Mortality among adult patients with sepsis and septic shock in Korea: a systematic review and meta-analysis
Article information
Abstract
Objective
To evaluate mortality from sepsis and septic shock in Korea during the past 10 years, we conducted a systematic review and meta-analysis.
Methods
We searched six databases for studies on mortality from sepsis and septic shock in adult patients. Primary outcomes were 28- or 30-day mortality and in-hospital mortality from sepsis and septic shock. To assess the risk of bias, we used the Newcastle-Ottawa Scale and Risk of Bias 2 tools. The protocol is registered in PROSPERO (No. CRD42022365739).
Results
A total of 61 studies were included. The mortality rates from sepsis and septic shock at 28 or 30 days were 22.7% (95% confidence interval [CI], 20.0%–25.6%; I2=89%) and 27.6% (95% CI, 22.3%–33.5%; I2=98%), respectively, according to the Sepsis-3 criteria. Furthermore, in accordance with the Sepsis-3 criteria, the in-hospital mortality rates were 28.1% (95% CI, 25.2%–31.1%; I2=87%) and 34.3% (95% CI, 27.2%–42.2%; I2=97%), respectively.
Conclusion
The mortality rates from sepsis and septic shock in Korea are high. In the case of septic shock, the in-hospital mortality rate is approximately 30%.
INTRODUCTION
Sepsis is a life-threatening multiorgan dysfunction caused by an inappropriate host response to infection [1]. Despite global efforts to minimize its lethality, sepsis remains the leading cause of death in critically ill patients and a burden on patients and healthcare systems worldwide [1–3]. Through campaigns to reduce the mortality rate of sepsis, experts in various fields have improved the survival rate by defining the Sepsis-3 diagnostic criteria and promoting adherence to recommended treatment protocols [1,4,5]. A total of 48.9 million incident cases and 11.0 million sepsis-related deaths have been reported in 2017, accounting for approximately 20% of global deaths during that time [2]. A recent meta-analysis showed that the pooled mortality rate of sepsis is 19.6% in North America, 23.6% in Europe, 18.7% in Australia, and 29.0% in China [6,7]. The mortality rates differ across countries because of disease severity, study type, period, and region, but different standard care protocols and health care systems also significantly affect the care and prognosis of patients with sepsis [6].
In Korea, previous research analyzing national health insurance data revealed sepsis mortality rates ranging from 17.5% to 30% [8–10]. However, those studies evaluated sepsis or septic shock based on diagnostic International Classification of Diseases, 10th Revision (ICD-10) codes in insurance records, not the sepsis criteria. Thus, their study populations might differ from the population described by the sepsis criteria and inaccurately depict sepsis mortality. Despite the large number of multicenter and single-center studies on sepsis and septic shock, including some multicenter registries, no previous studies in Korea reflect the overall sepsis fatality rate, to the best of our knowledge. To appropriately determine the mortality rate from sepsis and septic shock in Korea, a systematic review and meta-analysis are required. Therefore, we investigated the sepsis and septic shock mortality rates published for Korea during the past 10 years and analyzed those rates based on the Sepsis-3 criteria.
METHODS
Reporting guidelines and protocol registration
This study adhered to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) and the MOOSE (Meta-Analysis of Observational Studies in Epidemiology) guidelines for reporting information from observational studies [11,12]. This review protocol is prospectively registered in PROSPERO (No. CRD42022365739).
Search strategy
We systematically searched the PubMed, Embase, Cochrane Library, KMbase (Korean Medical Database), KoreaMed, and KISS (Korean Studies Information Service System) databases for studies about mortality and the frequency of sepsis and septic shock in adult patients that were published between January 2012 and July 2022. As our search strategy, we combined medical subject headings terms and free terms related to “sepsis,” “septic shock,” and “South Korea” and included Embase subject headings and text words. The detailed search strategy is presented in Supplementary Table 1.
Study selection
We selected studies through title and abstract screening and used the following inclusion criteria: confirmed sepsis, severe sepsis or septic shock in adult patients according to the Sepsis-1, -2, or -3 criteria, and studies conducted in Korea and published between January 1, 2012 and September 23, 2022. We excluded studies with insufficient data and those involving sepsis patients from specific disease groups, reviews, case reports, editorials, letters, conference abstracts, meta-analyses, and animal studies. To prevent duplicate data, we selected studies with the longest study period and largest sample size when we found multiple studies that shared the same registry or institution.
