The impact of COVID-19 on mortality in trauma patients undergoing orthopedic surgery: a systematic review and meta-analysis
Article information
Abstract
Objective
The global spread of the COVID-19 pandemic has affected all aspects of medicine, including orthopedic trauma surgery. This study aims to investigate whether COVID-19 patients who underwent orthopedic surgery trauma had a higher risk of postoperative mortality.
Methods
ScienceDirect, the Cochrane COVID-19 Study Register, and MEDLINE were searched for original publications. This study adhered to the PPRISMA 2020 statement. The validity of the studies was evaluated using a checklist developed by the Joanna Briggs Institute. Study and participant characteristics, as well as the odds ratio, were extracted from selected publications. Data were analyzed using RevMan ver. 5.4.1.
Results
After applying the inclusion and exclusion criteria, 16 articles among 717 total were deemed eligible for analysis. Lower-extremity injuries were the most common condition, and pelvic surgery was the most frequently performed intervention. There were 456 COVID-19 patients (6.12%) and 134 deaths among COVID-19 patients, revealing an increase in mortality (29.38% vs. 5.30%; odds ratio, 7.72; 95% confidence interval, 6.01–9.93; P<0.001).
Conclusion
Among COVID-19 patients who received orthopedic surgery due to trauma, the postoperative death rate increased by 7.72 times.
INTRODUCTION
The World Health Organization (WHO) announced the discovery of a new condition, COVID-19, in early February 2020, before declaring a global pandemic in March 2020. The rapid global spread of the causative pathogen, SARS-CoV-2, has caused major changes to human life worldwide. Many countries in the Asia-Pacific region, including Australia, Korea, and Japan, were among the first to respond to the COVID-19 epidemic [1].
During the COVID-19 pandemic, emergency room visits decreased, particularly visits for trauma and surgical intervention in traumatology cases [2,3]. With this reduction in visits, patients more frequently received delayed care during the current pandemic [4]. Previous studies have shown that delaying surgery increases mortality and the risk of postoperative pneumonia in trauma patients [5].
The present study sought to conduct a systematic review and meta-analysis on postoperative mortality in COVID-19–positive and COVID-19–negative patients undergoing orthopedic trauma surgery. The present meta-analysis sought to investigate the odds ratio (OR) of mortality in this patient population by comparing statistics between COVID-19–positive and COVID-19–negative groups. We hypothesized that postoperative COVID-19–positive orthopedic trauma patients would have a higher risk of death than those tested negative for COVID-19.
METHODS
Search strategy and study selection
The protocol of this review was registered in PROSPERO (International Prospective Register of Systematic Reviews) on September 27, 2022 (No. CRD42022359112). In accordance with recent PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) 2020 statement for identifying research through databases and registers, a systematic review of the mortality in orthopedic surgery owing to trauma during the COVID-19 pandemic was performed, as shown in Fig. 1 and Supplementary Material 1 [6]. The phrases “orthopedic” AND “trauma” AND “surgery” AND “COVID-19” were used to search the ScienceDirect and MEDLINE (via PubMed) databases for English-language studies that reported mortality among both COVID-19–positive and COVID-19–negative patients. The literature search was conducted on September 20, 2022. A search using MeSH (Medical Subject Headings) terms was carried out whenever possible using the combination of the search 1 (“orthopedic trauma surgery” [MeSH Terms] OR “orthopedic trauma surgery” [All Fields]) AND search 2 (“COVID-19 [MeSH Terms] OR “COVID-19” [All Fields]) strategies.
Inclusion and exclusion criteria
We included observational studies like cohort, cross-sectional, and case–control studies but excluded review articles. The validity of the papers included in this study was evaluated using a series of inquiries based on a checklist in line with the kind of study created by the Joanna Briggs Institute [7,8], as shown in Supplementary Table 1 [9–23] and Supplementary Table 2 [24]. Articles that did not fit the requirements for inclusion were rejected. The inclusion criteria formulated according to the PICO mnemonic for clinical research questions were as follows: (1) P (patient, population, problem): patients of all ages who underwent orthopedic trauma surgery; (2) I (intervention, prognostic factor, or exposure): COVID-19 infection (positive or negative polymerase chain reaction result); (3) C (comparison or intervention): none; and (4) O (outcome): postoperative mortality.
