Challenges surrounding the emergency physician workforce and their impact on the Emergency Medicine Match
Article information
INTRODUCTION
Although we believe the future of emergency medicine (EM) remains bright, short-term forecasts are clouded by concerns regarding the 2022 and 2023 Match results and projections of a future surplus of emergency physicians (EPs) [1–4]. On social media, at national conferences, and within our own emergency departments (EDs), our specialty’s trajectory is a common conversation piece with heated opinions. But key questions remain: what got us here and where are we going?
THE (UN)EXPECTED MATCH RESULTS
For many, the 2023 Emergency Medicine Match results came as a surprise. As others have commented, 554 initially unmatched positions in the 2023 Match should have been expected [4]. Amidst a growing controversy over the EP workforce, the Match heightened concerns from many about our specialty’s future [2–5]. However, an important caveat to the Match results are that EM—compared to most other specialties—has one of the fastest 5-year rates of growth in number of new residency programs [6]. Since joining the National Registry Matching Program in 1983, EM has added positions to the Match each year [7]. In 2018, EM offered 2,278 positions and, since then, it has added 732 new positions—a 32% increase! This increase outpaces other specialties (e.g., from 2018 to 2023 internal medicine, surgery, and pediatrics had a 29%, 27%, and 8% proportional growth, respectively) [7,8].
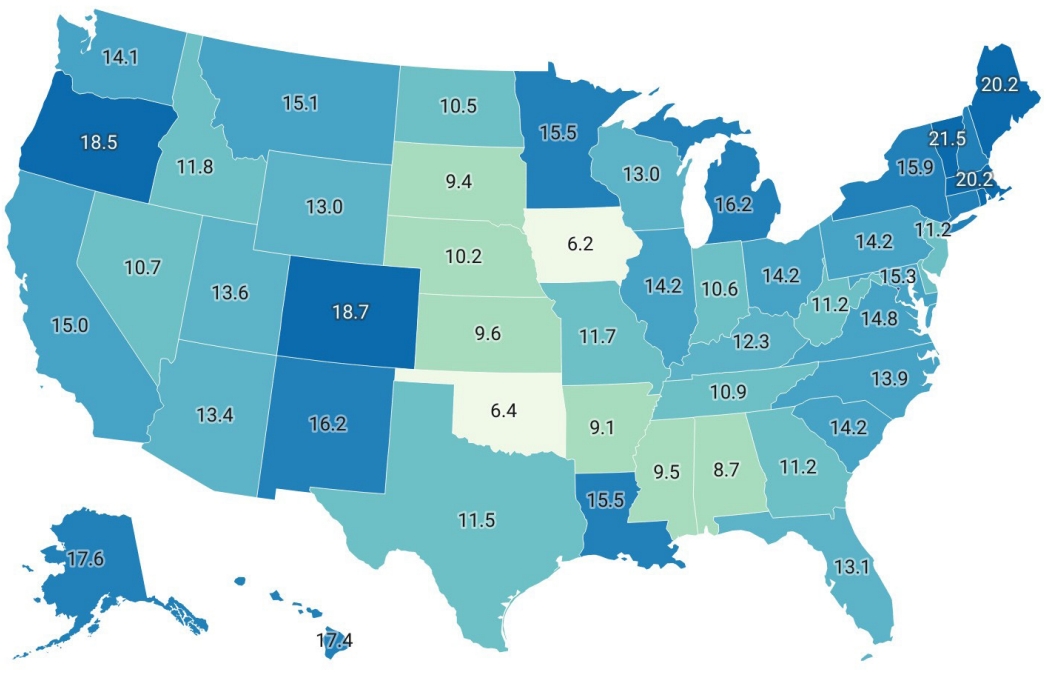
Reasons for the accelerating growth in EM residency positions are multifactorial. First, the migration of osteopathic programs to the Accreditation Council for Graduate Medical Education (ACGME) under the Single Accreditation System (SAS) from 2015 to 2020 resulted in the inclusion of osteopathic programs [9]. Second, there has been a rapid increase in the number of newly accredited residency programs [10]. This includes an increasing number of programs at institutions without a major teaching hospital affiliation and programs sponsored by for-profit hospitals [5]. These new programs are disproportionately added to areas with an already existing density of EM programs (Fig. 1) [5,10].
The lack of major teaching hospital affiliation among newly accredited EM residency programs is troubling [5]. Teaching hospital EDs tend to have higher visit volumes and more often provide complex, higher acuity care by nature of their status as referral centers. This offers EM residents training in specialized, multidisciplinary care. However, there are a finite number of teaching hospitals with the necessary infrastructure to create the academic environment for an EM residency. Compared to EM programs with a major teaching hospital affiliation, more recently launched EM programs based at hospitals without a major teaching hospital affiliation are less likely to be designated as a trauma, stroke, or burn center [5]. We acknowledge that teaching hospitals are less likely to be located in rural settings; thus, in medically underserved areas, teaching hospital affiliation may not need to be a prerequisite for EM residency accreditation. However, alternate indicators of the breadth and complexity of training opportunities should be met. Unfortunately, annual ED visit volumes at some newly accredited residencies’ primary site—the ED where the program is based and where residents spend most of their time—are consistently below the ACGME’s minimum threshold for annual visit volumes [5]. These low volumes raise concerns about the quality of the educational environment for EM residents in these programs. Moreover, these data suggest that some of these programs do not meet ACGME Common Program Requirements [5].
