Underlying mucus plugging during central line placement: a time-sensitive diagnostic dilemma
Article information
Dear Editor,
Superimposed clinical scenarios present diagnostic dilemmas that may delay care and ultimately increase morbidity and mortality. We report a case illustrating therapeutic ambiguity in the setting of central line placement with underlying mucus plugging of the right mainstem bronchus in a critically ill patient. The requirement for informed consent was waived due to the retrospective nature of the study.
In critically ill patients and postoperative patients with impaired cough reflex, an imbalance between mucus production and clearance occurs [1]. Despite diligent respiratory care, this imbalance may eventually lead to clinically significant mucus plugging, increasing morbidity and mortality [2]. When combined with invasive procedures such as central line placement, clinical management can become challenging, leading to diagnostic and therapeutic uncertainty.
A 62-year-old female patient with a history of combined liver-kidney transplant 19 years prior to admission presented with small bowel perforation. She underwent staged bowel resection and abdominal closure on day 1 and day 3, respectively, and was subsequently extubated. Postextubation, the patient had a normal chest X-ray. On hospital day 5, due to a lack of peripheral access and ongoing need for intravenous resuscitation, a central venous catheter was placed into the right internal jugular vein under ultrasound guidance without issue using the standard Seldinger technique. The patient was stable both hemodynamically and from a respiratory standpoint before, during, and after the procedure. However, on the postprocedure chest film, the right hemithorax was found to be opacified. This led to an unexpected clinical conundrum.
Physical examination of the chest demonstrated asymmetric thoracic movement and absent breath sounds on the right hemithorax. Hemothorax as a line-related complication was initially considered given the patient’s clinical course. We decided to proceed with bedside ultrasound of the thorax in anticipation of aspiration with possible tube thoracostomy. However, ultrasound failed to identify any fluid in the right hemithorax. Because of the patient’s hemodynamic stability chest computed tomography (CT) was performed, and showed appropriate central line placement and a large mucus plug in the right mainstem bronchus, causing collapse of the right lung with rightward tracheal deviation. Pulmonology performed a bedside bronchoscopy with evacuation of the mucus plug from the right mainstem. The remainder of the patient’s hospital course was uneventful, barring postoperative ileus, and she was discharged on hospital day 13. Figs.1–4 show the preprocedure X-ray, postprocedure X-ray, chest CT, and post-bronchoscopy chest X-ray.
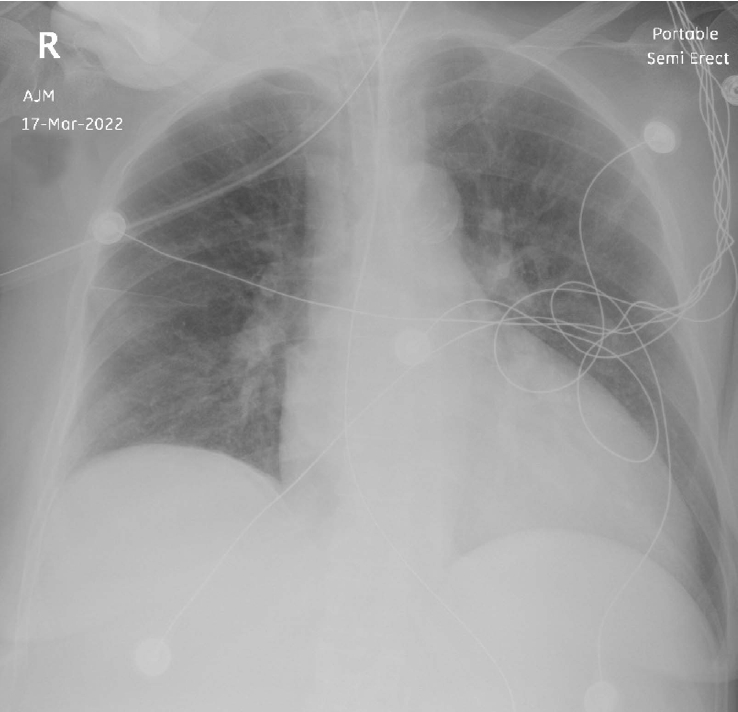
Chest X-ray 1 day prior to catheter placement: normal bilateral air spaces. Nasogastric tube and endotracheal tube noted in place.

Chest X-ray immediately following central line placement. Complete white-out of right thorax with right-sided tracheal deviation. Crowding of ribs noted on the right side.
