INTRODUCTION
Bystander knowledge of basic life support (BLS) is essential for improving the survival rate of sudden cardiac arrest [1,2]. Around 15% of bystanders in Thailand perform BLS upon encountering a collapsed patient [3]. In many countries, such as USA [4] and Norway [5], BLS is a compulsory part of school education. Evidence supports that teaching BLS in primary school improves the skill and knowledge of students [6-9]. However, there are no previous studies showing the benefit of teaching BLS as part of the compulsory curriculum in South East Asian schools, especially in primary education. The potential of children to learn BLS may drive policies to establish cardiopulmonary resuscitation (CPR) teaching starting from the primary schools. Hence, this study aims to report the influence of BLS courses on the knowledge, attitudes, and life support skills of primary school students; it also aims to improve certain aspects of medical professionalism among medical students acting as instructors.
METHODS
This experimental study was performed at Ban Rim Tai School, a rural primary school consisting of 1,057 students, in Chiang Mai Province. The protocol was approved by the Institutional Ethical Committee of the Faculty of Medicine, Chiang Mai University (EME-2560-04799). No informed consent was required as this study was waved for educational purpose. The BLS course was conducted by first-year medical students who had previously completed BLS provider and instructor courses. A curriculum was prepared for upper primary school students using the learn-and-play concept. This was performed by creating cartoon characters to promote child learning, and by utilizing simulation techniques in both skills and test stations. The 3.5-hour modified BLS course emphasized adult chest compression-only CPR and the use of automated external defibrillator which was taught both theoretically and practically. This course was modified from a standard 4-hour BLS provider course, which is the conventional BLS course in Thailand provided by the Thai Resuscitation Council. However, this course was different from the standard course due to its exclusion of courses on rescue breathing and foreign body aspiration. The courses and tests were designed by medical students, senior BLS instructors, and specialists in primary school education. Each course was closely monitored, controlled, and advised by experienced instructors who were doctors and nurses. Students in grades 4 and 5 participated in this course with the ratio of trainee-to-trainer of 6ŌĆō7:1. Four courses were conducted in the school gymnasium. The pretest and posttests, each consisting of 14 four-multiple choice questions (Supplement 1), were taken by both students and school teachers before and immediately after the teaching sessions. However, the skill and attitude tests were performed only by primary school students immediately after the teaching sessions. The skill test of one-rescuer CPR and automated external defibrillator was conducted by a medical student instructor using a standard checklist to evaluate the steps and quality of CPR (Supplement 2). Additionally, the attitude was evaluated using a 5-point Likert scale asking 11 questions. The instructors also answered a questionnaire before and after teaching the BLS course using a 5-point Likert scale. Three questions were asked regarding the following components: 1) understanding rationale, steps, and methods of BLS, 2) confidence in performing BLS, and 3) confidence in teaching BLS.
Data are presented as percent, mean and standard deviation. Statistical analysis was performed using IBM SPSS Statistics ver. 21.0 (IBM Corp., Armonk, NY, USA). Score comparisons were performed using Student t-test, and P<0.01 was considered statistically significant.
RESULTS
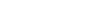
Three hundred and thirteen students and 23 teachers participated in this course. This included 166 grade 5 students (53.0%) and the remainder who were in grade 4. The average age of students in grade 4 and grade 5 was 9.4 and 10.7 years, respectively. The studentsŌĆÖ and teachersŌĆÖ knowledge regarding BLS significantly increased at the end of training. Although the students had lower mean scores than the teachers in both the pretest (5.74 vs. 9.23, P<0.01) and posttests (9.43 vs.12.29, P<0.01) results (Fig. 1), the difference between the two groups in terms of pretest and posttest scores was the same (3.05 vs. 3.678, P=0.33) (Table 1). Additionally, almost all the essential CPR skills were performed correctly by the students, except for ŌĆśscene safetyŌĆÖ and ŌĆśclear patient for shockŌĆÖ procedures (Table 2). At the end of the training, most of the students believed that BLS was essential, and that they could correctly perform BLS and provide bystander assistance to victims who collapse (Table 3).
Fifteen of the 23 medical students who were instructors of the BLS course answered the questionnaire, and responded that they had significantly increased their understanding of BLS (P<0.01), confidence in performing BLS (P<0.01), and confidence in teaching BLS (P<0.01) (Fig. 2).
DISCUSSION
Our data demonstrated that a BLS course consisting of lecture and practice components can improve primary school studentsŌĆÖ knowledge, while enhancing their skills and attitude towards CPR. Despite children having less strength than adults, they have the required psychomotor skills and are able to perform BLS after practice sessions. This correlated with many studies in Europe [7,8,10] and Australia [9], supporting that BLS and first-aid training can help develop the skill and knowledge of life support in children. Moreover, this may cultivate childrenŌĆÖs confidence to help other victims. Although the teachers had higher pretest and posttest scores than students, the knowledge improvement of primary school students was not different from that of adults. This may be attributed to students having less experience than teachers, although the students had equal ability in learning BLS. This result correlated with a study in Hungary that showed that the age group was correlated with learning BLS [6]. However, the sense of safety awareness among upper primary school students was inadequate, and this was reflected in students forgetting to perform safety awareness before helping and ŌĆ£clearing-before-shockingŌĆ£. This defect of learning can be corrected by repeated learning of BLS in secondary school. Furthermore, most students correctly performed skill maneuvers, as they had physical strength; nonetheless, scene safety must be emphasized more because students were least concerned about scene safety.
From the learning pyramid, teaching others is the best way to gain a better understanding and knowledge on a subject. Medical students learned from this teaching process and consequently gained more confidence to perform BLS by themselves. Another study also showed improvement of resuscitation and teaching skills in medical students after teaching others [11]. These skills are essential for medical professionals in the future. This study not only improved their knowledge and confidence to perform and teach BLS, but it also emphasized the importance of public health education to medical students.
This study had some limitations. First, this was a small study from one rural school. However, compulsory education in Thailand has the same curricula in all schools; hence, the data may be representative of primary school students in Thailand. Second, we did not collect baseline characteristics or factors associated with BLS knowledge of the students and school teachers such as gender, body mass index, education, previous BLS knowledge, or previous health education. Third, the students did not have a pretest of skills and attitudes, but almost all the students had no prior knowledge about BLS, as shown in the pretest. Additionally, the adapted multiple questions from the standard course were not validated by a standard method, and no subsequent reviews of the course were made to evaluate the skills and knowledge of the participants. Therefore, future studies should aim to review the knowledge retention of participants. Finally, the medical students were not assessed with a questionnaire before the course began, and this may contribute some bias to rating scale questions.
In conclusion, primary school students have the potential to learn BLS by using a simulation-based approach; the training improves their attitude and provides them with knowledge and crucial skill sets, which improves their confidence in performing BLS.