AbstractObjectiveFew studies have prospectively evaluated the diagnostic accuracy and temporal impact of ultrasound in the emergency department (ED) in a randomized manner. In this study, we aimed to perform a randomized, standard therapy controlled evaluation of the diagnostic accuracy and temporal impact of a standardized ultrasound strategy, versus standard care, in patients presenting to the ED with acute dyspnea.
MethodsThe patients underwent a standardized ultrasound examination that was blinded to the team caring for the patient. Ultrasound results remained blinded in patients randomized to the treating team but were unblinded in the interventional cohort. Scans were performed by trained emergency physicians. The gold standard diagnosis (GSDx) was determined by two physicians blinded to the ultrasound results. The same two physicians reviewed all data >30 days after the index visit.
ResultsFifty-nine randomized patients were enrolled. The mean±standard deviation age was 54.4±11 years, and 37 (62%) were male. The most common GSDx was acute heart failure with reduced ejection fraction in 13 (28.3%) patients and airway diseases such as acute exacerbation of asthma or chronic obstructive pulmonary disease in 10 (21.7%). ED diagnostic accuracy, as compared to the GSDx, was 76% in the ultrasound cohort and 79% in the standard care cohort (P=0.796). Compared with the standard care cohort, the final diagnosis was obtained much faster in the ultrasound cohort (mean±standard deviation: 12±3.2 minutes vs. 270 minutes, P<0.001).
INTRODUCTIONDyspnea is an abnormally uncomfortable awareness of breathing [1]. In 2014, dyspnea was the cause of 3.4 million emergency department (ED) admissions and accounted for 2.4% of total ED visits in the United States [2]. In patients aged older than 65 years, dyspnea is the third most common cause for ED admissions in the United States. Acute dyspnea is associated with many pathologies and is thus a challenge for the emergency physician. Differentiating between its causes may be difficult, particularly in elderly patients with multiple comorbidities. The most common pathologic causes of dyspnea include heart failure, chronic obstructive pulmonary disease (COPD), and pneumonia. However, there are several other causes of dyspnea that can be fatal, and these may require special diagnostic modalities that are potentially complicated, expensive, and invasive. Moreover, other pathologies of dyspnea require high-risk treatment regimens.
A rapid and accurate diagnosis is tantamount to early determination of appropriate intervention. Numerous studies have demonstrated an increased short-term mortality risk when appropriate interventions are delayed, which may occur when diagnosis is deferred [3-5]. Further, large studies have shown increased mortality when treatment is delayed as this also results in prolonged ED stay [6,7]. However, there is no single historical, physical examination, electrocardiographic (ECG) or radiographic finding that can accurately and independently diagnose the pathologic cause in patients presenting with dyspnea [8].
Because ultrasound allows for rapid, inexpensive, and non-invasive assessment of many different organs, it may be valuable in ED patients with acute dyspnea [9]. Further, it may have unique diagnostic characteristics that cannot be obtained by other standard ED investigations in patients presenting with acute dyspnea. Ultrasound can be used to evaluate the potential for interstitial lung fluid as it can detect B-lines, which have a high diagnostic accuracy for distinguishing acute dyspnea of cardiac etiology from that related to pulmonary diseases (e.g., COPD) [10]. Although B-lines are not specific for cardiogenic pulmonary edema and can be seen in other respiratory disorders such as acute lung injury and acute respiratory distress syndrome [11], their presence combined with other parameters, i.e., left ventricular (LV) systolic function [12] and collapsibility of inferior vena cava (IVC), may help identify abnormal volume states (e.g., sepsis, dehydration, hemorrhage, or heart failure) [13].
However, few studies have evaluated the diagnostic accuracy and temporal impact of ED ultrasound in a randomized blinded manner in patients presenting with acute dyspnea. This study aimed to determine the diagnostic accuracy and temporal impact of ultrasound in patients with acute dyspnea admitted to the ED compared with standard therapy. Moreover, we also aimed to determine and compare the time required to obtain an accurate diagnosis in patients randomized to a standardized ultrasound strategy and standard care.
METHODSTrial designThis was a parallel, block randomized, standard therapy controlled, blinded evaluation of a point-of-care ultrasound strategy in adult ED patients presenting with a chief complaint of shortness of breath. The trial was approved by the institutional ethics committee (H-38431) and used a convenience sampling method (when the ultrasonographers were available) for patient enrollment. The patient’s allocation ratio was 1:1, and no changes to the methods were made after the start of the trial.