Data synthesis
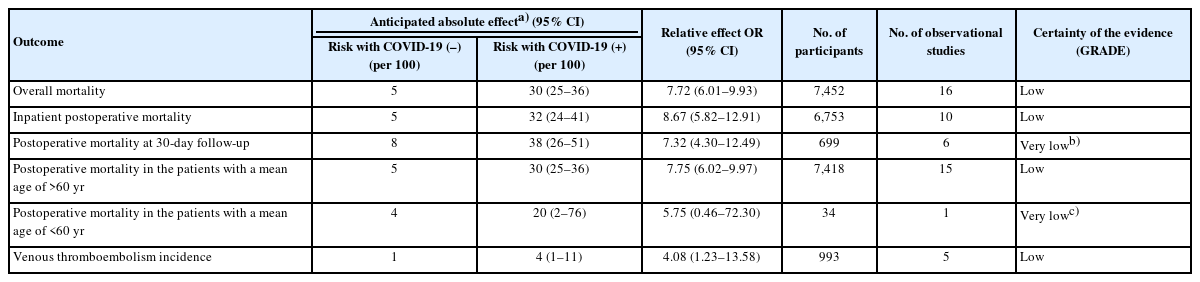
If possible, the data synthesis included information on patient mean age, sex, death rate, underlying disease, complications, intervention site, type of surgery, and hospital stay. The data were summarized in Microsoft Excel (Microsoft Corp) after their collection, and RevMan ver. 5.4.1 (Cochrane Collaboration) was used for statistical analysis. We performed planned subgroup analyses for the confounding variables, which included time points of patient outcome measurement (inpatient vs. 30-day follow-up) and age (<60 years vs. >60 years). Publication bias was measured by visual inspection of funnel plots and quantitatively using Egger test [25]. We considered findings significant if P<0.05. GRADE (Grading of Recommendations, Assessment, Development, and Evaluation) scores were used to evaluate the certainty of the evidence for each outcome [26]. A GRADE summary of the findings in Table 1 was generated using GRADEpro (GradePro Inc.) [27].
RESULTS
During the literature search, 717 studies were discovered. After removing duplicates, 691 studies remained, and 32 potentially relevant studies were chosen for eligibility examination. This meta-analysis included 16 observational studies (10 retrospective cohort studies, five prospective cohort studies, and one crosssectional study). The majority of patients in these investigations were >60 years old. The study characteristics and postoperative mortality findings are shown in Table 2 [9–24]. The most common injury sites were the hip and femur, followed by other lowerlimb sites such as the patella, tibia, ankle, foot, and upper limb. Supplementary Table 3 shows the types of injuries that required orthopedic surgery. Hemiarthroplasty, total hip arthroplasty, unspecified elective minor surgery, and open reduction and internal fixation of the femur were the major surgeries performed.

Incidence of venous thromboembolism, underlying disease, complications, and length of hospital stay in COVID-19–positive and COVID-19–negative groups
Five studies [15,18,20,21,24] compared the number of orthopedic surgeries performed during and before the start of the COVID-19 pandemic and discovered that the numbers of surgeries performed did not significantly differ. Nonetheless, postoperative mortality increased significantly during the pandemic.
During the COVID-19 pandemic, 7,795 injuries were reported (Supplementary Table 3), with 15 cases (0.19%) not being treated surgically. According to Table 2 [9–24], we identified 6,996 COVID-19–negative patients (93.89%) and 456 COVID-19–positive patients (6.11%) among the 7,452 operative patients who underwent COVID-19 testing via polymerase chain reaction testing of a nasopharyngeal swab. Meanwhile, 134 COVID-19–positive patients (29.38%) died after surgery compared to 5.30% of the COVID-19–negative group, despite the small number of COVID-19–positive patients. The mortality rate of COVID-19–positive patients ranged from 14.28% to 50% among included studies.
