INTRODUCTION
According to a recent study, official development assistance (ODA) projects in the healthcare sector of underdeveloped countries are undergoing significant changes [1,2]. The focus of the current strategy is on controlling infectious diseases, but it is shifting to improving the emergency medical system for life-threatening diseases and injuries, as well as the emergency management abilities and education of emergency medical services (EMS) providers. This shift is primarily due to a decrease in infectious disease deaths in underdeveloped countries by the continued supply of essential vaccines and intensive disease management, while an increase in mortality from chronic diseases, specifically, emergent diseases like cardiovascular disease and major injuries [1,2].
According to Uzbekistan’s health statistics, the country’s average life expectancy is 72.0 years (female, 74.3 years; male, 69.8 years). The population is relatively young, with 41% under 14 years. There are 4.8 beds and 2.6 doctors for every 1,000 people. It has 81,500 doctors and 259,700 mid-level medical personnel comprising nurses, midwives, and laboratory assistants. Deaths due to chronic metabolic and circulatory diseases, such as cerebrovascular disease and heart disease, account for a significant percentage [2,3]. Furthermore, based on the comparison between major causes between 2009 and 2019, ischemic heart disease rose by 6.1% and stroke increased by 2.8%, metabolic diseases such as cirrhosis rose by 22.6%, and infectious diseases such as lower respiratory tract infections decreased by 25%. Hence, it is imperative to provide appropriate EMS for acute diseases such as cerebrovascular and cardiovascular diseases to promote the community health in Uzbekistan. Appropriate EMS should be accompanied by improving the equipment of the EMS, and the curriculum and training for emergency medical personnel [3].
ODA projects such as the introduction of emergency patient transport ambulances and utlizing the latest emergency management equipment are actively underway in Uzbekistan to help strengthen the emergency medical system. Since 2017, the Korea Foundation for International Healthcare has signed a Memorandum of Understanding with the Uzbekistan Ministry of Health to strengthen EMS capabilities, and provided theoretical and practical training for the workers through onsite training trips of Korean professionals. The Ministry of Health, after consultation with the director of the Tashkent Ambulance Center, certified the EMS training for this project as a regular curriculum, and recognized the completion time for the trainees. However, due to the rapid spread of coronavirus, countries have banned human resource exchanges under the national quarantine guidelines (Ministry of Foreign Affairs; March 23, 2020), making it impossible for professionals to hold training seminars in Uzbekistan [4]. Consequently, it is challenging to train emergency medical workers to reinforce their competency.
Therefore, since onsite education is difficult during COVID-19, the authors have implemented an online training of trainers (ToT) for Uzbekistan emergency medical professionals to facilitate the local application of emergency medical advanced courses. Through these trainers, the Emergency Medical Advanced Course was conducted for local emergency medical workers who boarded ambulances. Accordingly, the authors shared the experience of running online ToT and an emergency medical advanced course centered on local instructors as a part of the ODA project, and discussed its results and effects.
METHODS
Study design
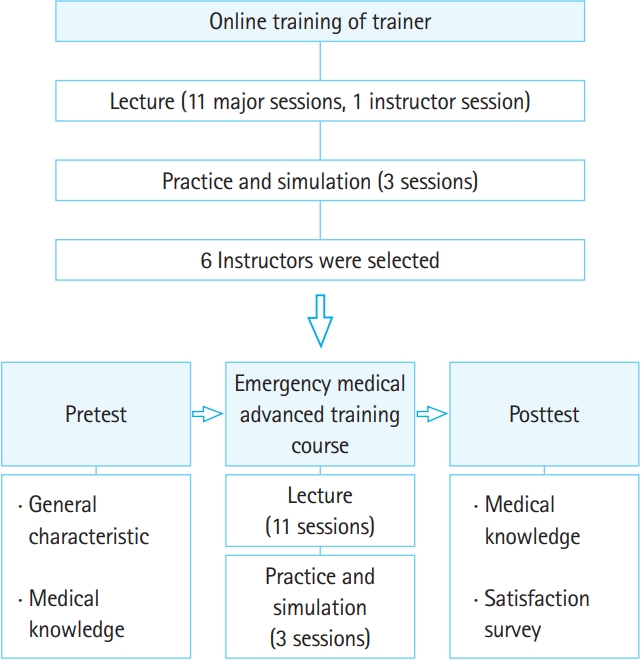
This study was a retrospective descriptive study of online ToT among emergency medical personnel experts and emergency medical advanced courses provided by trained instructors in Uzbekistan. This study was approved by the Institutional Review Board of Inje University Ilsan Paik Hospital (No. 2021-02-006-002). This comprised lecture-based education, practice, and simulation-based training (Fig. 1), for 5 days for emergency medical experts who had experienced simulation-based education in Uzbekistan. This curriculum was similar to that of the Emergency Medical Advanced Course and the “becoming good instructors” curriculum. ToT trainees were educated using video lecture materials dubbed in Russian, and those were made available to trainees through ubiquitous-based learning (UBL) Cloud (NSDevil Co., Daejeon, Korea). For practice sessions, video conferencing was used to demonstrate key procedures in real-time, and ToT trainees directly participated in the practice using the same educational equipment. The simulation training was conducted by emergency medical experts using the same simulation equipment and ToT trainees. In these curriculums, researchers used video conferences to evaluate trainees’ performance and to provide direct feedback.