ParticipantsThis study was conducted at a large urban public hospital ED with an annual census of >100,000. We enrolled patients from March 2016 to April 2017. All patients were followed up during their ED stay. The medical records were reviewed 30 days after the index visit to determine the final diagnosis.
Patients were enrolled if they met the following inclusion criteria: age >18 years and shortness of breath of at least moderate severity as determined according to the modified Borg dyspnea scale [14] and a 100-point visual analogue scale (VAS) (Figs. 1, 2). Patients were excluded if they had ECG changes consistent with ST segment elevation indicative of myocardial infarction, a Modified Borg Scale >8, or the treating physician had already received the results of non-ECG diagnostic test (i.e., lab or chest radiography findings), thereby disrupting blinding.
Trial interventionBlinded ultrasounds were performed as soon as possible after ED arrival once informed consent was obtained. The patients were then randomized according to whether their treating team was unblinded (group A) or not (group B) to their ultrasound results. All patients received standard care. The study flow is presented in Fig. 3. Time zero was defined as the time the patient was placed in an ED examination room.
Ultrasound scanning was performed by trained ED physicians. Scanners were blinded to the patient’s medical history and were not allowed to be involved in any diagnostic or therapeutic patient care discussions.
In the unblinded ultrasound cohort (group A), before unblinding the ultrasound results, the primary physician was asked to document their primary diagnosis and their diagnostic certainty using a 10-cm VAS (Fig. 4). Ultrasonographers were also asked to provide a primary diagnosis and diagnostic certainty (group C) (Fig. 3). To evaluate diagnostic change as a function of ultrasound results, diagnostic certainty was reported a second time by the primary physician 10 minutes after receiving the ultrasound results, in the unblinded cohort (Fig. 4).
Standardized ultrasound procedureUltrasound scanning was performed by one of four emergency medicine physicians, each with at least 2 years of practice experience, and all of whom had completed an ultrasound fellowship. All patients were evaluated using a phased array probe, with a range of 1 to 3 MHz (Edge; SonoSite, Bothell, WA, USA). The required standardized ultrasound approach included echocardiography, an IVC evaluation, and a lung exam.
Cardiac ultrasound was performed with visual assessment of the global LV systolic function from as many views as possible. The ratio between the right and left ventricles was visually assessed and then recorded. Pericardial effusions, LV hypertrophy, or any other observed cardiac pathology were also recorded.
Bilateral scanning of the anterior, lateral, and posterior chest walls was performed with the patient in the supine or sitting position (Fig. 5) [15]. The chest wall was divided into three zones: anterior (from the parasternal line to anterior axillary line), lateral (from the anterior axillary line to the posterior axillary line), and posterior (posterior axillary line to the paravertebral line). Each zone was then further divided into upper and lower areas. This resulted in a total of 12 areas scanned for each patient. The investigator recorded the presence of A and B lines, pleural effusions, hepatization, air bronchogram, or any other noted lung pathology.
The IVC was evaluated within 2.0 cm of the IVC-right atrium junction. The IVC diameter was expressed as no respiratory variation, minimum respiratory variation (<50% collapse of the IVC diameter), or significant respiratory variation (>50% collapse of the IVC diameter). Ultrasound diagnoses were ultimately defined according to the following criteria [16]:
Heart failure with preserved ejection fraction (HFrEF) with pulmonary edema: Lung scan would show diffuse interstitial pattern (or diffuse B-pattern, >3 B-lines in a rib space in at least 2 among 4 anterolateral areas of each hemithorax bilaterally.
HFrEF with pulmonary edema: Lung scan would show diffuse interstitial pattern (or diffuse B-pattern, >3 B-lines in a rib space in at least 2 among 4 anterolateral areas of each hemithorax. Cardiac scan: reduced EF on visual assessment of the global LV systolic function. IVC scan would show minimum respiratory variation during inspiration (<50%).
Airway diseases diagnosis is made by exclusion, if nothing was found on the ultrasound scan, AND includes asthma and chronic obstructive pulmonary disease.
Pneumonia is diagnosed by absence of lung sliding with B-lines, consolidation, OR focal interstitial pattern.
Pleural effusion is diagnosed by the presence of anechoic or black fluid collection between the visceral and parietal pleura in a dependent pattern.
