Trends in emergency department visits for emergency care–sensitive conditions before and during the COVID-19 pandemic: a nationwide study in Korea, 2019–2021
Article information
Abstract
Objective
Emergency care systems worldwide have been significantly affected by the COVID-19 pandemic. This study investigated the trend of emergency department (ED) visits for emergency care–sensitive conditions (ECSCs) in Korea before and during the pandemic.
Methods
We performed a longitudinal study using the national ED database in Korea from January 2019 to December 2021. We calculated the number and incidence rate of visits for ECSCs per 100,000 ED visits, and the incidence rate ratio of 2021 relative to the value in 2019. The selected ECSCs were intracranial injury, ischemic heart disease, stroke, and cardiac arrest.
Results
The number of ED visits for all causes decreased by about 23% during the pandemic. The number of ED visits for intracranial injuries decreased from 166,695 in 2019 to 133,226 in 2020 and then increased to 145,165 in 2021. The number of ED visits for ischemic heart disease and stroke decreased in 2020 but increased to 2019 levels in 2021. In contrast, the number of ED visits for cardiac arrest increased from 23,903 in 2019 to 24,344 in 2020 and to 27,027 in 2021. The incidence rate and incidence rate ratio of these four ECSCs increased from 2019 to 2021, suggesting increasing relative proportions of ECSCs in total ED visits.
Conclusion
During the COVID-19 pandemic, the number of cardiac arrests seen in the EDs increased, but that of other ECSCs decreased. The decrease in ED visits for ECSCs was not as pronounced as the decrease in ED visits for all causes during the pandemic. Further studies are needed to determine clinical outcomes in patients with ECSC during the pandemic.
INTRODUCTION
After the first case of COVID-19 was reported in Wuhan, China, in December 2019, this dangerous epidemic spread worldwide [1]. By July 2023, the World Health Organization (WHO) reported that more than 760 million people were infected with COVID-19, and more than 6.9 million of those infected had died [2]. In regions critically impacted by COVID-19 cases, such as Europe and North America [3], substantial medical resources were required to respond to this situation [4]. Moreover, these efforts had to be carried out while ensuring continued access to essential health care services [5]. However, emerging studies have suggested that the COVID-19 pandemic had a negative impact on health care utilization [6]. A study conducted in five states in the United States [7] found that emergency department (ED) visits decreased by 41.5% to 63.5% in the 4 months following the pandemic outbreak compared to before the pandemic. Another Canadian study [8] found that the decline in ED visits continued for more than two years after the start of the pandemic. These declines in access to EDs are raising concerns that patients with acute life-threatening conditions such as acute myocardial infarction (AMI), stroke, and out-of-hospital cardiac arrest (OHCA) may not be able to access prompt care. In fact, there was a 10% decrease in AMI patients who visited the ED for coronary artery revascularization during the first wave of the COVID-19 pandemic in Korea [9].
Despite growing concerns, the impact of the pandemic on the emergency care system has not been fully studied. Most studies are limited to the first year of the pandemic, and nationwide data are limited. Considering that the pandemic has put a strain on the emergency care system over the past 2 years, longer-term studies are needed. Therefore, this study aims to explore the changes in ED visits for emergency care–sensitive conditions (ECSCs) in Korea before and during the pandemic using national data.
METHODS
Ethics statement
This study was approved by the Institutional Review Board of the National Medical Center (No. NMC-2021-10-123). The requirement for informed consent was waived due to the retrospective nature of the study.
Data source
This was a retrospective time-series study using data from the National Emergency Department Information System (NEDIS) between 2019 and 2021. NEDIS is a nationwide information system developed in 2003 to collect and store information on patients visiting EDs in Korea. The NEDIS database is designed to assist professionals and policy makers involved in emergency care at the regional and national levels to evaluate the performance of the emergency care system and to support future strategic planning. To this end, NEDIS provides a framework for collecting, storing, and sharing standardized data. Through NEDIS, participating EDs transmit visit-level patient data, including demographic, administrative, and clinical information, to a central processing facility. All patient-related information is anonymized and transmitted electronically, and data inconsistencies are detected manually and using computational algorithms. Detailed design and variables of the NEDIS database have been described elsewhere [9–12].
Study population
From the NEDIS database, we identified all ED patients and those with ECSCs as the primary diagnosis between January 1, 2019, and December 31, 2021. According to the definition of ECSC, we selected four of 50 time-sensitive condition candidates presented in previous studies using a multidisciplinary expert consensus method [13,14], considering the incidence and disease burden in Korea. The four ECSCs selected for the study were ischemic heart disease (IHD), stroke, cardiac arrest, and intracranial injury. The International Classification of Diseases, 10th Revision (ICD-10) codes for ECSCs are presented in Supplementary Table 1.