Data extraction
Two reviewers independently extracted the relevant data about the patients in the included studies, and discrepancies between reviewers were discussed and resolved by consensus. We extracted the following variables: publication data; study design and settings; patient information—number of participating centers, patient locations (emergency room, ward, or intensive care unit [ICU]), number of patients, and deaths; sepsis diagnostic criteria; and the time of outcome measurement (28- or 30-day mortality and in-hospital mortality).
Quality assessment of individual studies
The Newcastle-Ottawa Scale, which divides an eight-item score into three domains, was used to evaluate nonrandomized studies [13]. The Risk of Bias 2 tool was used to evaluate randomized controlled trials [14]. Each article was rated based on selection (maximum, four stars), comparability (maximum, two stars), and outcome (maximum, three stars). Both reviewers assessed the 61 included studies independently. Unresolved disagreements between reviewers were resolved by discussion or consultation with a third reviewer.
Statistical analysis
Individual and pooled statistics were calculated as frequencies of sepsis and septic shock diagnosed at admission or during an ICU stay to estimate mortality in the ICU or hospital and to estimate mortality at 28 or 30 days. A random effects model was used to assess mortality for each outcome. Separate analyses were performed in the following subgroups: diagnosed according to Sepsis-3 and non-Sepsis-3 criteria; retrospective and prospective studies; single-center and multicenter studies; and patient location (emergency room, ward, or ICU). Statistical heterogeneity was visually assessed using forest plots and formally assessed using I2. Publication bias was evaluated using a Begg funnel plot. All analyses were performed using the R ver. 4.0.0 (The R Foundation for Statistical Computing) software packages “meta” (ver. 6.1-0) and “metafor” (ver. 3.8-1). A P-value of <0.05 was considered statistically significant.
RESULTS
Study selection
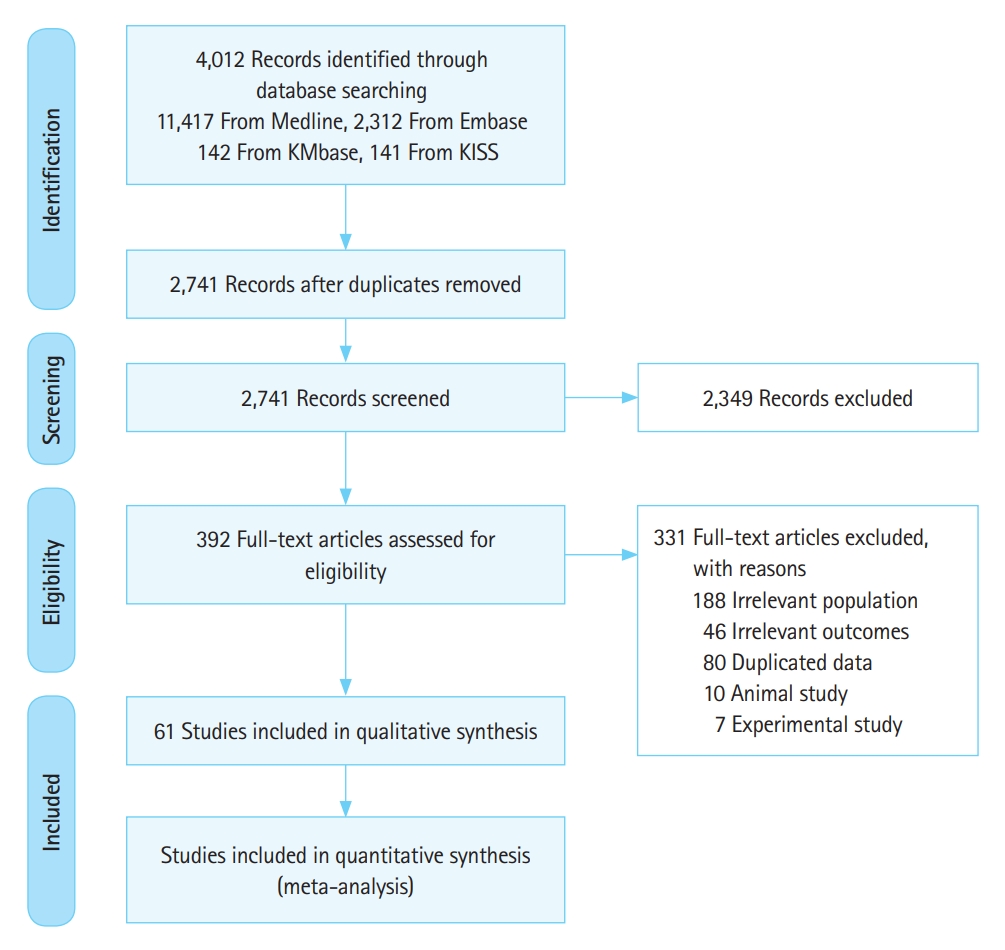
Our database search yielded 4,012 records. From them, 1,271 duplicates were removed, and 2,349 records were excluded in the review of titles and abstracts. Of the remaining 392 records, 331 were also excluded based on the full article review because they had an irrelevant population (n=188), irrelevant outcome (n=46), duplicated data (n=80), animal study (n=10), or experimental study (n=7); details are provided in Supplementary Tables 2 and 3 [15–75]. Therefore, 61 studies of sepsis and septic shock mortality are included in this review [15–75]. Fig. 1 shows the study flow for the selection process.
