median are noted on the diagram. †P<0.017.
As secondary endpoints, none of the participants failed to intubate during their first attempt in trial A, while six participants required >1 attempt in trial B and one participant required >1 attempt in trial C. There was a significant difference in first-pass success (P<0.050) and the number of attempts (P<0.050) when comparing all three trials. However, a post hoc analysis of first-pass success and number of attempts did not highlight a significant increase when comparing trials A and B (P=0.031 and P=0.031, respectively), A and C (P=0.125 and P=0.094, respectively), or B and C (P>0.999 and P>0.999, respectively). The self-reported POGO score and Cormack-Lehane view also were significantly different overall among the trials (P<0.017). A post hoc analysis showed that the POGO scores of trials A and C were significantly higher than that of trial B (P<0.017); in contrast, the POGO score difference between trials A and C was not significant (P=0.022), indicating that familiarization improved the view of the vocal cords. A post hoc analysis of the Cormack-Lehane view confirmed a similar pattern when comparing trials A and C with trial B, although the reported data of trial C suggested a significant decrease in the Cormack-Lehane view compared to those of trial A (Table 2).
The results from the adjunctive survey questionnaire about participants’ experience with the Carrycure Isolator are presented in Table 3. Participants felt that performing intubation using the Carrycure Isolator was relatively difficult (mean, 2.64 points), led to significant arm movement restrictions (mean, 4 points), required significant view restrictions (mean, 3.68 points), and significantly increased their time to intubation (mean, 3.89 points).
DISCUSSION
This study aimed to introduce a novel aerosol box, the Carrycure Isolator, and to test its efficiency. Price et al. [16], in their review article, categorized efficacy, usability, and efficiency as three important aspects to investigate when testing an aerosol box. Efficacy represents the ability to contain aerosol inside the box, usability refers to the user experience, and efficiency is indicated by the time to intubation [16]. Previous studies on negative pressure aerosol boxes or vacuum-assisted aerosol boxes have proven their efficacy by showing reduced particles during intubation of a manikin [19,20]. Our previous study with the Carrycure Isolator also proved its efficacy by showing a reduction of particles outside the Carrycure Isolator during simulated AGMPs performed on a manikin [12]. To test the Carrycure Isolator’s efficiency, we measured the time to intubation along with the other secondary outcomes mentioned above.
Our results showed that using the Carrycure Isolator significantly increased the time to intubation. This result was consistent with those of previous aerosol box studies conducted on a manikin [13,14]. In their systemic review and meta-analysis, Lim et al. [21] also reported that using an aerosol box in general significantly increased the time to intubation, but they mentioned that more experienced medical practitioners achieved a shorter time to intubation. However, previous studies have not focused on the effects of practice when testing aerosol boxes. Our results demonstrated that, after sufficient practice and guidance, the time to intubation was significantly decreased (59.0 seconds vs. 34.0 seconds, P<0.017), although it remained longer than that of the control group (30.5 seconds vs. 34.0 seconds, P=0.008). Owing to the slanted nature of the viewing window of the Carrycure Isolator, participants often experienced a collision of the connector side of the endotracheal tube with the viewing window, thereby interrupting tube advancement. In addition, because of the inevitable cramped nature of the aerosol box, participants had difficulty grasping materials on the opposite side of their hands. Some authors have presented a larger box or tent-like devices that may solve these difficulties [4,9,14]. However, the Carrycure Isolator was purposefully designed with specific dimensions so that the practitioner can approach the patient while performing intubation, and it can be used inside the computed tomography scanner while maintaining negative pressure. Most of the participants felt that the tip provided by the instructor during the familiarization period was useful and reported that, with sufficient practice, these inconveniences could be overcome. In addition, some participants felt that bending the connector portion of the endotracheal tube facilitated tube insertion and prevented a collision with the viewing window. Although this bending of the tube may benefit insertion attempts, it may also interrupt the removal of the stylet from the tube. Thus, further studies on more flexible and softer stylet materials should be conducted to improve both tube insertion and stylet removal.