Outcomes
The primary outcome of interest was the number and incidence rate (IR) of ED visits for ECSCs during the study period. The secondary outcome was the incidence rate ratio (IRR) of ED visits for ECSCs.
Statistical analysis
The number and IRs of ED visits for ECSCs were calculated for each ECSC by calendar month. ED visit trends for ECSCs were presented as line charts according to calendar months from 2019 to 2021. The IR of ECSC per 100,000 ED visits was defined as follows:
To estimate changes in ED visits for ECSCs before and during the pandemic, 2019 was designated as the before pandemic period, while 2020 and 2021 were designated as the during pandemic period. Poisson regression was used to calculate IRR and 95% confidence intervals, which are IR comparisons for ECSCs before and during the pandemic.
The database construction and statistical analysis were performed using SAS ver. 9.4 (SAS Institute) and R ver. 4.1.1. (R Foundation for Statistical Computing). Results with a two-tailed P<0.05 were considered statistically significant.
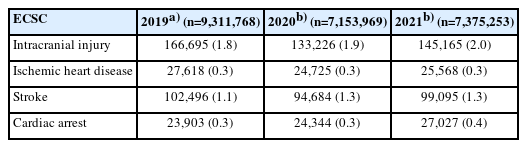
RESULTS
Between 2019 and 2021, the participation rate of nationwide EDs in the NEDIS was 99.8% (401 of 402) in 2019, 100% (403 of 403) in 2020, and 100% (405 of 405) in 2021. From the NEDIS, we identified a total of 23,840,990 ED visits from January 1, 2019, to December 31, 2021. Of these, 9,311,768 patients visited EDs before the pandemic period, and 14,529,222 patients visited EDs during the pandemic period (Table 1). The number of ED visits for all causes during the pandemic period decreased by about 23% compared to the pre-pandemic period. However, the number of ED visits for ECSCs showed a smaller decrease or even increased. The number of ED visits for intracranial injuries decreased by about 20% in 2020 and by 13% in 2021 compared to before the pandemic period. The number of ED visits for IHD and stroke decreased in 2020 but increased to 2019 levels in 2021. In contrast, the number of ED visits for cardiac arrest continued to increase during the pandemic.
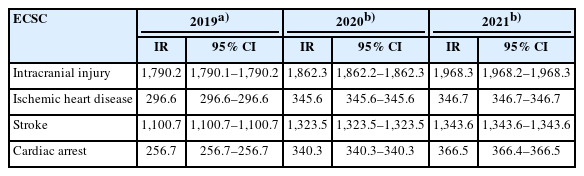
The IRs of ED visits for ECSCs are presented in Table 2. The IRs of ED visits for intracranial injury per 100,000 ED visits were 1,790.2 (95% confidence interval [CI], 1,790.1–1,790.2) in 2019, before the pandemic period, and 1,862.3 (95% CI, 1,862.2–1,862.3) in 2020 and 1,968.3 (95% CI, 1,968.2–1,968.3) in 2021, during the pandemic period. Similar IR patterns were observed in all ECSC diagnostic groups. The number of ED visits for ECSCs decreased during compared to before the pandemic. However, the IR of ED visits for ECSCs increased because the denominator, which is the number of ED visits for all causes, decreased by a larger margin. This suggests that the decrease in ED visits for ECSCs was not as pronounced as the decrease in ED visits for all causes during the pandemic period.
The IRRs of ED visits for ECSCs are presented in Table 3. The IRR of ED visits for intracranial injury was 1.04 (95% CI, 1.03–1.05) in 2020 and 1.10 (95% CI, 1.09–1.11) in 2021. The IRR of ED visits for each ECSC in 2021 was significantly higher than that in 2020. This is because the IR of ED visits for ECSCs increased in 2021 compared to 2020. In particular, the IRR of cardiac arrest in 2021 was significantly higher than that in 2020.
DISCUSSION
In this study, we found that the number of overall ED visits in Korea decreased sharply during the COVID-19 pandemic. However, the decrease was less pronounced for ECSCs. In fact, the number of ED visits for cardiac arrest increased. The IR of ED visits for ECSCs increased during the pandemic, and the IRR of ED visits for ECSCs in 2021 was significantly higher than that in 2020. This suggests that the decrease in ED visits for ECSCs was not as pronounced as the decrease in ED visits for all causes during the pandemic period. This may be because individuals with ECSCs were more likely to seek care at the ED during the pandemic due to the increased risk of complications from their condition. Additionally, the increase in ED visits for cardiac arrest during the pandemic could be due to the worsening condition of patients with originally acute conditions due to delay in seeking emergency care [15].