Study characteristics
Of the 61 included studies, 26 were prospective cohort studies, 33 were retrospective cohort studies, and two were randomized clinical trials; 46 were single-center studies, and 15 were multicenter studies, nine of which investigated the same two prospective sepsis registries (five used the Korean Shock Society [KoSS] registry [48,50,52,67,75] and four used the Korean Sepsis Alliance [KSA] registry [28,33,59,73]). The KoSS registry was established in 2013 to study patients who went into septic shock in emergency departments (EDs); it has been prospectively collecting data since October 2015 [76]. At the beginning of enrollment, 10 EDs participated, but in the most recent study, which used data up to December 2019, 12 EDs participated [48]. The KSA registry was organized mainly by pulmonologists and critical care medicine physicians from 16 secondary and tertiary hospitals nationwide; this database covers 19 hospitals and includes patients who were diagnosed with sepsis in EDs or hospitals [28].
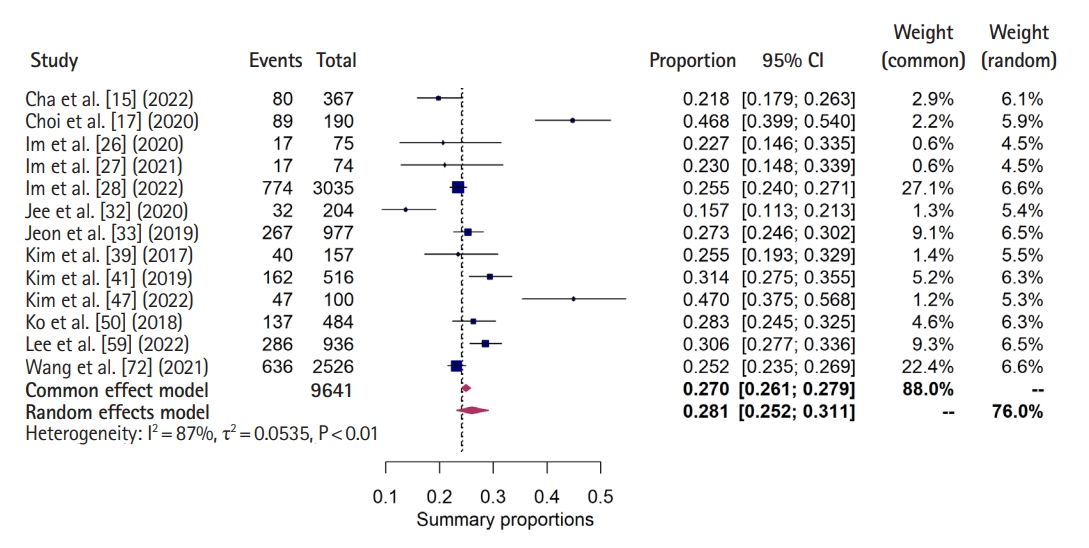
Data on 28- or 30-day mortality and in-hospital mortality among sepsis patients were extracted from 27 and 17 studies, respectively, and those data for septic shock patients were extracted from 32 and 18 studies, respectively. Table 1 summarizes the characteristics of the included studies [15–75].
