INTRODUCTION
Traumatic brain injury (TBI) is a major cause of death and disability, with over 1.1 million emergency department visits, 235,000 hospital admissions, and 50,000 deaths occurring annually in the United States alone. In addition, 30.5% of all injury deaths include a diagnosis of TBI [1,2]. The prevalence of long-term disability due to TBI in the United States is between 3.2 to 5.3 million, with lifetime medical costs in 2010 estimated at $11.5 billion [1,3]. In addition to functional and cognitive impairment, disabilities extend to include psychological stressors, such as increased irritability, anxiety, depression, and suicidal ideation [4,5].
Traditionally, rates of TBI have been thought to be highest in adolescents and young adults, although an increase in the elderly (age >65) has been observed. Among adults aged 65 and older, there was an increase in fall-related TBIs from 2002 to 2006, with a 46% increase in emergency department visits, a 34% increase in hospitalizations, and a 27% increase in death [6]. Therefore, with the increase in the average age in the US, the demographics of TBI may be evolving, which will impact outcome and management strategies.
Previous studies have shown large public datasets, such as the NHAMCS (National Hospital Ambulatory Medical Care Survey), have disposition discrepancies, which reflects a measure of their internal validity. As a result, these datasets, which are widely used for research, may have significant limitations in data reliability [7,8]. Since many prior studies on TBI rely on these datasets, analysis of trends and outcomes in other databases would be helpful to better understand areas in need of further study.
One recent study showed that the Illinois Department of Public Health (IDPH) Trauma Registry has infrequent incongruent dispositions, a finding suggesting high reliability [9]. Studies suggest that unreliable datasets may be due to insufficient abstractor training, and the IDPH Trauma Registry abstractors are required to have both medical and abstractor training, which may contribute to the quality of this localized data [9]. To further explore temporal trends in TBI using a high-reliability dataset, we sought to examine the IDPH Trauma Registry to determine changes in demographics and outcome of patients, in Illinois, presenting with TBI over a 9-year timeframe.
METHODS
Study design and setting
This is a retrospective database review, analyzing data from the IDPH Trauma Registry. Data included in this study captures patients treated for TBI at a Level 1 Trauma Center and large tertiary care hospital by the trauma service during the years 2004 to 2012, inclusive. The dataset includes all patients with traumatic injuries that were seen and admitted to the trauma service. Specifically, this includes patients that were transferred to the trauma center and subsequently admitted, including patients that were dead on arrival or died in the emergency department. Patients that died on the scene of the traumatic injury but were not transported to a trauma center, and patients who were treated in the emergency department and discharged in less than 12 hours were not included in the database. Criteria to be seen by the trauma service on arrival in the emergency department were initiated in the field and includes: patients with a head injury with persistent unconsciousness or focal signs such as seizures; posturing or the inability to respond to simple commands; transmediastinal gunshot wounds; spinal cord injury with paralysis; maternal trauma with significant mechanism and/or obvious trauma at 20 to 32 weeks gestation; pediatric trauma including blunt or penetrating head, chest, or abdominal trauma. For blunt or penetrating trauma, patients with unstable vital signs (systolic blood pressure <90 mmHg), respiratory compromise (respiratory rate <10 or >29 breaths/min), or head injury with Glasgow Coma Score ≤10 were included. The Glasgow Coma Scale is used to categorize traumatic head injuries based on severity. Total scores of 13 to 15 is defined as mild, 9 to 12 as moderate, 3 to 8 as severe [10]. For anatomical injury, penetrating injury of the head, neck, chest or abdomen, two or more body regions with potential life or limb threat, amputation above the wrist or ankle, limb paralysis above the wrist or ankle, flail chest, or two or more proximal long bone fractures were included. For mechanism of injury, ejection from a motor vehicle, death in the same passenger compartment, falls >20 feet, falls >3 times the body length (for children), and maternal trauma >24 weeks were included. For trauma transfers, patients with a head injury as seen on computed tomography imaging (subdural hematoma, subarachnoid hemorrhage, intraparenchymal hemorrhage) with a Glasgow Coma Scale <9, or if the transferring physician felt the patient would require intensive care unit level of care were included.