Pericardial effusion is diagnosed by the presence of anechoic or black fluid collection in the pericardial cavity, usually best visualized in the subcostal view.
Pneumothorax is diagnosed by absence of lung sliding, the presence of a “lung point” or a “transition point” (defined as the presence of normal lung sliding and no lung sliding at the pneumothorax border).
Gold standard diagnosisThe gold standard diagnosis was determined by two independent emergency physician reviewers who were not involved in the study or patient care and blinded to all ultrasound results and to each physician’s diagnosis. They reviewed all available clinical data at least 30 days after the index ED visit. The final gold standard diagnosis was defined as both reviewers having the same diagnosis. In cases where the reviewers had different diagnoses that persisted after discussion, a third physician, blinded to all study ultrasound data, resolved the disagreement.
Statistical analysisAs this was an observational study, no pre-specified power analysis was performed. Patients were randomized using a 4-subject block randomization scheme. The ultrasonographer determined the group allocation by opening a single sequentially numbered opaque envelope containing the randomization result. In 50% of the patients, the treating physician was aware of the ultrasound results, while in the other 50%, the ultrasound results remained blinded. Data were analyzed with descriptive statistics using Stata ver. 14 (StataCorp., College Station, TX, USA). The sensitivity, specificity, accuracy, positive predictive value, and negative predictive value of the standardized ultrasound strategy for an accurate gold standard diagnosis of dyspnea is presented. Statistical analyses were performed with z-test. Times of diagnosis, treatment, and disposition decision were presented as mean±standard deviation, and Student t test and chi-square test was used for continuous and categorical data analysis.
RESULTSPatient characteristicsOf the 60 patients enrolled, one left against medical advice before the final diagnosis was made. Thus, 59 patients were randomized to the standard of care cohort (ultrasound data remained blinded, n=30) and unblinded ultrasound cohort (n=29). The mean±standard deviation age was 54.4±11 years, and 37 (62%) were male. Racial distribution was 31 (51.5%) African Americans, 24 (40%) White, 2 (3.4%) Asians, 2 (3.4%) Indians, and 1.7% other races. Patients were enrolled by 12 emergency physician faculty and 16 residents with different levels of experience. The patients’ demographic data are presented in Table 1. There were no significant differences between the blinded ultrasound control and the unblinded ultrasound cohorts. The median (interquartile range, IQR) time from ED arrival to bed placement was 23.5 (7.25 to 47.5) minutes, with randomization occurring at 79 (49 to 122) minutes. The 55.5-minute time from bed placement to randomization was a consequence of obtaining informed consent.
DiagnosesThe median (IQR) time from randomization to ED diagnosis was 21 (10 to 15) minutes for unblinded ultrasound patients versus 244 (128 to 360) minutes for standard of care blinded ultrasound group (P<0.001) (Table 2). The final adjudicated diagnoses and ED disposition are listed in Table 3. Overall, HFrEF and “other” diagnoses accounted for almost 50% of diagnoses in the enrolled patients (23.8% for each), followed by airway diseases (asthma/COPD), non-specific chest pain, and pneumonia. Patients had high rates of severe illness, as reflected by high rates of intensive care unit admission. A total of 60% of patients with pneumonia, 36% of patients with heart failure, and nearly 20% of patients with airway diseases were admitted to the intensive care unit, respectively.
Diagnostic accuracyDiagnostic accuracy in both unblinded and blinded ultrasound physician with access to clinical information (groups A and B, respectively) was 76% (Table 4). This was similar to the diagnostic accuracy (79%) of group C (the ultrasonographers without clinical information) (P>0.796). When stratified by diagnosis, accuracy was similar across all groups, and was similar for the specific diagnoses of heart failure and airway disease. While both the unblinded and blinded ultrasound groups had similar diagnostic performance for HFrEF, both missed 2 cases. Finally, while the unblinded standardized ultrasound strategy had a higher sensitivity than standard care for pneumonia, it had lower specificity and positive predictive value.
Diagnostic certainty is crucial to a physician’s ability to initiate treatment. Unblinding of the ultrasound results had minimal effect on diagnostic certainty, planned therapy, or disposition decision. In the standardized ultrasound strategy cohort, initial diagnostic certainty was 73% (95% confidence interval [CI], 65% to 82%) and increased to 78% (95% CI, 67% to 87%) (P=0.559) after un-blinding. Only 8 physicians changed their level of certainty; 7 became more confident and 1 became less certain of their diagnosis. Additionally, unblinding of ultrasound results did not change the planned disposition; only 1 physician changed their disposition with unblinding (from home to admission). Finally, although group A was unblinded to the ultrasound results, no physician changed their management plan. They preferred to use the standard of care to reach the diagnoses; therefore, there were no significant differences between group A and group B regarding time to diagnosis or ED length of stay. Overall, no harms or unintended effects occurred in any subgroup.
