In a crowded emergency department (ED), several crucial decisions must be made to provide effective patient care [1,2]. Prehospital decision-making, such as transport location and timing decisions, are crucial for continuity of care from prehospital to hospital levels [3-5]. Appropriate triage is required for selective and targeted care of critically ill patients [6]. To improve patient outcomes, a prompt investigation and intervention decision should be achieved [7,8]. The final disposition choice must consider patient safety [9]. Management of the overall process and the allocation of resources are also essential for ED operation [10]. Overall, the decision-making points should be considered based on patient state and ED situation.
Clinical decision support (CDS) based on artificial intelligence (AI) has recently been introduced into numerous medical fields, including emergency care. Increased data sources such as wearable devices and electronic medical records, higher computing power, and increased storage locations such as online cloud databases have contributed to the expansion of AI technology. As a result, several AI-based algorithms have been introduced for use in the ED journey.
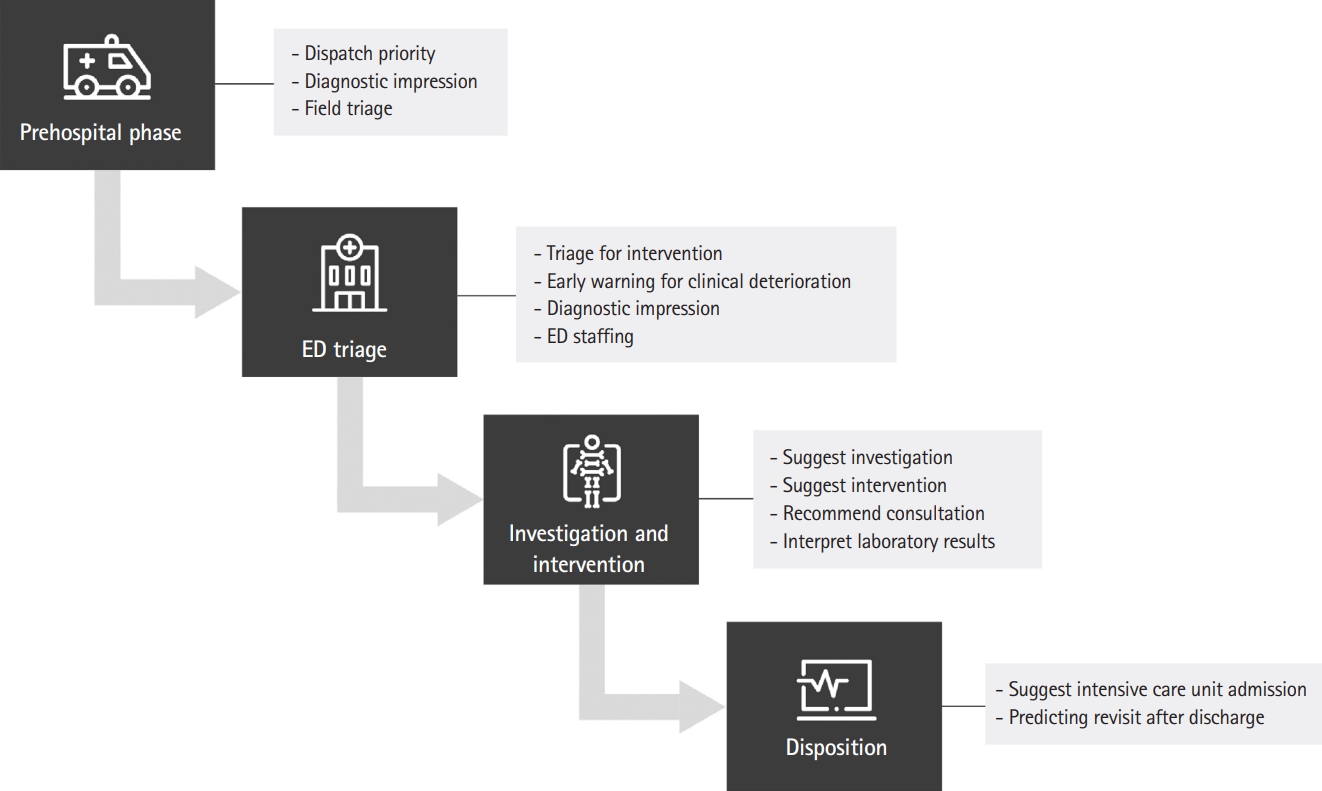
AI-CDS can be categorized according to the decision phase of the ED journey. From the standpoint of patient care and based on a previous study, the ED journey can be classified into phases of prehospital phase, triage, investigation, intervention, and final disposition [11]. Each stage has its own decision objective and may be repeated based on the situation in the ED and the patient condition (Fig. 1).