After the online ToT, instructors were selected based on written tests and video monitoring of practice and simulation performance of trainees who completed the program. We provided the syllabus, instructor manuals of practice, and simulation operation for the courses. To guarantee the quality, the researchers directly instructed through video conference on how to conduct practice and simulation-based training two hours before this training course began.
Operation of the emergency medical advanced course
The participants were emergency medical staff at the Tashkent Ambulance Center in Uzbekistan. Emergency medical personnel who were certified general physicians and boarded ambulances were primarily selected. Considering the characteristics of practice and simulation-based training, four or fewer trainees were recruited per instructor in each course, totaling around 24 trainees, and the course was opened as face-to-face over a period of 5 days.
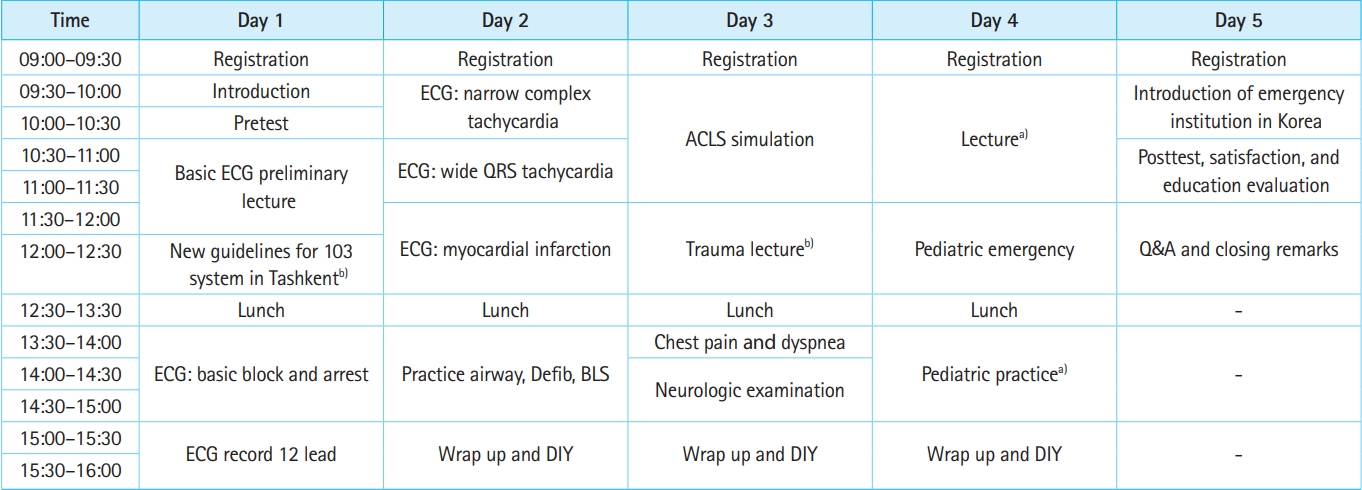
During the online lecture, the instructors utilized notes from the researchers and taught as per the prescribed curriculum. Topics included basic electrocardiography (ST elevation, tachycardia, and bradycardia), pediatric emergencies, pediatric advanced life support, home delivery, neonatal resuscitation program, prehospital neurologic examination, and approach to chest pain, headache, and syncope. Moreover, the UBL cloud allowed trainees to access the course contents for review at any time. Two lectures were given by Uzbekistan experts. The new guidelines of the emergency system in Tashkent and prehospital trauma management lecture were taught to trainees by the director of Tashkent Ambulance Center and a trauma surgeon.