Despite being blinded to the patients’ history and physical exam findings, ultrasonographers were asked to document their diagnoses. Evaluation of the entire sample found that the ultrasonographers (group C) had higher diagnostic certainty after scan completion than the treatment team (groups A and B) before the ultrasound results were known (82% [95% CI, 77 to 87] vs. 74% [95% CI, 69% to 79%], P=0.018).
Overall, the median (IQR) ED length of stay was 8.0 (6 to 11) hours, during which dyspnea severity was evaluated hourly with the VAS and modified Borg scale. In general, dyspnea severity improved during the patient’s ED stay. The median (IQR) VAS severity of dyspnea at the time of enrollment was 75 (50 to 80), improving to 50 (40 to 60) over 4 hours (P<0.001).
DISCUSSIONIn this study, the use of a standardized ultrasound strategy resulted in more rapid, but equally accurate diagnoses, as compared to standard of care in ED patients presenting with acute dyspnea. This finding has operational implications in busy EDs and may allow potential outcome improvements in patients with high severity of illness where diagnostic delays may be associated with worse outcomes. The time to obtain a correct ED diagnosis is important. In a study of 14,900 heart failure patients admitted to the ED [3], delayed furosemide administration was associated with increased mortality. In another study of 35,000 heart failure patients admitted to the ED [4], delayed vasoactive treatment was associated with increased rates of acute death. Our findings that ultrasound allows for a more rapid HFrEF diagnosis in ED patients presenting with dyspnea indicates that our standardized ED ultrasound strategy could improve HFrEF outcomes.
Our study has a number of unique features, the most important of which is that we investigated the diagnostic accuracy and operational efficiency of ultrasound and its impact in the ED through a single evaluation. First, we validated the accuracy of our standardized ultrasound strategy versus standard care and demonstrated equal performance between the two. Second, as the physicians performing the ultrasound were blinded to the patients’ history and physical exam findings, we could determine the independent contribution of performing the ultrasound to diagnostic certainty. Third, by timing the interval to diagnostic results, we quantified the time saved from the standardized ultrasound strategy as compared to that in standard care. Unlike other studies [16-19] that evaluated various parts of our approach, our finding of a 4.5-hour earlier time to accurate result is likely to have important operational and clinical outcome relevance in the ED.
Others have reported subsets of our study. Gallard et al. [17] demonstrated a mean±standard deviation time to complete a cardiopulmonary ultrasound of 12±3 minutes, which was similar to our median (IQR) time of 12 (3 to 18) minutes. However, they did not perform an IVC exam and did not include data regarding time for standard of care diagnosis. Another study by Zanobetti et al. [18] used ultrasound and standard care reporting similar to our investigation, e.g., lung, cardiac, and IVC ultrasound, but without blinding. They reported similar mean±standard deviation times of 24± 10 and 186±72 minutes for ultrasound and standard of care diagnostic time, respectively. Finally, both Mantuani et al. [19] and Papanagnou et al. [20] found that the most common final diagnoses in patients presenting to the ED with acute dyspnea were heart failure, airway disease, and pneumonia, which is similar to our findings.
In our analysis, the overall diagnostic accuracy of the standardized ultrasound strategy was similar to standard care (76% vs. 78%, P=0.796). Meanwhile, other studies have reported diagnostic superiority for this type of strategy. The SEARCH8Es protocol reported an accuracy of 90.1% and superiority over standard care (P<0.001) [21]. Importantly, their ultrasonographers were not blinded to patient data, the points of their scans varied based on their differential diagnosis, and their post-scan diagnosis was chosen from a list limited to 13 options.
Compared with standard care, our standardized ultrasound approach was more sensitive (83 vs. 66%) for diagnosing pneumonia, but it had lower specificity (75.9 vs. 98.1). Others have reported similar results. In a meta-analysis of 1,551 patients, Long et al. [22] reported an ultrasound sensitivity of 88% (95% CI, 0.86 to 0.90), with a higher specificity (86%; 95% CI, 0.83 to 0.88) than our analysis. This may be because we did not define sonographic criteria for pneumonia, which allowed for more diagnostic variation.