During the prehospital period, decisions are based on the experience of the medical staff at the scene and the protocols of the local emergency medical service. However, it is difficult to make decisions with limited resources and patient information. With AI-CDS, efforts have been made to improve the accuracy of initial diagnoses based on prehospital information and data. Dispatching could also be aided by AI-CDS; for example, when the conversation between callers and bystanders shows certain context or words for critical conditions, systems would suggest higher-level providers to be dispatched. With prehospital data, a machine-learning-based prediction of hospital admission was attempted in a previous study to inform prehospital providers of patient prognosis after ED care [12]. Natural language processing techniques were implemented in prehospital paramedic reports for diagnosis of stroke [13]. A previous study predicted early sepsis using prehospital data [14].
Nations and institutions have their own triage system for proper early care of a critical patient and effective resource distribution [7,15]. Underestimation or overestimation of triage can result in resource loss or deterioration of critically ill patients due to delayed care [6]. For triage, several AI-CDS system or novel AI-based methods have been introduced. There have been attempts to predict outcomes such as mortality or admission, including development of certain clinical conditions such as sepsis [16-18]. However, few studies demonstrate prospective AI-based triage research or implementation [19,20]. Attempts should be sought to match ED triage with ED resource allocation, including staff, beds, and investigatory efforts.
Prescription and interpretation of diagnostic tests are included in the investigation phase. The intervention phase consists of interventions and medication to improve patient conditions. Investigations and interventions that are time consuming and equipment restrictive should be limited. AI can assist in allocation of investigatory and treatment options or to plan expert consultations.
Investigation and intervention tools can be inputs or outputs of an AI algorithm. Some research has attempted to predict the need for computed tomography in the evaluation of disease [21]. Selected interventions can be a result of a prediction [22]. The majority of investigational studies are concerned with interpretation of diagnostic tests in relation to final diagnosis and outcome [23-25].
In an ED, the decision for further management should be made carefully and appropriately. A patient-specific disposition, such as intensive care unit admission, is a frequently targeted outcome [25-27]. Predicting the readmission or return of a discharged patient is also essential [28,29]. Before making a final determination, these algorithms can help physicians reconsider the conditions of their patients.
Several barriers exist regarding the nature of AI. The first issue involves the data. Due to the nature of AI-based algorithms, data quality is as important as data quantity. Using low-quality data as input renders the algorithm less effective. However, unlike that from the intensive care unit, ED data collection is challenging due to rapid patient turnover and the complex environment. Additionally, patient information is easily lost along the path from injury to ward admission. Data collection should be encouraged, and data quality must be maintained.
It is well known that AI-based algorithms have a ŌĆ£black boxŌĆØ nature [30,31]. Therefore, it is difficult to determine the decisionŌĆÖs cause or the decision-making process. To overcome the uncertainty of AI, explainable AI has recently been introduced, such as modified scoring systems or showing feature importance [32,33]. It is anticipated that explainable artificial intelligence-based predictive models will be applicable to emergency medicine as they are implemented throughout the medical field [34].
Recent review articles revealed that only a small number of AI-based models are utilized in actual practice, despite the development of numerous AI-based models for diverse decision phases [35-37]. The health care field is strictly managed by regulations, which is considered as the most important factor for delayed implementation of AI-CDS. For example, a randomized controlled trial is an important strategy to analyze the regulatory process, which is often difficult or impractical for AI-CDS. With these reasons, we do not frequently witness AI-CDS in practice.
Several AI-CDSs have been developed to cope with ED problems and can be categorized by the decision point in an ED: prehospital, triage, investigation, intervention, and disposition phases. Recently, only few of AI-CDS had been implemented and used in actual practice. These obstacles should be evaluated from the aspects of data, algorithm, and application. AI implementation is a practical decision that involves continuous and harmonized efforts by the ED, information technology, and data science.