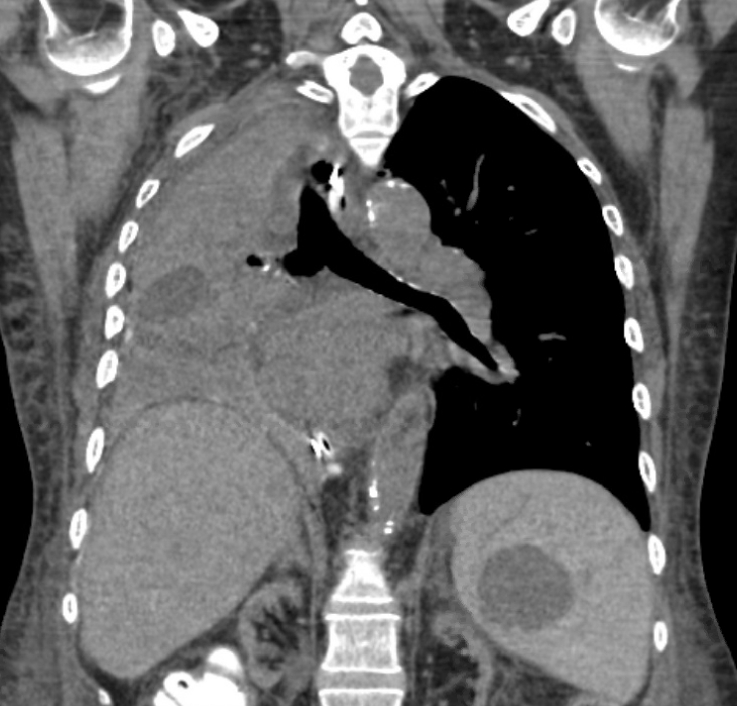
Computed tomography of the chest following line placement. Collapse of right lung with right-sided tracheal deviation.
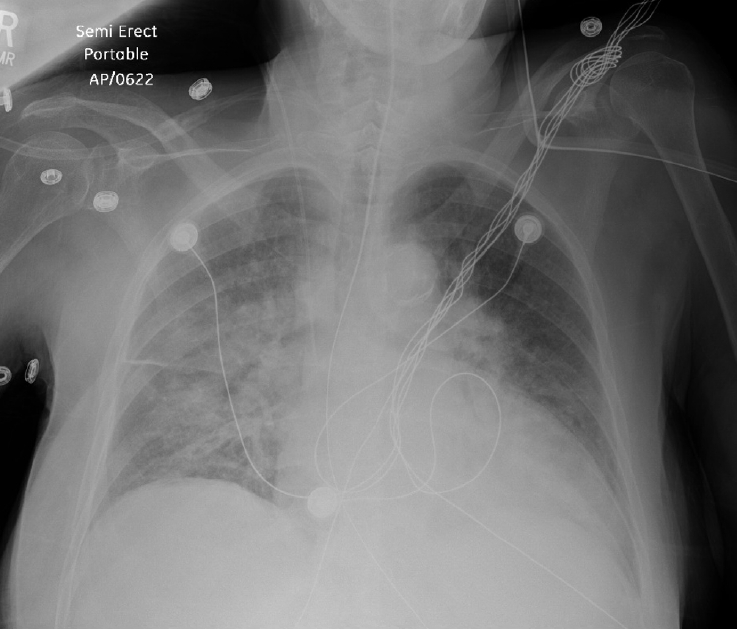
Chest X-ray following bronchoscopy. Partial resolution of right lung collapse with improved aeration.
Before the widespread use of ultrasound guidance, immediate complication rates post-central line insertion are between 6.3% and 11.8%, with these rates decreasing to 4.0% to 7.0% with ultrasound use [3,4]. Hemothorax following central line placement is a known complication. Central line placements in a surgical unit are mostly placed by surgical trainees who are also first responders to correlating a radiological finding on their patients. New imaging findings post-central line insertion similar to our patient can often pose a diagnostic dilemma and a decisionmaking challenge for young surgical trainees on call. A mistaken working diagnosis of hemothorax following central line insertion with opacification of the right hemithorax on chest X-ray can lead to an unnecessary tube thoracostomy in an unstable patient [4].
Mucus plugs can accumulate from desquamating mucus cells of the bronchus and lead to mechanical airway obstruction in postoperative patients, especially those with reduced cough capacity [1]. Occlusion by a mucus plug in the larger upper airway can lead to complete lung collapse, as seen in our case. Thoracic X-ray can be diagnostic when not confounded by any other thoracic intervention. Thoracic CT can be useful when the diagnosis is unclear. Bronchoscopy is usually both diagnostic and therapeutic [5].
While the dilemma in our example was ultimately innocuous and the patient improved, suspicion should remain high for such indolent processes in critically ill patients due to limited reserve and potential morbidity and mortality.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
FUNDING
None.
AUTHOR CONTRIBUTIONS
Conceptualization: all authors; Data curation: all authors; Formal analysis: all authors; Supervision: AV; Visualization: all authors; Writing–original draft: all authors; Writing–review & editing: all authors. All authors read and approved the final manuscript.