Finally, our study found a high sensitivity of 90.9% (95% CI, 83.5% to 98%) for diagnosing airway disease, which was similar to standard care. Prior studies have shown lower sensitivities. The SEARCH8Es reported the sensitivity of ultrasound to be as low as 76.5% in patients with airway disease and sepsis [21]. The reasons for their less than expected performance may be explained by their relatively small number of patients with airway disease or sepsis (n=30) and that airway diseases, such as asthma or COPD, may require more extensive lung evaluations than those that were mandated by their protocol. In our study, there were four false-positive cases of posterolateral alveolar/pleural syndrome in patients with COPD; these patients were ultimately found to have no pneumonia. This finding was comparable to that of SEARCH8Es, in which three patients with airway disease were identified to have normal lung patterns but subsequently found to have abnormal pulmonary functions after admission.
We found that our standardized ultrasound strategy did not significantly change the physician’s diagnosis, although we observed a modest increase in their diagnostic confidence. This finding is in contrast to that of Papanagnou et al. [20] who reported a moderate increase in diagnostic confidence and some changes in management. Consistent with the lack of a change in diagnosis, we found that un-blinding the ultrasound data did not change therapy or disposition decisions. This may be a function of a lack of confidence in the ultrasonographic findings as reported to the treating team with unblinding. Interestingly, ultrasonographers demonstrated considerably higher levels of diagnostic certainty despite being blinded to the clinical scenario.
Our study has several limitations. These include its small sample size and single-center enrollment that may have restricted some of our findings. Our study did not include patients with severe dyspnea (defined as a Borg dyspnea score >8) as this group is unable to provide informed consent. This may limit the generalizability of our results to the population studied. However, our findings can be a basis for future studies to include a more severely dyspneic cohort. We also enlisted only fellowship trained ultrasonographers, whose skill sets may not be duplicated elsewhere. Additionally, our convenience sampling design, with enrollment occurring when the investigator and the ultrasonographers were in the ED simultaneously, may have resulted in unmeasured bias. Finally, there was no pre-specified agreement on the pneumonia diagnostic criteria, which may have decreased the sensitivity of the ultrasound data.
In conclusion, compared to standard of care, a standardized ultrasound strategy is diagnostically as accurate, but provides much earlier diagnosis, saving more than 4.3 hours in the evaluation of patients presenting to the ED with acute dyspnea.
REFERENCES1. Mann D, Zipes D, Libby P, Bonow R. Braunwald’s heart disease: a textbook of cardiovascular medicine. 10th ed. Philadelphia, PA: Elsevier Saunders; 2015.
2. National Center for Health Statistics. National Hospital Ambulatory Medical Care Survey: 2014 emergency department summary tables. Atlanta, GA: Centers of Disease Control Prevention; 2014.
3. Maisel AS, Peacock WF, McMullin N, et al. Timing of immunoreactive B-type natriuretic peptide levels and treatment delay in acute decompensated heart failure: an ADHERE (Acute Decompensated Heart Failure National Registry) analysis. J Am Coll Cardiol 2008; 52:534-40.
4. Peacock WF, Emerman C, Costanzo MR, Diercks DB, Lopatin M, Fonarow GC. Early vasoactive drugs improve heart failure outcomes. Congest Heart Fail 2009; 15:256-64.
5. Wong YW, Fonarow GC, Mi X, et al. Early intravenous heart failure therapy and outcomes among older patients hospitalized for acute decompensated heart failure: findings from the Acute Decompensated Heart Failure Registry Emergency Module (ADHERE-EM). Am Heart J 2013; 166:349-56.
6. Guttmann A, Schull MJ, Vermeulen MJ, Stukel TA. Association between waiting times and short term mortality and hospital admission after departure from emergency department: population based cohort study from Ontario, Canada. BMJ 2011; 342:d2983.
7. Sprivulis PC, Da Silva JA, Jacobs IG, Frazer AR, Jelinek GA. The association between hospital overcrowding and mortality among patients admitted via Western Australian emergency departments. Med J Aust 2006; 184:208-12.
8. Martindale JL, Wakai A, Collins SP, et al. Diagnosing acute heart failure in the emergency department: a systematic review and meta-analysis. Acad Emerg Med 2016; 23:223-42.