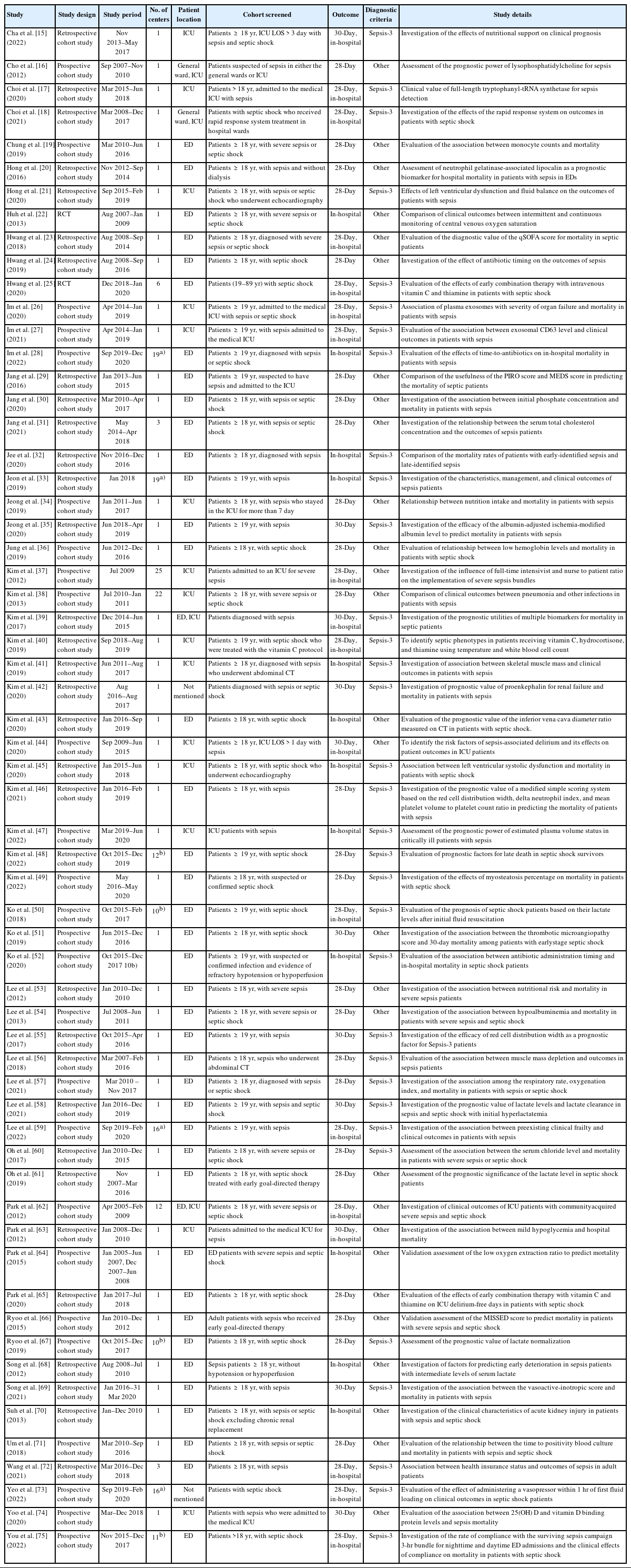
Sepsis mortality
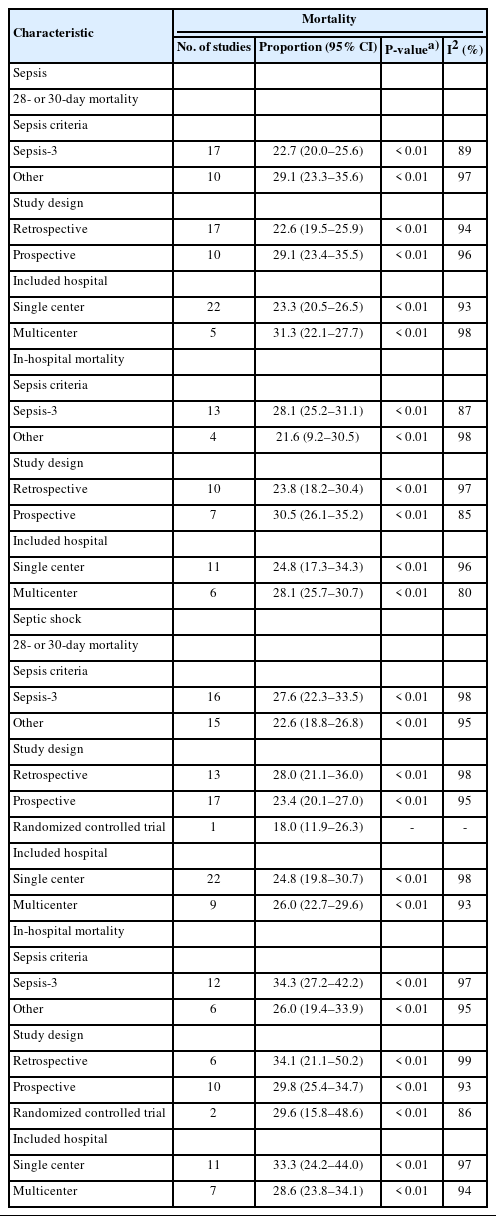
The studies that examined 28- or 30-day mortality from sepsis analyzed 22,050 patients. The 28- or 30-day mortality from sepsis diagnosed using the Sepsis-3 criteria was 22.7% (95% confidence interval [CI], 20.0%–25.6%; I2=89%) (Table 2 and Fig. 2) [15,17,21,26,27,35,39,42,46,50,55–59,69,72]. The range of mortality in the included studies was 14.4% to 40.8%. In addition, the 28- or 30-day mortality rate by including all sepsis criteria was 24.8% (95% CI, 22.1%–27.7%; I2=95%) (Supplementary Fig. 1) [15,17, 20,21,26,27,29–31,34,35,39,42,44,46,50,55–59,63,69,71,72,74]. In the subgroup analyses, 28- or 30-day mortality from sepsis was 22.6% (95% CI, 19.5%–25.9%; I2=94%) in retrospective cohort studies, 29.1% (95% CI, 23.4%–35.5%; I2=96%) in prospective studies, 23.3% (95% CI, 20.5%–26.5%; I2=93%) in single-center studies, and 31.3% (95% CI, 23.4%–40.4%; I2=98%) in multicenter studies (Table 2).