Another key driver of the growth in EM residencies is the growing role of for-profit entities in academic EM [1,2,11]. As an example, the publicly traded hospital operator Hospital Corporation of America (HCA) accounts for a sizable share of all newly accredited EM residency programs in the United States. Beyond EM, HCA sponsors more than 5,300 residents and fellows in more than 300 residencies and fellowships [12]. Of equal concern is the rise of private equity ownership in EM physician groups, which is estimated to affect 25% to 40% of all US EDs [13]. Concerns have been raised regarding staffing models at institutions affiliated with for-profit entities—in particular, that low physician staffing may adversely impact time and resources available for resident education and potentially even adversely impact patient care [14,15]. The role of for-profit entities places health care facilities at higher financial risk, increasing the likelihood of disruptions to EM residency training. The rapid closure of the Summa Health and Hahnemann EM residencies in 2019 are cautionary tales where financial decisions inflicted direct harm on resident education [16]. The recent bankruptcies of two of the largest EM staffing firms—both backed by private equity—in the wake of the 2022 No Surprises Act raise questions about the continued role of for-profit entities in EP workforce and training [17,18].
THE EP WORKFORCE (AND ATTRITION FROM IT)
Another potential factor in the 2023 Match outcome was a 2021 report projecting an overall surplus of EPs in the United States by 2030 [3]. The “overall” aspect of this surplus is important; a key assumption of this work was uniform rates of attrition (with annual attrition estimated to range from 2%–4%). We believe that a single national projection is overly simplistic and there are mismatches in where EPs are needed and where they desire to live. Although the EP workforce continues to grow overall, there is persistent regional variation in both EP supply and EP demand [19]. Specifically, urban markets are increasingly saturated and projections of surpluses in these markets are likely correct [19,20]. But there are also EP “deserts” in large swaths of the country [20]. Much of rural America has either insufficient or absent access to EP care (Fig. 2) [20,21]. This includes even more limited access to EPs with EM residency training and EM board certification [21,22]. Recent work demonstrates that this desert continues to grow as the proportion of EPs working in rural areas decrease [20]. Therefore, rural EP shortages are likely to worsen in the coming years.
This widening rural-urban gap is largely driven by an older population of rural EPs who are nearing the retirement age and leaving the clinically active workforce [20–22]. It is exacerbated by evidence demonstrating that residency graduates are likely to continue practicing in urban and suburban environments similar to their training programs [10,23]. Since most new residency programs are not in underserved rural areas, the vision of every person seeking emergency care being seen by an EM-trained (and EM board-certified) EP seems less and less feasible [24]. Regardless of the drivers, the end result is the same—an increased reliance on nonphysician providers and non-EM board-certified physicians [25,26].
Another equally important assumption is that the 2021 estimate of 2% to 4% annual attrition among EPs is based on data from 2013–2019 [3]. More recent evidence suggests the annual rate of EP attrition is at least 5% [27]. Alarmingly, attrition during early stages of the COVID-19 pandemic was more than 8% overall—and even higher for EPs without EM board certification (11%) and those in rural locations (11%) [27]. Given the ongoing stresses of COVID-19, burnout, crowding, boarding, the rise of hallway medicine, and attrition rates are likely to remain higher than prior estimates.
THE 5 (AND 10) YEAR HORIZON
The current trajectory suggests that an increased number of EPs will enter into the clinically active workforce and, with more EM residency programs added each year, the total number of EPs entering the workforce will grow each year [10,20]. Although some residency programs may close, the rate of new program growth will likely result in an overall net gain in EM residency programs [5,10]. This growth will be primarily in urban markets—and reflexively EPs will do what they do best and accommodate. Those who desire to work in competitive markets will find novel ways to provide emergency care (e.g., telehealth) and for some, expand what we now consider our scope of practice. Meanwhile, many rural Americans will continue to receive emergency care by persons without either EM residency training or EM board certification, or nonphysician providers.
We believe the 2023 Match results are a natural extension of workforce and market factors. While it is possible that the unfilled slots will eventually lead to a “reset” and closure of EM residency programs with persistently unmatched positions, the coming years may be a painful transition. To mitigate future adverse impacts, policy solutions and action are needed. Simply waiting for programs with persistently high rates of unmatched positions to close will not resolve the underlying issues that led to the current situation. We recommend critically examining and strengthening ACGME accreditation requirements, which are currently undergoing revision. We also believe more research is needed to evaluate the impact of for-profit entities on EM training and that all national EM organizations should jointly advocate for greater transparency in this regard. Finally, it is important to create and promote incentives for board-certified EPs to practice in rural and underserved areas, including Public Service Loan Forgiveness programs [20]. The specialty of EM is at a critical inflection point. While we have no doubt it will survive, now is the time to advocate together for changes that secure a bright future for our specialty.
Notes
ETHICS STATEMENT
Not applicable.
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
FUNDING
None.
AUTHOR CONTRIBUTIONS
Conceptualization: all authors; Writing–original draft: all authors; Writing–review & editing: all authors. All authors read and approved the final manuscript.