This study was institutional review board approved and granted a waiver of the consent process since the data was publicly available and de-identified.
Methods of measurement
Basic demographics, such as age and sex, and clinical outcomes from over 3,000 patients were exported from the database into Excel. Outcomes, such as ventilator days, hospital admission days, intensive care unit days, Glasgow Coma Scale and mortality were compared across time and age. Data points were grouped by quarter to provide a reasonable sample size per time period. This data was analyzed and compared over the years with logistic regression models which used age, sex, and clinical outcomes as variables.
Outcome measures
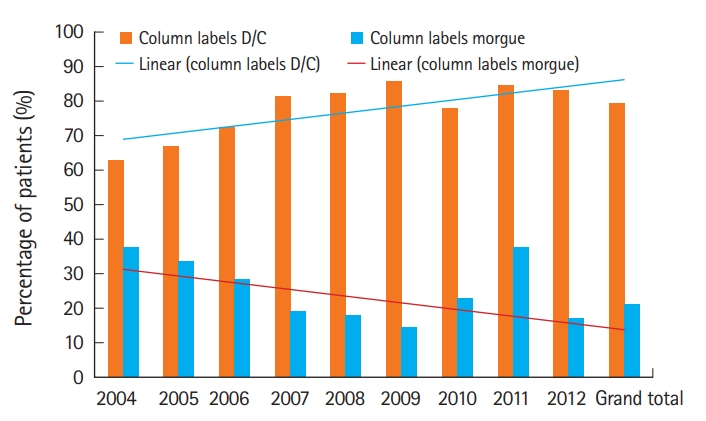
Clinical outcomes were recorded as one of three categories: discharged, morgue, or other. An outcome of ‘discharged’ consisted of several dispositions including: transferred to another hospital or subacute hospital, discharged home or self-care, discharged to child protection agency, discharged to nursing home/skilled nursing facility/intermediate care facility/residential, discharged to jail/prison, discharged to a psychiatric hospital, discharged to a rehabilitation center, and left against medical advice. An outcome of ‘morgue’ was any patient that did not survive to discharge. This includes patients that were sent to the morgue, funeral home, medical examiner or coroner. An outcome of ‘other’ was given to those whose discharges were unknown. This category only accounted for 0.07% of the patients that were analyzed, and therefore was not included on figures.
RESULTS
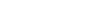
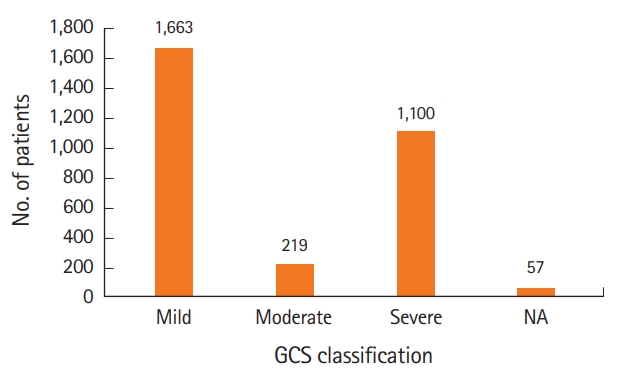