First-pass success and fewer total attempts may be critical in patients requiring endotracheal intubation. Our data revealed significant differences among the three trials. When participants used the Carrycure Isolator for the first time, the first-time success rate was significantly decreased. However, even after sufficient practice, there was no significant difference. Meanwhile, although no significant increase in first-pass success was found when comparing trials B and C, we believe this result is due to the small sample size since all six participants who initially failed to achieve first-pass success succeeded after the familiarization period.
Although self-reported, the Cormack-Lehane view showed a similar pattern to that of time to intubation, where significant improvement was reported after familiarization. In addition to the effect of practice, we believe that the slanted viewing window also aids in vocal cord visualization. Further studies should be designed to test the effect of the slanted viewing window of the Carrycure Isolator by directly comparing it to a cubic aerosol box.
Participants’ completion of survey questions after the trials revealed negative reports on difficulty, movement restrictions, view restrictions, and perceived increased time to intubation. We believe that these results are due to the compact nature of the aerosol box. Further design modifications using malleable materials or variable sizes should be considered to overcome these difficulties.
Despite the novel nature and benefits of the Carrycure Isolator, our study has the following limitations. First, this was only a simulation-based manikin study. Since every individual patient has different airway structures, and patients often present with difficult airways, the results may differ when human subjects are used. Further studies on the efficiency of the Carrycure Isolator in patients or manikins with difficult airways should be considered. Second, because most of the participants were residents, a lack of experience may have caused an increase in intubation time. Although all participants reported that they were comfortable with endotracheal intubation using a direct laryngoscope, their mean age was 29.8 years and their mean experience in the emergency room was only 3.2 years. As endotracheal intubation is a critical procedure that often requires years of experience, our study may not reflect the entire physician population. Third, this study was performed using a direct laryngoscope. As videoscopy is becoming increasingly available worldwide, further studies with a videoscope should be conducted to improve the view of the vocal cords, although the size of this device may not be completely suitable for the Carrycure Isolator. Finally, since we conducted trial C right after the familiarization period, the long-term effects of practice should be examined in a future study.
Using an aerosol box challenges medical practitioners during AGMPs and increases their time to intubation. The same was true for our novel aerosol box, the Carrycure Isolator. However, our study showed that, after sufficient practice and proper guidance, the time to intubation is improvable on a manikin. Therefore, future attempts should be made to educate practitioners on the use of aerosol boxes, including how to apply them safely in actual medical practice.
Notes
CONFLICT OF INTEREST
Ideas in this study are included in a pending patent in Korea, and Severance Hospital (Seoul, Korea) signed a technology transfer contract with SJ Science (Seoul, Korea). If this technology is commercialized, the first and corresponding authors/inventors of this product might receive remuneration. However, the authors received no personal benefits from SJ Science.
FUNDING
This work was supported by a faculty research grant from Yonsei University College of Medicine (No. 6-2020 0121). The funder had no role in the study design, the collection, analysis, or interpretation of data, the writing of the report, or the decision to submit the article for publication.
AUTHOR CONTRIBUTIONS
Conceptualization: JYH, KSS; Data curation: YP, KSS; Formal analysis: YP, JHK; Funding acquisition: JYH, KSS; Visualization: JYH, YP; Writing–original draft: JYH, YP; Writing–review & editing: all authors. All authors read and approved the final manuscript.
References
Article information Continued
Notes
Capsule Summary
What is already known
Despite the benefits of protecting medical practitioners from airborne illnesses, previous studies have shown that using an aerosol box limits the practitioner’s ability to perform aerosol-generating medical procedures and thereby increases the intubation time. As an increased intubation time may prolong hypoxia and increase patient risk, studies have been cautious about applying these aerosol boxes in actual medical practice.
What is new in the current study
This study aimed to introduce a novel negative pressure aerosol box named Carrycure Isolator and test its efficiency and limitations in order to suggest improvements and further directions. We believe that our study makes a significant contribution to the literature because it highlights that using the Carrycure Isolator for intubation on a manikin led to results similar to those of previous studies involving aerosol boxes, where the time to intubation was initially significantly increased. However, the time to intubation is improvable after sufficient practice and familiarization.