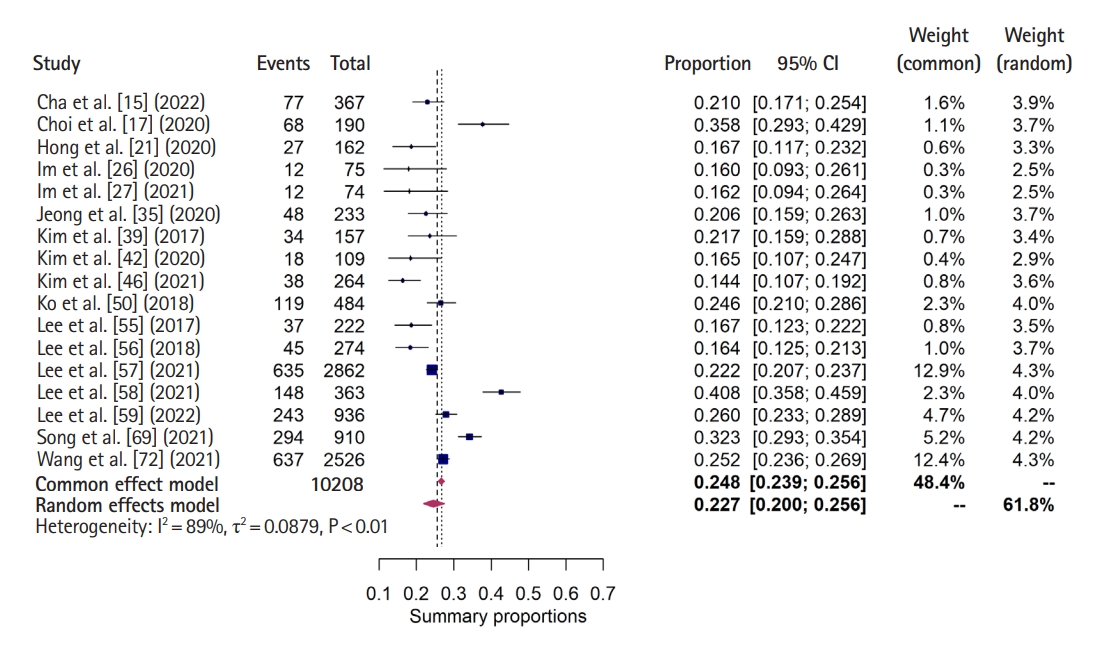
Forest plot for 28- or 30-day mortality from sepsis using the Sepsis-3 criteria. CI, confidence interval.
The studies of in-hospital mortality from sepsis analyzed 11,595 patients. In-hospital mortality from sepsis diagnosed using the Sepsis-3 criteria was 28.1% (95% CI, 25.2%–31.1%; I2=87%) (Table 2 and Fig. 3) [15,17,26–28,32,33,39,41,47,50,59,72]. The range of mortality was 15.7% to 47.0%. In addition, in-hospital mortality by including all sepsis criteria was 26.3% (95% CI, 22.6%–30.5%; I2=95%) (Supplementary Fig. 2) [15,17,26–28,32,33,39,41,44,47,50,59,63,68,70,72]. In the subgroup analyses, the in-hospital mortality from sepsis was 23.8% (95% CI, 18.2%–30.4%; I2=97%) in retrospective cohort studies, 30.5% (95% CI, 26.1%–35.2%; I2=85%) in prospective studies, 24.8% (95% CI, 17.3%–34.3%; I2=96%) in single-center studies, and 28.1% (95% CI, 25.7%–30.7%; I2=80%) in multicenter studies (Table 2).
