Data integration using information and communication technology for emergency medical services and systems
Article information
Lack of resources is a challenging issue in emergency medicine. As a result, emergency medical systems and services (EMS) are being developed to overcome problems with limited emergency medical resources [1]. In particular, because it is difficult to provide high-quality emergency care outside of medical institutions, information between emergency medical centers and local communities must be connected efficiently [1–4].
The connections in the EMS can be discussed from two perspectives. First, for efficient emergency patient treatment and transportation based on medical guidance, the connection of information between the prehospital and hospital stages in the community must be performed in real time. Second, quality management should be performed based on large-scale integrated data between the two stages for the governance of EMS in the community.
Therefore, we can discuss the problems facing EMS in Korea from the perspective of information connections. The EMS policy in Korea, especially in the prehospital stage, is still dominated by consensus-based protocols rather than evidence-based protocols. This is because there is insufficient evidence to use an integrated dataset from the EMS [5]. The data management participants of the prehospital and hospital stages are different, and their information linkage is delayed for reasons such as the Personal Information Protection Act [6].
Various efforts have been made to derive scientific evidence on EMS issues by integrating large-scale data sources extracted from the community [7–10]. To integrate large-scale data sources, matching through key values is required; however, complete matching without missing values is difficult because of the heterogeneity of registries [6,11]. Even if it is possible to solve technical issues, integrating large-scale registries that include sensitive personal information (medical information) requires a latent period for administrative processes and approval from each authority. To overcome this delay, each authority needs a platform that can transmit the selected information from its registry in real time and collect it in a standardized format. Advances in 5G communications and clouding technology have enabled the use of these platforms in EMS [12].
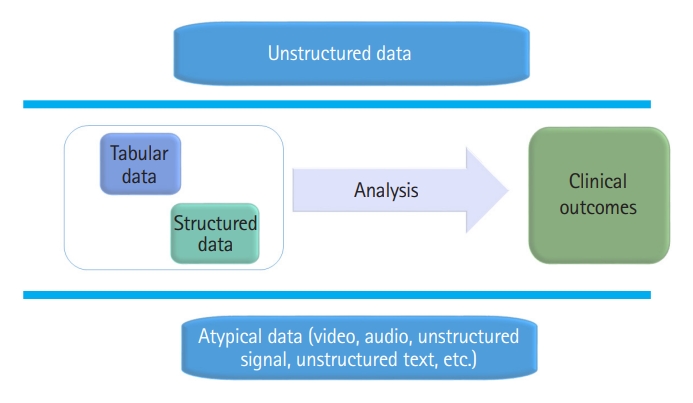
Most datasets used in the EMS field are composed of structured data. Structured data are created in a tabular form through manual primary processing. Owing to limitations in physical space and time, it is difficult for providers to convert various events that occur in the EMS field into tabular data sources in real time. Accordingly, unstructured data that cannot be converted into a tabular form cannot be stored as a dataset, and the reliability of structured data cannot be guaranteed [11]. Therefore, the current dataset, which was manually collected in tabular form, did not fully reflect the EMS event (Fig. 1).
The development of digital health technology makes it possible to collect information in an atypical form that is currently disappearing in the EMS field [13,14]. There are several studies in which unstructured data such as voice, vital signals, and video information are collected through wearable devices and 5G networks to derive evidence in emergency medicine. They showed that a technology capable of collecting unstructured data in real time in the field of emergency medicine could improve clinical practice [15–17]. In the future, the development of unstructured data collection and processing capacity can enhance first aid capacity by analyzing information that is not available in the EMS field in real time and can contribute to quality management from high-quality datasets [12,18,19].
The development of information and communication technology enables the rapid sharing of diverse and vast information generated from the EMS field and facilitates the data integration of each entity. This improves the quality of management provided at the prehospital stage and helps derive high-quality evidence that reflects the reality of the local community. However, information based on relevant legal and institutional arrangements and social implications is supported. Therefore, in the future, efforts to complete regionalization by establishing a data-driven precision EMS centering on the local community should continue.
Notes
ETHICS STATEMENTS
Not applicable.
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
FUNDING
This work was supported by the Severance Hospital Research Fund for Clinical Excellence (SHRC) (No. C-2022-0010).