The decrease in ED visits may reflect a decrease in the actual need for emergency care, a decrease in access to emergency care, or a combination of both. Several factors may have contributed to the decrease in ED visits for ECSCs during the pandemic period, including social distancing, public fear of COVID-19, and diversion of patients to COVID-19-designated hospitals. For some types of ECSCs, the decrease in ED visits may be due to a “true” decrease in the number of cases. Korea, like other countries, has implemented nonpharmaceutical interventions (NPIs) such as telecommuting, travel restrictions, and gathering bans to reduce the transmission of COVID-19 through person-to-person contact [16]. These NPIs, known as social distancing, led to a significant decrease in outdoor activities and public transportation use, which can explain the decrease in ED visits due to injuries [17,18]. In our study, we found that the number of ED visits for intracranial injuries decreased the most among ECSCs. This finding is consistent with previous studies that have shown a decrease in the incidence of traumatic brain injury following the outbreak of the pandemic [19–22]. For other types of ECSCs, the decrease in ED visits may be due to fear of infection and subsequent avoidance of hospitals [23,24]. For example, individuals may not have sought emergency care because of the fear of exposure to COVID-19 in crowded emergency rooms and the concern about the possibility of extended waiting times [25]. Finally, the Korean government has designated and operated several hospitals only for patients with COVID-19 [26]. However, these measures can increase the challenge for patients with non–COVID-19 emergency conditions in accessing emergency care.
The decrease in the number of ED visits suggests that a significant number of people postponed or canceled ED visits even though they were experiencing acute conditions. ECSC essentially consists of time-sensitive conditions. According to a previous study conducted in Korea [14], delays in hospital access time in ECSCs were associated with increased mortality. Therefore, it is necessary to study whether their long-term clinical outcomes are worse. The decrease in ED visits for ECSCs is concerning as it may lead to worse long-term outcomes for patients with these conditions. It is important to understand the reasons for the decrease in ED visits for ECSCs to develop strategies for mitigating the impact of the pandemic on these patients.
This study has several notable limitations. First, it compared ED visits during the pandemic to those in the year before the pandemic. Long-term changes in the pre-pandemic period were not included in the study. Second, the definition of ECSCs is based solely on ICD-10 codes. Therefore, there is a possibility of misclassification. Third, study populations were not assessed for severity. This means that it is not possible to know the severity of patient conditions, which could impact the results of the study. For example, patients with more urgent conditions may be more likely to seek care at the ED, even during a pandemic. Finally, the study did not assess the clinical outcomes of patients with ECSCs who delayed or canceled ED visits during the pandemic. Further research is needed on this topic.
In conclusion, during the COVID-19 pandemic, the total ED visits for all causes decreased, but the IRs of the ECSCs increased. The number of cardiac arrests increased, but other ECSCs including IHD, stroke, and intracranial injuries, decreased. Understanding the specific conditions that led to the biggest decrease in ED visits during the pandemic is important in planning for the next pandemic, regarding potential vulnerabilities in the emergency care system.
Notes
Author contributions
Conceptualization: SK, EK, SJK; Data curation: SK, JL; Formal analysis: SK, HKS; Funding acquisition: HKS; Methodology: HKS; Writing–original draft: SK, HKS; Writing–review & editing: all authors. All authors read and approved the final manuscript.
Conflicts of interest
The authors have no conflicts of interest to declare.
Funding
This study was supported by a grant from the National Medical Center (Goyang, Korea) (No. NMC2022-PR-01).
Acknowledgments
The authors acknowledge the late Dr. Han-duk Yoon for his dedication in establishing the National Emergency Department Information System (NEDIS).
Supplementary materials
Supplementary materials are available from https://doi.org/10.15441/ceem.23.087.
Supplementary Table 1.
The ICD-10 codes for the selected ECSCs
References
Article information Continued
Notes
Capsule Summary
What is already known
Emergency care systems worldwide have been severely impacted by the COVID-19 pandemic.
What is new in the current study
During the COVID-19 pandemic period, the number of emergency department visits for all causes and emergency care–sensitive conditions, including intracranial injury, ischemic heart disease, and stroke, has decreased significantly in Korea. On the other hand, the number of cardiac arrests has increased.