Septic shock mortality
The studies for 28- or 30-day mortality from septic shock analyzed 25,101 patients. The 28- or 30-day mortality from septic shock diagnosed using the Sepsis-3 criteria was 27.6% (95% CI, 22.3%–33.5%; I2=98%) (Table 2 and Fig. 4) [15,17,25–27,42,46,48–50,58,60,67,69,73,75]. The range of mortality was 12.6% to 52.9%. In addition, the 28- or 30-day mortality rate by including all sepsis criteria from septic shock was 25.1% (95% CI, 21.8%–28.8%; I2=97%) (Supplementary Fig. 3) [15,17,19,24–27,29,36–38,42,46,48–51,53,54,58,60-62,65–67,69,73–75]. In the subgroup analyses, the 28- or 30-day mortality from septic shock was 28.0% (95% CI, 21.1%–36.0%; I2=98%) in retrospective cohort studies, 23.4% (95% CI, 20.1%–27.0%; I2=95%) in prospective studies, 18.0% in the one randomized controlled trial, 24.8% in single-center studies (95% CI, 19.8%–30.7%; I2=98%), and 26.0% in multicenter studies (95% CI, 22.7%–29.6%; I2=93%) (Table 2).

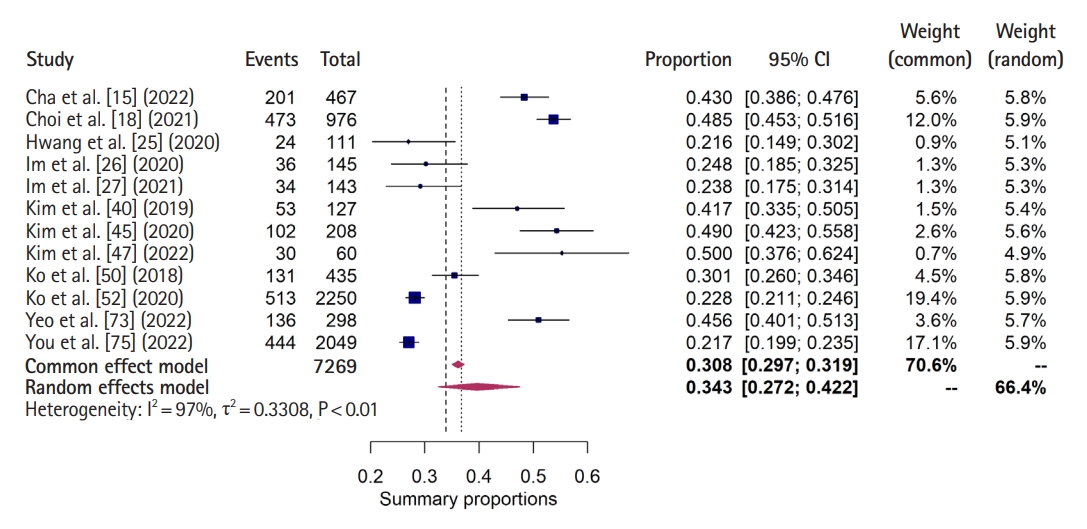
Forest plot for 28- or 30-day mortality from septic shock using the Sepsis-3 criteria. CI, confidence interval.
The studies of in-hospital mortality from septic shock analyzed 10,769 patients. In-hospital mortality from septic shock diagnosed using the Sepsis-3 criteria was 34.3% (95% CI, 27.2%–42.2%; I2=97%) (Table 2 and Fig. 5) [15,18,25–27,40,45,47,50,52,73,75]. The range of mortality was 21.6% to 50.0%. In addition, in-hospital mortality by including all sepsis criteria from septic shock was 31.4% (95% CI, 26.1%–37.3%; I2=97%) (Supplementary Fig. 4) [15,18,22,23,25–27,37,40,43,45,47,50,52,62,64,73,75]. In the subgroup analyses, the in-hospital mortality from septic shock was 34.1% (95% CI, 21.1%–50.2%; I2=99%) in retrospective cohort studies, 29.8% (95% CI, 25.4%–34.7%; I2=93%) in prospective studies, 29.6% (95% CI, 15.8%–48.6%; I2=86%) in randomized controlled trials, 33.3% (95% CI, 24.2%–44.0%; I2=97%) in single-center studies, and 28.6% (95% CI, 23.8%–34.1%; I2=94%) in multicenter studies (Table 2).