The practice session comprised 12-lead electrocardiography recording, airway and bag valve mask ventilation, basic life support, and defibrillation (Fig. 2). Training equipment was used to increase accessibility for trainees. The 12-lead electrocardiography recording required three to four trainees to monitor the electrocardiogram (ECG). Airway and bag valve mask ventilation required trainees to directly apply oxygen masks to a manikin and insert endotracheal tubes. Basic life support required chest compression and mouth-to-mouth ventilation. Defibrillation required trainees to attach electrodes to a manikin and monitor, charge, and perform it directly.
The simulation course consisted of home delivery, neonatal care, neonatal resuscitation, and advanced cardiac life support (ACLS) (Fig. 2). Simulation on pediatric advanced life support was omitted due to time. Home delivery, neonatal care, and resuscitation were from delivery to early management of normal newborns (wiping, stimulating, and using oral aspirators) and neonatal asphyxia and resuscitation. The trainings were provided using neonatal maternal training equipment. The number of trainees in the ACLS simulation were limited to eight in one scenario, and two instructors participated, with one manipulating the manikin control and the other guiding the scenario. ACLS scenarios focused on cardiac arrest, and a series of courses were taught via simulation using checklists, including chest compression and ventilation support, drug administration, defibrillation, and patient evaluation.
Evaluation and survey of emergency medical advanced course
We tested all trainees using written tests in Russian regarding their clinical knowledge before and after the emergency medical advanced course (Supplementary Material 1). Trainees participated in the pretest before the course and the posttest after completing it. To accurately assess educational effectiveness, questions were randomly allocated, and trainees were tested for an hour under onsite supervision. The questions centered around ECG reading, emergency management at the scene, and resuscitation for children and adults. Questions regarding ECG consisted of four basic and six advanced questions, and the results were calculated out of 100 points. There were eight questions on emergency management at the scene, including those related to pediatric emergencies, emergency childbirths, neonatal resuscitations, chest pain assessments, and neurological tests, and the results were calculated out of 100 points. There were seven questions on pediatric and adult cardiopulmonary resuscitation (CPR), ranging from basic to drug administration for advanced cardiac life support, with the results calculated out of 100 points. Based on the summation of ECG readings (100 points), emergency management at the scene (100 points), and CPR (100 points), the educational assessment results were evaluated out of 300, and then compared and analyzed.
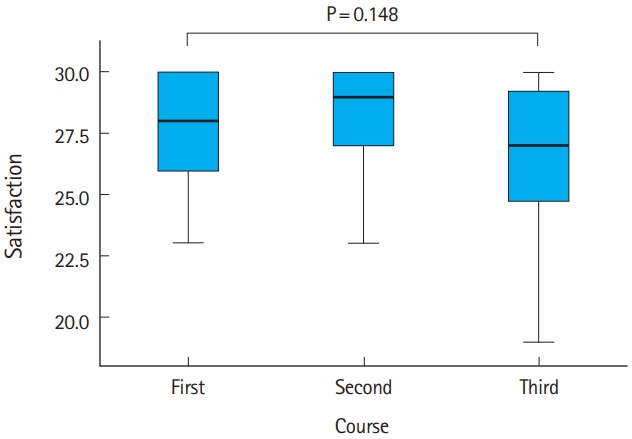
On a Likert scale, all participants were surveyed about the contents and relevance of the emergency medical advanced course. The questionnaire on the content included items on the training content, its difficulty, and appropriateness of the course time. Questions on relevance to the workplace, utilization in the prehospital field, and competency and confidence in prehospital procedures were examined. Based on a Likert scale summing rating of the sub-items, satisfaction was evaluated on a 30-point scale. Each course curriculum was compared and analyzed. A satisfaction survey on education methods was administered to obtain trainees’ understanding, effectiveness, and interest as sub-items using a Likert scale, rated with 15 points. Moreover, each method of education was individually examined for satisfaction and compared.
Statistics
Using the D’Agostino-Pearson test, continuous variables were expressed as the mean±standard deviation for normally distributed data and as the median value (interquartile range [IQR], 25%–75%) for non-normally distrubted data. The statistical significance between pretests and posttests was assessed with a paired t-test and the Wilcoxon signed-rank test. The statistical significance among the three groups was assessed with the Kruskal-Wallis test, followed by multiple comparisons post-hoc analyses with Bonferroni correction. A P-value <0.05 was statistically significant. Data were analyzed using IBM SPSS Statics ver. 20 (IBM Corp., Armonk, NY, USA).