9. Ultrasound guidelines: emergency, point-of-care and clinical ultrasound guidelines in medicine. Ann Emerg Me 2017; 69:e27-54.
10. Ang SH, Andrus P. Lung ultrasound in the management of acute decompensated heart failure. Curr Cardiol Rev 2012; 8:123-36.
11. Liteplo AS, Marill KA, Villen T, et al. Emergency thoracic ultrasound in the differentiation of the etiology of shortness of breath (ETUDES): sonographic B-lines and N-terminal pro-brain-type natriuretic peptide in diagnosing congestive heart failure. Acad Emerg Med 2009; 16:201-10.
12. Kajimoto K, Madeen K, Nakayama T, Tsudo H, Kuroda T, Abe T. Rapid evaluation by lung-cardiac-inferior vena cava (LCI) integrated ultrasound for differentiating heart failure from pulmonary disease as the cause of acute dyspnea in the emergency setting. Cardiovasc Ultrasound 2012; 10:49.
13. Frank Peacock W, Soto KM. Current technique of fluid status assessment. Congest Heart Fail 2010; 16 Suppl 1:S45-51.
14. Crisafulli E, Clini EM. Measures of dyspnea in pulmonary rehabilitation. Multidiscip Respir Med 2010; 5:202-10.
15. Volpicelli G, Mussa A, Garofalo G, et al. Bedside lung ultrasound in the assessment of alveolar-interstitial syndrome. Am J Emerg Med 2006; 24:689-96.
16. Volpicelli G, Elbarbary M, Blaivas M, et al. International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med 2012; 38:577-91.
17. Gallard E, Redonnet JP, Bourcier JE, et al. Diagnostic performance of cardiopulmonary ultrasound performed by the emergency physician in the management of acute dyspnea. Am J Emerg Med 2015; 33:352-8.
18. Zanobetti M, Scorpiniti M, Gigli C, et al. Point-of-care ultrasonography for evaluation of acute dyspnea in the ED. Chest 2017; 151:1295-301.
19. Mantuani D, Frazee BW, Fahimi J, Nagdev A. Point-of-care multi-organ ultrasound improves diagnostic accuracy in adults presenting to the emergency department with acute dyspnea. West J Emerg Med 2016; 17:46-53.
20. Papanagnou D, Secko M, Gullett J, Stone M, Zehtabchi S. Clinician-performed bedside ultrasound in improving diagnostic accuracy in patients presenting to the ED with acute dyspnea. West J Emerg Med 2017; 18:382-9.