Quality assessment
When we used the Newcastle-Ottawa Scale to evaluate the quality of the included articles, we found that 19 studies were of poor quality. The following assessments were derived from the other studies, which were rated as good quality: 24 studies received 9 points, and the others received 7 or 8 points. Using the Risk of Bias 2 for the two randomized controlled trials, one study had low bias, and the other study had high bias (Supplementary Tables 2, 3).
Publication bias
All the funnel plots made to assess the publication bias for each outcome showed symmetry. The funnel plots for sepsis (28- or 30-day and in-hospital mortality) and septic shock (28- or 30-day and in-hospital mortality) are shown in Supplementary Fig. 5.
DISCUSSION
To the best of our knowledge, this is the first meta-analysis to investigate mortality among sepsis and septic shock patients in Korea. We found that the pooled mean of the 28- or 30-day mortality rate and in-hospital mortality rate are 24.8% and 26.3%, respectively, in sepsis patients, and 25.1% and 31.4%, respectively, in septic shock patients. Those data reflect the actual clinical prognosis of sepsis patients classified according to the sepsis criteria used in hospitals. The 28- or 30-day sepsis mortality rate in a national cohort study by Oh et al. [77] is higher than our result at approximately 30%. However, that study used National Health Insurance Service of Korea data and ICD-10 codes to classify sepsis patients; therefore, the diagnosis of sepsis might have been overestimated by including septic shock. Moreover, deaths unrelated to sepsis might have been included in the overall mortality data of that study.
The sepsis mortality rates in the present study are higher than those reported in a recent meta-analysis for the United States (19.6%) and Australia (18.7%), but similar to that in Europe (23.6%) and lower than that in China (29.1%) [6,7]. In contrast, the mortality rate among septic shock patients appears to be similar or lower than that in other countries (North America, 33.7%; Australia, 26.4%; Europe, 32.5%; China, 35.9%) [6,7]. Most of the sepsis studies evaluated in our meta-analysis included sepsis with shock, introducing the possibility of heterogeneity among studies and inaccurately high death rates. In addition, because our study includes research from the past 10 years, our data are based on several sets of sepsis criteria (Sepsis-1, -2, and -3), and that inconsistency could increase heterogeneity. On the other hand, we found clinically relevant results when the Sepsis-3 criteria were used.
Another finding of this study is that in-hospital mortality was higher than 28- or 30-day mortality in sepsis and septic shock patients. This result is consistent with that of previous meta-analyses conducted by Vincent et al. [78] and Liu et al. [7] in Europe, North America, and China. The studies included in this meta-analysis presented their outcomes as either 28- or 30-day mortality or in-hospital mortality, and the study populations differed in their inclusion of sepsis or septic shock patients. In other words, 28- or 30-day mortality and in-hospital mortality were not measured consecutively in the same studies but represent the sum of values extracted from different studies. Therefore, because of the statistical constraints of a meta-analysis, caution is needed in interpreting the result that in-hospital mortality was higher than 28- or 30-day mortality in sepsis and septic shock patients.
We analyzed the mortality rates from sepsis and septic shock after dividing the patients into those diagnosed with the Sepsis-3 criteria and those diagnosed with other criteria. The 28- or 30-day mortality rate and in-hospital mortality rates for septic shock diagnosed according to the Sepsis-3 criteria were 27.6% and 34.3%, respectively, which are higher than those based on the non-Sepsis-3 criteria (28- or 30-day mortality, 22.6%; in-hospital mortality, 26.0%) (Figs. 4, 5) [15,17,18,25–27,40,42,45–50,52,58,60,67,69,73,75] That finding is consistent with a previous meta-analysis in Europe and North America, which reported that in-hospital septic shock mortality increased significantly, from 39.0% to 52.1%, when the Sepsis-3 criteria were used for diagnosis [78]. The criteria prior to Sepsis-3 defined sepsis as a state with at least two of the four systemic inflammatory response syndrome (SIRS) criteria, which focus solely on the inflammatory response [79,80]. Because the SIRS criteria do not exactly reflect organ dysfunction and life-threatening conditions, the new Sepsis-3 criteria, which were published in 2016, include the Sequential Organ Failure Assessment (SOFA) score and lactate level [1]. Therefore, the increase in septic shock mortality when using the Sepsis-3 criteria could be explained by the advanced disease severity reflected by the change in diagnostic criteria.