RESULTS
We selected six instructors to conduct the emergency medical advanced course that was voluntarily attended by 22, 23, and 23 emergency medical workers in the first, second, and third sessions respectively. Four trainees were excluded because they did not complete the course. All 64 trainees (52 men and 12 women) were certified general physicians, with an average age of 40.5±10.0 years. The median clinical experience of trainees, including those working with ambulances, was 15.0 years (IQR, 6.0–22.0 years), and the median ambulance staff experience was 10.5 years (IQR, 3.0–15.8 years).
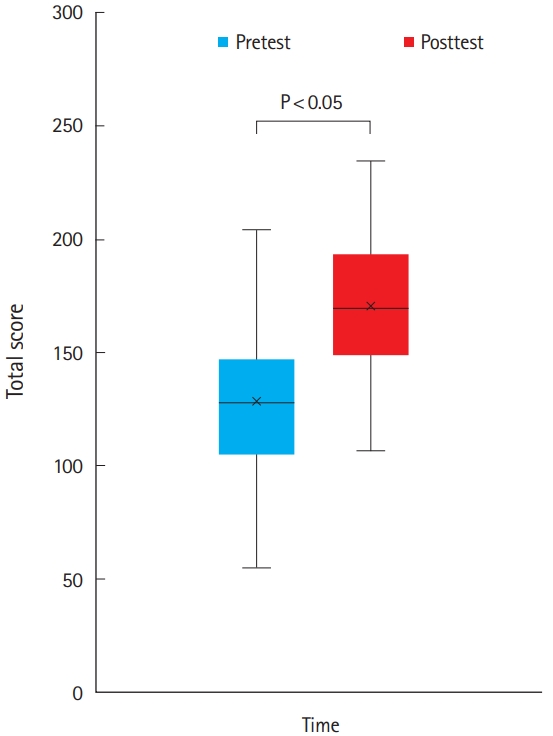
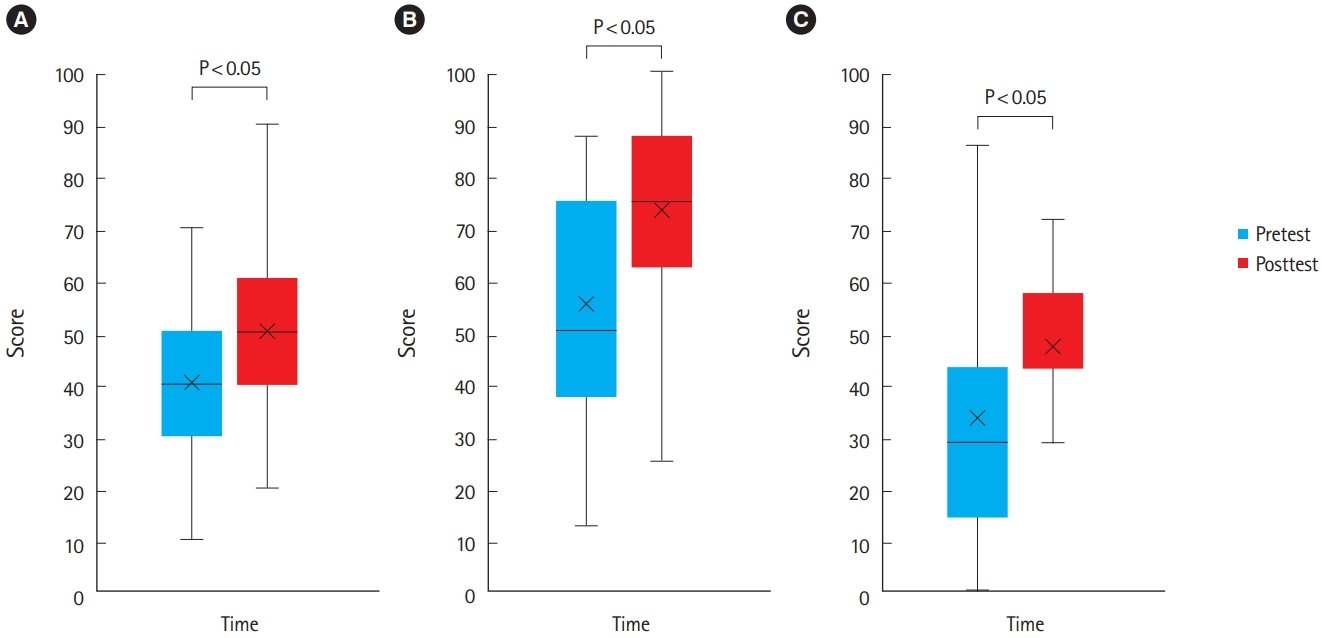
The total score on the pretraining test was 129.2±34.8, and on the posttraining test was 170.8±31.2, which was significantly higher (P<0.05) (Fig. 3). According to the test questionnaires, the analysis is as follows: for pretraining test, ECG scores were 40 (IQR, 30–50), emergency management at the scene scores were 50 (IQR, 37.5–75.0), and pediatric and adult CPR scores were 28.6 (IQR, 14.3–42.9); for posttraining test, ECG scores were 50 (IQR, 40–60), emergency management at the scene scores were 75 (IQR, 62.5–87.5), and pediatric and adult CPR scores were 42.9 (IQR, 42.9–57.1). In summary, the statistical significance of all sub-items was high (P<0.05) (Fig. 4).
