Sepsis is a global burden with no specific treatment [1,2]. Traditional treatment has focused on macrocirculation and hyperinflammation, but none has been successful.
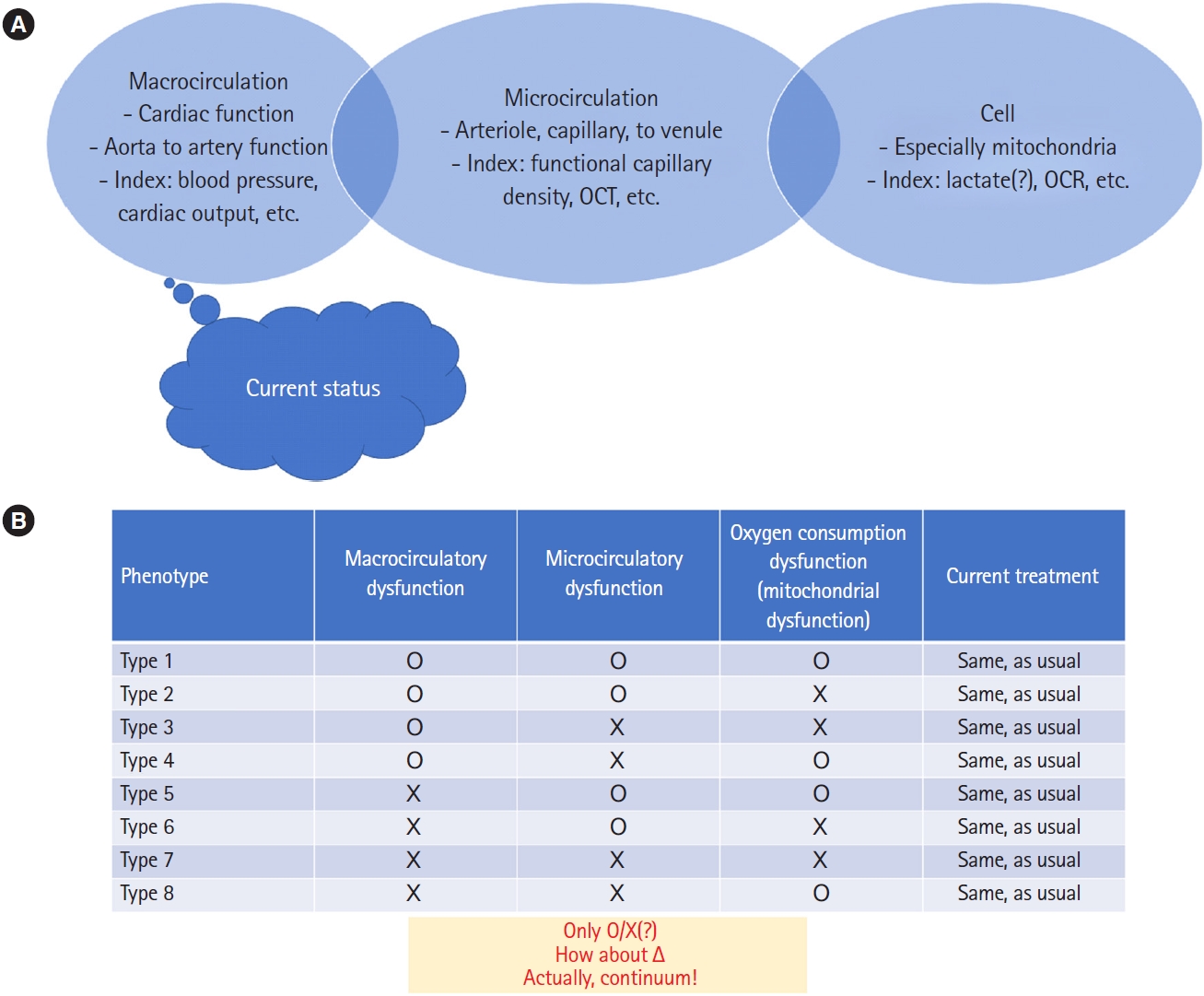
Sepsis is not a single disease but can have many phenotypes [3]. Regarding oxygen supply and consumption, three systems are important: macrocirculation, microcirculation, and mitochondria [4]. Macrocirculation comprises cardiac function and arterial resistance (compliance). Fluid resuscitation and vasoactive treatment target cardiac output and blood pressure, which are components of the macrocirculation. Microcirculation is important since it is the last path for oxygen to reach the cell. Even though the optimal macrocirculation targets (blood pressure and cardiac output) can be achieved, the oxygen might not be able to be used by the cell due to microcirculatory and/or mitochondrial dysfunction. In this way, analysis is limited by lack of a widely and clinically used diagnostic tool to monitor microcirculation and mitochondrial function. At the investigational level, there are monitoring devices for those purposes [5,6]. Additional treatment options could be developed with advancement of real-time monitoring of these three components. As in Fig. 1, different combinations of sepsis are possible according to the three systems, and treatment could be more personalized rather than using the ŌĆ£one-size-fits-allŌĆØ concept.
Another potential issue in sepsis is inflammation status. The traditional approach to reduce hyperinflammation (i.e., cytokine storm) is not optimal, and opposing treatments to enhance immune function are becoming more common [7]. For example, anti-programmed death-1 (anti-PD-1)/anti-programmed death ligand-1 (anti-PDL1), interferon gamma, and interleukin-7 are being investigated. However, the spectrum of immune status of patients is not categorical and can be rating scale and compartment specific. Therefore, additional diagnostic approaches are needed.
Medical treatment is dependent on the specific diagnosis, which requires knowledge of in-depth pathophysiology. To improve treatment of sepsis, its in-depth pathophysiology must be better understood for ideal diagnosis and personalized treatment.