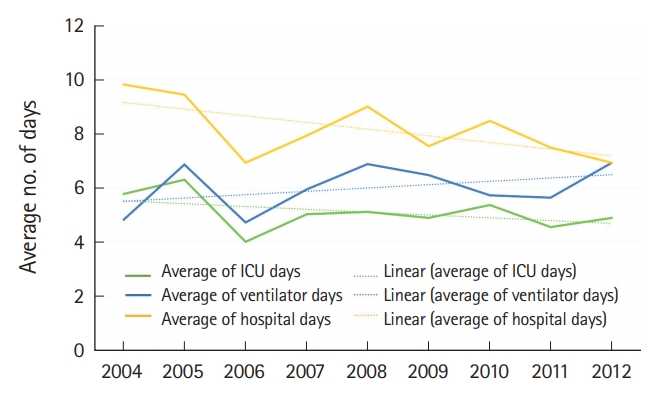
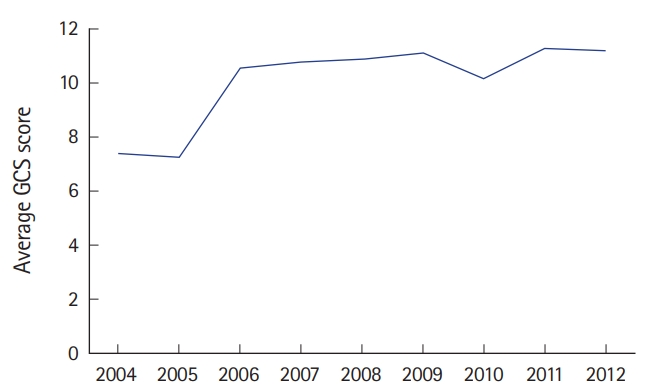
A total of 3,039 patients with TBI were treated over the study period. TBI was defined as having an International Classification of Diseases 9th revision diagnosis code under the category of intracranial injury and/or skull fracture. Based on the Glasgow Coma Scale, 1,663 (55%) of the patients with TBI were classified as mild, 219 (7%) were moderate, 1,100 (36%) were severe, and 57 (2%) of the patients did not receive scores (Fig. 1). The patients’ ages ranged from less than 1 month to 109 years of age. The mean age of the study sample was 43 years (standard deviation, 24) and the median age was 41 (interquartile range, 23 to 60) (Fig. 2). Three peaks in age can be visualized in this histogram (Fig. 2), including young adult, middle aged, and elderly. Age increased steadily throughout the study period, with a mean age of 32 years in 2004 and a mean of 49 years in 2012. Overall mortality was 21%. Patient mortality decreased over the entire period (odds ratio [OR], 0.88; 95% confidence interval [CI], 0.85 to 0.91) (Fig. 3). Ventilator days, intensive care unit days, and hospital admission days did not show a significant change over time (Fig. 4). Glasgow Coma Scale scores, after the first 2 years, remained stable over time (Fig. 5).
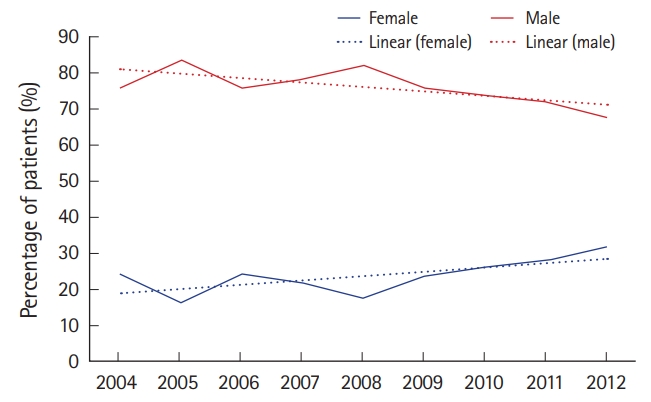
Twenty-five percent of the patients in the study period were female. The percentage of female TBI patients increased throughout the study period, from 16.4% initially, to 27.5% over the last 4 years (Fig. 6). In addition, a greater decrease in mortality was seen in females (OR, 0.84; 95% CI, 0.78 to 0.90) than in males (OR, 0.90; 95% CI, 0.86 to 0.94) (Fig. 7).