Complications due to COVID-19 were most commonly reported as the primary cause of postoperative death among COVID-19–positive patients. The reported primary causes of postoperative death, complications, underlying disease, and mean hospital stay in both groups are shown in Table 3 [9–24]. Eight studies [11–15,19,20,22] did not report the cause of death in their research.
A total of 1,616 reported surgeries from seven studies [13,16–18,20–22] are shown in Supplementary Table 4. In contrast, nine studies [9–12,14,15,19,23,24] did not specify the surgeries performed in their studies. Only Lim et al. [18] reported the type of anesthesia used in both groups.
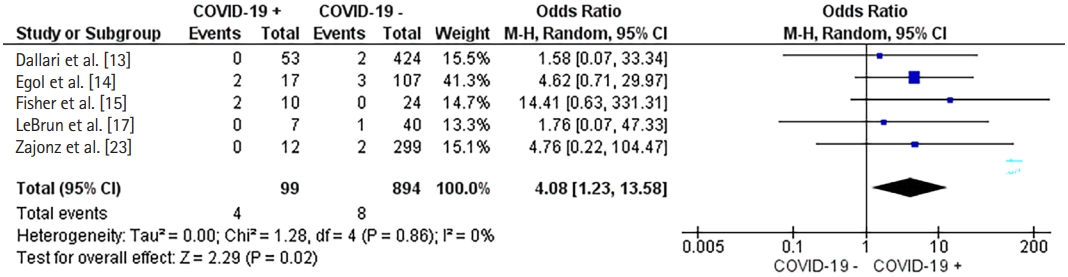
Fig. 2 depicts the qualitative analysis of each study’s funnel plot to determine the degree of asymmetry. Egger regression test was calculated with P=0.34. A funnel plot and Egger test showed no evidence of publication bias. As shown in Figs. 3–6 [9–24], we established a forest plot and subgroup analysis to illustrate the significance among all studies included in our meta-analysis. We analyzed the 16 trials and established a random-effects model, resulting in an overall OR of 7.72 (95% confidence interval [CI], 6.01–9.93; P<0.001; I2=0%). The test for subgroup differences in Figs. 4 and 5 [9–24] indicated a statistically significant subgroup effect (P<0.05) for index hospitalization (OR, 8.67; 95% CI, 5.82–12.91), 30-day follow-up (OR, 7.32; 95% CI, 4.30–12.49), and in patients with a mean age of >60 years (OR, 7.75; 95% CI, 6.02–9.97). Mortality in COVID-19–positive patients with a mean age of <60 years showed an increase in one study, but this increase was not statistically significant (OR, 5.75; 95% CI, 0.46–72.30; P=0.18). As shown in Fig. 6 [13–15,17,23], the incidence of venous thromboembolism (VTE) was increased among COVID-19–positive patients (OR, 4.08; 95% CI, 1.23–13.58). According to these findings, COVID-19 positivity might increase the mortality rate and occurrence of thromboembolism in patients undergoing orthopedic surgery.
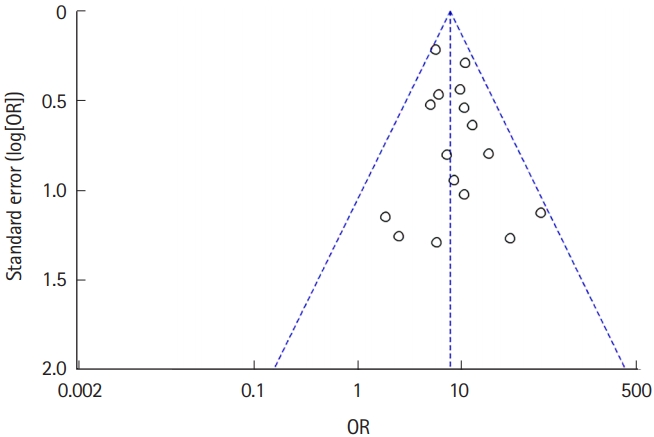
No publication bias is visible in the funnel plot of the selected studies. This figure displays the qualitatively evaluated asymmetry findings from each study. OR, odds ratio.