Fig. 1.Modified Borg dyspnea scale. Severity of dyspnea reported by the patient by selecting a number or face. Every patient presented with shortness of breath in emergency department was asked to report the severity of his/her symptoms by pointing at the face and/or the number resembling their condition. The investigator recorded the number every hour during the patient stay in the emergency department. 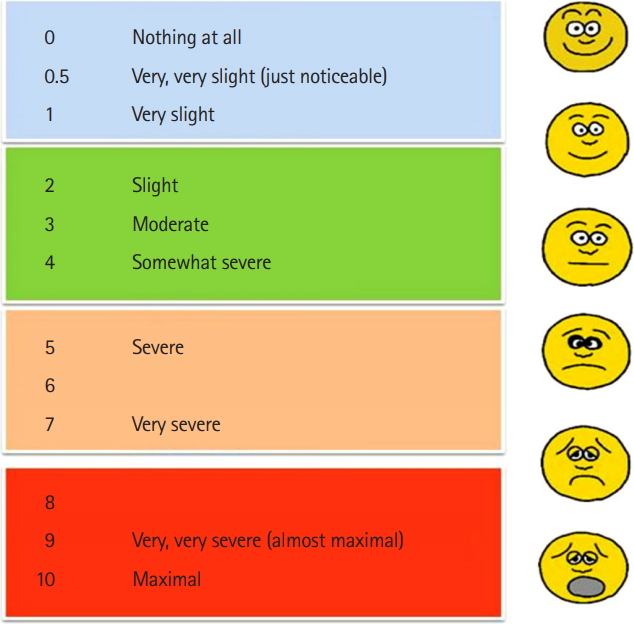
Fig. 2.Visual analogue scale. Severity of dyspnea reported by the patient by indicating with a vertical line. Every patient was enrolled in our study was asked to rate their shortness of breath severity by choosing a number. Zero was having no shortness of breath at all. One hundred was the worst dyspnea to experience by the patient. We recorded the numbers every hour during the patients’ stay in the emergency department. 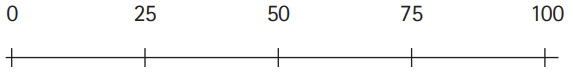
Fig. 3.Study flow chart and participating physicians. A, intervention team physicians; B, standard care team physicians; C, sonographers; D, reviewers; ED, emergency department; GSDX, gold standard diagnosis. 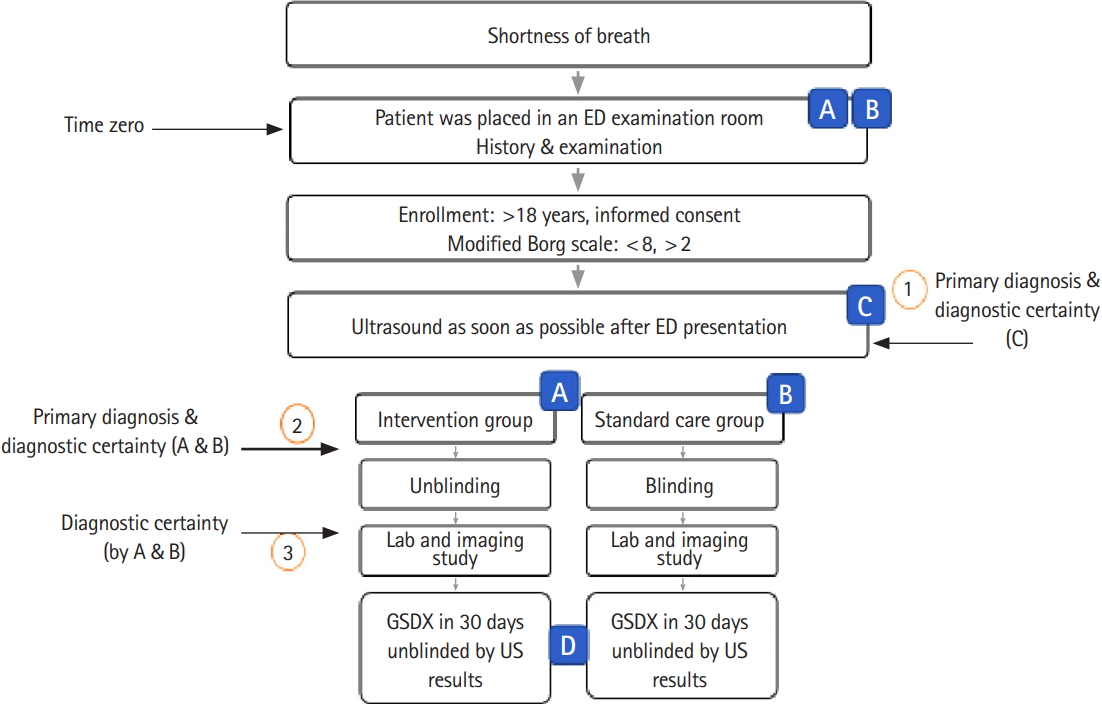
Fig. 4.Visual analogue scale (10 cm) for reporting diagnostic certainty. The treating physicians was asked to report their certainty of the diagnosis before and after knowing the ultrasound results. As zero was not certain at all, and 100 was absolutely sure. The ultrasound team who was blinded by the patient history or physical exam was asked to report their certainty after the scan. 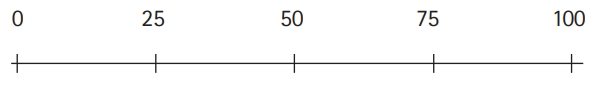
Fig. 5.Zones for ultrasound evaluation of the lungs. (A) The hemithorax is divided into the anterior and lateral parts, and each part was further divided into the upper and lower areas based on the study by Volpicelli et al.[15] (B) The posterior chest wall is divided into the upper and lower parts. A total of 12 areas were scanned were for each patient. AA, anterior axillary line; AP, posterior axillary line. Consents were taken from the patients to use their photos. 
Table 1.Demographic and presentation data, stratified by study cohorts Table 2.Time from order to results for emergency department investigations Table 3.Gold standard diagnoses and emergency department disposition
Table 4.The accuracy of ultrasound diagnosis (group C) versus ED diagnosis (group A and B)
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||