According to the survey on the emergency medical advanced course, 34 respondents were very satisfied (53.1%), 25 were satisfied (39.1%), three were neutral (4.7%), and two were dissatisfied (3.1%). Regarding the level of difficulty, 44 responded very satisfied (68.8%), 16 satisfied (25.0%), and four neutral (6.3%). On the appropriateness of course time, 36 responded very satisfied (56.3%), 24 satisfied (37.5%), and four neutral (6.3%). Regarding the utilization of fields, 43 responded very satisfied (67.2%), 18 satisfied (28.1%), and three neutral (4.7%). On confidence, 43 responded very satisfied (67.2%), 19 satisfied (29.7%), and two neutral (3.1%). On competency, 47 responded very satisfied (73.4%), 16 responded satisfied (25.0%), and one neutral (1.6%). Curriculum satisfaction calculated by adding the values of survey items was 28.0 (IQR, 26.0–30.0), and there was no statistical difference in trainee satisfaction among the three sessions (P=0.148) (Fig. 5).
In the survey on the emergency medical advanced course, satisfaction with the lecture-style training method was 14.0 (IQR, 12.0–15.0), and the training method using practice and simulation was 15.0 (IQR, 14.0–15.0). There was no statistical difference between the lecture-style method and practice and simulation method across the three sessions (P=0.095 and P=0.067, respectively).
DISCUSSION
This study described the online ToT experience of tutoring instructors of emergency medical advanced courses in Uzbekistan during the COVID-19 pandemic. We observed that the instructors trained via the online program could successfully provide an emergency medical advanced course for local emergency medical workers. In Uzbekistan’s capital Tashkent, EMS are provided by 12 branches and 204 ambulance stations, managed by the Central Emergency Medical Center, which has 140 ambulances and 1,642 paramedics on duty. EMS providers mainly comprise general physicians, feldshers, and nurses. Physicians can earn their licenses after completing a 3-year college degree and a 7-year medical school curriculum, while feldshers must complete courses focused on emergency treatment, EMS, obstetrics, and surgical care after 4 years of professional training. The nurse’s curriculum entails 3 years of university or lyceum study [5].
All emergency medical workers who use ambulances are required to complete a 1-year curriculum certified by the Ministry of Health of Uzbekistan. In Uzbekistan’s emergency medical system, these workers are responsible for more than transferring and managing emergency patients. They also diagnose the patient’s condition at the scene and make out a prescription for them. As part of primary treatments, patients in nonemergency conditions can be prescribed or administered medication, or in emergencies, they can be transferred to a hospital while receiving prehospital treatment. Since ambulance services and primary health care are free in Uzbekistan, local demand is high. Hence, proper emergency management and clinical decision-making by EMS providers is essential.
By partnering with the American International Health Alliance, the ODA project, initiated for emergency medical systems in Uzbekistan, conducted a multimedia lecture and workshop in 1999 [6]. As of 2002, 1,467 were trained, including 112 general physicians and 749 feldshers. It has been a meaningful curriculum as the first ODA project focused on EMT in Uzbekistan [6]. However, a lack of financial support and educational facilities prevented the provision of regular training courses based on practice to emergency medical staff in the field [6].