Forest plot of all the articles included in this study. M-H, Mantel-Haenszel test; Random, random-effects model; CI, confidence interval.

Postoperative mortality of (A) during index hospitalization and (B) 30-day follow-up. M-H, Mantel-Haenszel test; Random, random-effects model; CI, confidence interval.
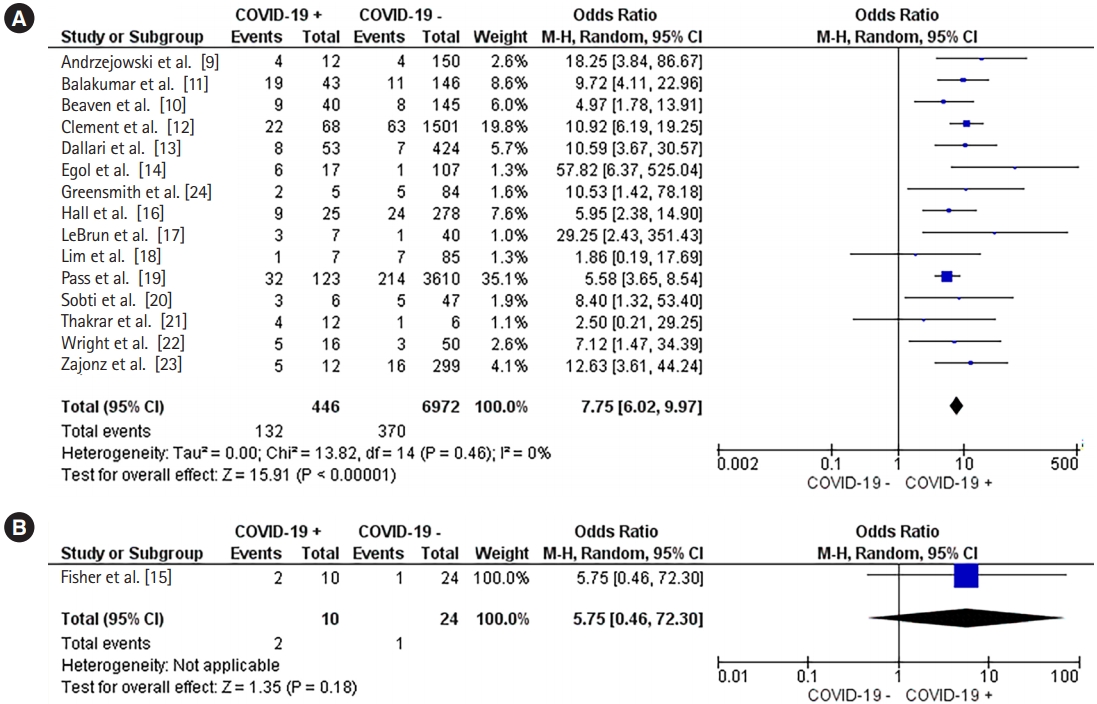
Postoperative mortality in the patients with a mean age of (A) >60 years and (B) <60 years. M-H, Mantel-Haenszel test; Random, random-effects model; CI, confidence interval.
DISCUSSION
This systematic review and meta-analysis looked at the death rate among COVID-19–positive and COVID-19–negative trauma patients undergoing orthopedic surgery. Most of the participants in this study were >60 years old. This finding is consistent with those of Atinga et al. [28], who found that geriatric trauma cases are increasing every year and now account for >25% of all significant trauma cases in the United Kingdom. Aging is associated with progressive physiological changes that affect various systems. Elderly people respond to trauma in a physiologically different manner than other people. Physiological responses in the elderly might vary due to co-occurring diseases, premorbid frailty, and prescribed drugs.