Variations in mortality rates among the included studies are likely attributable to differences in the disease severity of the patients. For example, to identify the risk factors of sepsis-associated delirium and their effects on the outcomes of ICU patients, Kim et al. [44] excluded patients with <24 hours of ICU stay or deep or full sedation from their assessment of 28- or 30-day sepsis mortality. Those factors could exacerbate the severity of the patients included, resulting in a higher mortality rate. In addition, Hong et al. [20] excluded patients admitted for hemodialysis or peritoneal dialysis, transferred from other hospitals, or admitted for palliative care. In that case, the mortality rate might have been underreported due to the exclusion of critically ill patients.
It is challenging to generalize the findings of this study to all sepsis patients in Korea. The majority of the research included in this meta-analysis was conducted at tertiary medical institutions or large hospitals, and the sepsis registries include only hospitals with the ability to provide quality care. Thus, data from institutions that are treating sepsis but not reporting their results were not included here. If the outcomes from ineffective-performance medical settings are not considered, the overall results of sepsis treatment might appear to be better than they actually are. Additionally, a recent Korean report indicated that the surviving sepsis campaign had low compliance [81]. Therefore, the mortality rate might increase further when the sepsis outcomes of all medical institutions are considered. Further investigation is needed to examine sepsis outcomes according to the performance level of the medical institution.
This review has several limitations. First, heterogeneity among the studies included in the meta-analysis is very high, all over 95%. One reason for this high heterogeneity is the diversity of study designs included in the analysis. In addition, the definition of sepsis in the included studies was heterogeneous because the new Sepsis-3 criteria were only published in 2016, and that diversity of definitions might have resulted in a wide range of mortality rates. Therefore, we analyzed the mortality rates according to the use of the Sepsis-3 and non-Sepsis-3 criteria. Second, the sepsis criteria were met when patients were included in these studies, but it is possible that critically ill patients might have been only selectively included based on particular domains, such as the lactate level. Third, when several studies were conducted in a single institution or used the same registry during the same study period, we selected only the study with the longest study period and largest sample size because we suspected that the study population might be duplicated. Thus, despite our efforts to include as many studies as possible, we cannot completely rule out the possibility of selection bias. Fourth, despite that attempt to prevent duplicated data, the possibility of duplication between registry studies and single-center studies whose data are included in that registry remains. Fifth, the medical history and care conditions of individual patients, which influence the mortality rate, were not considered. Personal factors were not considered in this study, and our meta-analysis simply confirmed the mortality rate.
In conclusion, our study shows that the mortality rates from sepsis and septic shock in Korea are high. In the case of septic shock, the in-hospital mortality rate is approximately 30%, and that rate was higher when septic shock was diagnosed according to the Sepsis-3 criteria than when it was diagnosed using other criteria.
SUPPLEMENTARY MATERIAL
Supplementary material is available at https://doi.org/10.15441/ceem.23.005.
Supplementary Table 1.
Search strategy
Supplementary Table 2.
Quality assessment using NewcastleOttawa Scale for cohort studies
Supplementary Table 3.
Quality assessments using Risk of Bias 2 for randomized controlled trials
Supplementary Fig. 1.
Forest plot for 28- or 30-day sepsis mortality by including all sepsis criteria.
Supplementary Fig. 2.
Forest plot for in-hospital sepsis mortality by including all sepsis criteria.
Supplementary Fig. 3.
Forest plot for 28- or 30-day septic shock mortality by including all sepsis criteria.
Supplementary Fig. 4.
Forest plot for in-hospital septic shock mortality by including all sepsis criteria.
Supplementary Fig. 5.
Funnel plots for each outcome.
Notes
ETHICS STATEMENTS
Not applicable.
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
FUNDING
None.
AUTHOR CONTRIBUTIONS
Conceptualization: MN, CA; Data curation: MN, YP, MW; Formal analysis: IYK, JL; Visualization: CA; Writing–original draft: MN, CA; Writing–review & editing: all authors. All authors read and approved the final manuscript.
References
Article information Continued
Notes
Capsule Summary
What is already known
Mortality rates for sepsis and septic shock vary between studies. To appropriately determine the mortality rate from sepsis and septic shock in Korea, it is necessary to conduct a systematic review and meta-analysis.
What is new in the current study
This is the first meta-analysis of published sepsis and septic shock mortality rates in Korea. Sepsis mortality in Korea was similar or higher than in the United States and Europe, whereas septic shock mortality was lower.