A preliminary survey of emergency medical staff in Tashkent revealed that only 22% to 38% of emergency medical staff had experience and were confident with advanced airways and endotracheal intubation, and only 18% to 20% had experience with defibrillators and cardioversion [7]. Moreover, according to the test results conducted to confirm the medical knowledge level, only half of the participants chose the proper diagnosis and clinical decision in the questions on basic CPR, ECG, and neonatal resuscitation. These findings suggest that the absence of practice and simulation-based curriculums and clinical experience in Tashkent will hinder their ability to provide emergency management and make good clinical decisions during emergencies [7].
Korea Foundation for International Healthcare supported training courses developed for emergency medical staff boarding ambulances through the “Emergency Medical System Reinforcement Project in Tashkent city, Uzbekistan” in 2017 and the “Uzbekistan Emergency Medical Service Capability Building Project” in 2019. Furthermore, due to the growing importance of emergency medical systems as a result of various ODA projects, an emergency medical curriculum that can be opened independently was required to quickly strengthen the staff’s capacity. Considering the pretest/ posttest and satisfaction results of the emergency medical advanced course, it is feasible to continuously provide high-quality emergency medical education by training excellent instructors through ToT programs that do not require in-person instruction.
In emergency medical education, simulation-based has been gaining attention since the 1990s. Simulators allow the hands-on practice of procedures, repeated learning, and less risk of harm. Moreover, it is considered an efficient teaching method as the same learning situations can be presented to various learners with immediate feedback [8]. Several studies have confirmed the effectiveness of practice and simulation-based educational methods. According to a report by Tavares et al. [9] when the simulation-based curriculum was conducted and simulation-based assessment was implemented for 49 paramedic trainees, the average competency among participants improved in scene assessment, medical history listening, patient evaluation, decision-making, and communication. Moreover, Jang et al. [10] revealed that an eight-week course of ECG education for first-class emergency medical personnel improved knowledge from 26.8 points before training to 45.3 points after, and Funk et al. [11] reported a significant enhancement in knowledge after medical training for myocardial infarction patients.
The posttest results were significantly higher (pre-education test 129.2±34.8, post-education test 170.8±31.1, P<0.05). Moreover, the results from the posttest were significantly higher in the ECG, emergency management, and pediatric and adult CPR domains. Furthermore, according to the satisfaction survey conducted on the training methods, the lecture-based training was rated 14.0 (IQR, 12.0–15.0), while the practice and simulation-based training was rated relatively higher at 15.0 (IQR, 14.0–15.0). These results highlight the importance of training emergency medical personnel through programs that use practice and simulation. Hence, the effectiveness and satisfaction of future education for emergency medical personnel can be increased by combining these two aspects along with simulations similar to the prehospital fields.
This study had several limitations. First, a significant portion of practical training focused on prehospital procedures and techniques; however, environmental factors that could limit prehospital performance on the scene were not considered. As various factors related to the prehospital environment play a role, the testing of emergency management and clinical decision of trainees based on only practical curriculum has limitations. Thus, in future research, the effectiveness of education can be verified using major indicators in EMS within the community after the completion of the curriculum for emergency medical workers. Second, the Emergency Medical Advanced Course was unable to provide standardized education in practice and simulation-based training. Due to the physical and linguistic limitations caused by COVID-19, ToT was conducted through video conferencing, online lectures, and instructor manuals for local experts with prior experience in the curriculum. Despite this, education involving practice and simulation cannot provide immediate feedback. Hence, it is inevitable that curriculum standardization is limited by differences in instructor competencies, which may negatively impact test results and trainee satisfaction. Hence, deploying experts to local sites for emergency medical staff education is important for advancing and researching emergency medical worker education projects. Third, the fundamental gap among trainees who participated in the three sessions was not considered. While the effectiveness of the course on medical knowledge could be determined pretest and posttest, the testing of trainees for practice and simulationbased training did not consider their practices and clinical experiences. As there is a significant difference in the educational effectiveness of emergency medical staff based on levels of knowledge and clinical experience, the selection process of future trainees should include the pretest scores and clinical experience. Fourth, as the major religion followed in Uzbekistan is Islam, death is perceived not as termination of life, rather its continuation in another form. At the scene of cardiac arrest in the emergency department, the rate of performing CPR is less than in other countries. Hence, in training emergency medicine specialists, education on persuading patient’s family is needed.
To summarize, we trained instructors of the emergency medical advanced courses through online ToT among experts of emergency medical personnel in Uzbekistan. The instructors could successfully provide the emergency medical advanced course comprising lecture, practice, and simulation. Results suggest that the qualified education of instructors through online ToT programs could result in effective training of other healthcare providers.