Previous research has linked hip fracture in the elderly to greater morbidity, a loss of autonomy in activities of daily living, a high rate of institutionalization, and mortality. Conservatively, mortality after hip fracture surgery is high in the first year, being approximately 30% of all cases [29–31]. In this study, 70 of the 134 patients with postoperative deaths among 456 COVID-19–positive patients who underwent orthopedic surgery had a hip or femur fracture.
According to Supplementary Table 4, the most commonly performed procedure in this study was hip arthroplasty. Haskel et al. [32] discovered that hip fracture volume in the elderly did not decrease during the lockdown period, even in areas severely affected by COVID-19 outbreaks. Age, a large waist circumference, a lower skeletal muscle index, bone mass density, vitamin D level, physical function, nutritional status, and cognitive function are linked to hip fractures in the elderly [33,34].
VTE involves both pulmonary embolism and deep vein thrombosis, respectively, and occurs in 0.6% to 1.5% of patients undergoing total joint arthroplasty. The risk factors for VTE are described by Virchow triad, which are venous stasis, endothelial damage, and a hypercoagulable state. VTE is typically the result of the interaction of two or less causes. Venous stasis can occur both during and after surgery due to intraoperative immobilization. Prolonged immobility raises the possibility of VTE development [35].
Previous research found that COVID-19–positive patients had a higher mortality rate during hip and femur fracture surgery [36–39]. Surgery within 48 hours of hospital admission does not correlate with a lower mortality rate in COVID-19–positive patients [13]. As shown in Table 3 [9–24], the mean hospital stay length among COVID-19–positive patients undergoing hip and femur surgery was longer than that among COVID-19–negative patients. This result is in line with the study by Kayani et al. [37], which stated that hip surgery in COVID-19–positive patients was associated with a longer hospital stay, longer immobilization, more hospitalizations in the intensive care unit, an increased chance of peri-operative complications, and greater mortality rates. COVID-19–positive patients with a smoking history and multiple (>3) significant comorbidities have a higher risk of death. Identifying factors that contribute to a higher death rate may improve prognostic classification and interdisciplinary perioperative care.
This review has some limitations. The majority GRADE rating in Table 1 was low because the evidence came from observational studies. Inaccurate studies with smaller sample sizes of COVID-19–positive patients may be influenced by chance. Of the 16 studies, only nine provided information about the type of surgery performed, eight reported the primary cause of postoperative death, and just one provided information about the type of anesthesia used in both groups. All of the included studies were conducted prior to the availability of COVID-19 vaccines.
In conclusion, the postoperative mortality rate among COVID-19–positive patients was 7.72 times greater than that of COVID-19–negative patients. Identifying risk factors for increased mortality may improve prognostic classification and perioperative interdisciplinary management. The findings of this study should be considered by the larger orthopedic community when developing guidelines for treating orthopedic trauma in specific populations in the COVID-19 era.
SUPPLEMENTARY MATERIAL
Supplementary materials are available at https://doi.org/10.15441/ceem.22.403.
Supplementary Table 1.
Joanna Briggs Institute risk of bias quality assessment for cohort studies
Supplementary Table 2.
Joanna Briggs Institute risk of bias quality assessment for cross-sectional studies
Supplementary Table 3.
Indications for orthopedic surgery during the COVID-19 pandemic
Supplementary Table 4.
The reported surgery in this study
Supplementary Material 1.
PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) checklist.
Notes
ETHICS STATEMENTS
Not applicable.
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
FUNDING
None.
AUTHOR CONTRIBUTIONS
Conceptualization: HDP; Formal analysis: VH, RP; Methodology: all authors; Project administration: HDP; Writing–original draft: HDP; Writing–review & editing: all authors. All authors read and approved the final manuscript.
References
Article information Continued
Notes
Capsule Summary
What is already known
During the COVID-19 pandemic, there was a decrease in emergency room visits for trauma and surgical interventions, particularly in traumatology services.
What is new in the current study
This study analyzes the most recent literature on postoperative mortality in trauma patients undergoing orthopedic surgery during the COVID-19 pandemic.