DISCUSSION
From 2004 to 2012, the average age of patients treated for TBI at our Level 1 Trauma Center increased over time, which was accompanied by an increased percentage of female sex. Despite these temporal trends, mortality improved for both sexes, with a greater improvement for females. These changes in trends and outcomes of TBI in the IDPH Trauma Registry support the importance of analyzing other databases to identify areas for further study.
Given the aging patient population and likelihood of comorbidities, one may expect that an increase in mortality would be concurrently seen. However, unexpectedly, the overall percent mortality decreased over time. This could be due to many factors, including a decrease in severity of injury presentation or an improvement of patient care; however, based on Glasgow Coma Scale score, our population injury severity appeared to have remained relatively stable over the majority of our period of analysis. A possible unmeasured decrease in injury severity at presentation, due to factors such as improved pre-hospital care or change in safety rules/public awareness, may account for these findings. Emergency medical services and pre-hospital treatment, as well as in-hospital treatment and rehabilitation, continues to improve, which provides better outcomes for TBI [11,12].
Illinois does not currently implement a helmet law for motorcyclists and there were no changes in helmet laws during the study period. However, some changes to legislature regarding seatbelt laws in Illinois were implemented. In 2003, Illinois implemented a primary seatbelt law, allowing police to pull over motorists to ticket them for not wearing a seatbelt. On January 1, 2012, all backseat passengers in Illinois were required to wear a seatbelt, not just those under 19 years of age as was previously mandated. A decrease in mortality may also be due to improved in-hospital care. However, the lack of a substantial decrease in intensive care unit, hospital, and ventilator days with the change in mortality may suggest that there is no significant change in severity of injury or hospital management of these patients.
Regarding sex differences in mortality, there has been some speculation that progesterone may be protective in acute brain injury. A recent study involving mice found that females treated with sex steroids (progesterone and estrogen) showed a decreased sensitivity to TBI compared to male and female mice that lack the sex steroids [13]. However, recent clinical investigations have concluded that the administration of progesterone did not decrease mortality in patients presenting with TBI [14]. Other investigators have proposed multiple factors that may contribute to the negative results in clinical trials such as the overall complexity in the pathophysiology of TBI, pre-existing conditions, and the difficulty in controlling for other confounding variables compared to animal models [15,16]. A third factor proposed is suboptimal dosing parameters from pre-clinical trials which may have led to too high a drug dose over too short of an administration period during the clinical investigation [17]. Due to these factors, further research is required to understand the potential role progesterone has on both the outcome and treatment of TBI.
The overall quality of research on traumatic brain injuries is dictated by the reliability of the datasets that the researchers choose to use. Prior studies on TBI rely on large public datasets that have recently shown limitations in data reliability. Without reliable data, studies on the topic of TBI runs an increased risk of poorly representing the broader scope of the injury as well as the individuals affected by it. When this occurs, the progress in identifying and treating traumatic brain injuries is slowed. Analyzing databases such as the IDPH Trauma Registry has shown to be beneficial in understanding the trends and demographics of TBI. It is for this reason that researchers should place emphasis on datasets that incorporate rigorous training methods to minimize the amount of discrepancies and produce the most accurate data possible. Applying the use of these datasets can be beneficial in determining whether the changes in epidemiology of TBI found in this study are congruent with rates at the state and national level.
This study has the inherent limitations associated with retrospective database review. In addition, this analysis, as is common with many analyses of TBI, does not sub-categorize type of TBI. International Classification of Diseases 9th revision codes are non-specific, which includes a variety of codes such as ‘cortex contusion’ to ‘subdural hemorrhage’ to ‘skull fracture.’ It also does not stratify by cause of death, nor does it distinguish among various levels of neurological outcomes.
Although the age of patients presenting with TBI is increasing substantially, the data suggests that overall percent mortality appears to be decreasing, and this decrease appears greater in females than in males. These trends in demographics and outcomes of TBI found in the IDPH Trauma Registry supports the importance for further analysis of other reliable public datasets to identify areas of future study.